Intra-articular Fractures of the Distal Radius (AO types C3, with Special Focus in C3.3), Open Approach
20.1 Introduction
Severe intra-articular fractures of the distal radius with comminuted, displaced, and malrotated fragments combined with a metaphyseal comminution extending into the radial diaphysis are the most challenging fracture patterns. Reconstruction faces several major problems: fixation of cartilage-bearing fragments that are too small for stabilization by standard plates or screws, restoration of substantial cartilage loss in the articular surfaces, and extended metaphyseal/subchondral bony defects. Finally, there is a need for a secure fixation of the metaphysis. A strategy is reported to address these problems by using small, subchondrally placed Kirschner wires for the realignment of the articular surfaces, a temporary inlay of silicon foil in case of lost articular cartilage, and iliac crest bone grafting for bony defects. Stability is further augmented by a combined palmar and dorsal locking plating or bridge-plating of the radius.
In the treatment of intra-articular fractures of the distal radius, reconstruction of an articular surface without step-off or gap formation is an important aim. Several studies have demonstrated a distinct correlation between posttraumatic osteoarthritis and residual articular incongruity, addressing the outcome of displaced intra-articular distal radius fractures. On the basis of these results, there is a wide agreement not to accept a step-off or gap formation >1 to 2 mm.1,2 In clinical routine, however, these clinically and biomechanically well-established requirements are frustrated by considerable technical problems. Complex fragmentation of the articular surface of the distal radius, including deep impression of joint-bearing fragments, associated with a badly crushed metaphysis is a particularly challenging fracture pattern. Some of these cartilage-bearing fragments can be so small and thin that fixation by standard screws and plates is not possible. In addition, loss of articular cartilage and bone stock is frequently noted. Often, but not in all cases, the severe fragmentation of the articular surface of the distal radius is associated with severe comminution of the radial metaphysis with extension in the diaphysis of the radius. According to the AO/ASIF (Association for Osteosynthesis/Association for the Study of Internal Fixation) Comprehensive Classification of Fractures, this fracture pattern is classified as C3.3 fractures. According to the Fernandez classification, these fractures are categorized as type V fractures.
In the time before fixed-angle devices, the primary focus in the treatment of such complex intra-articular fractures of the distal radius was more avoidance of a secondary collapse of the metaphysis and less a meticulous reconstruction of the articular surface. For these reasons, external fixation maximally combined with limited open reduction was the treatment of choice, accepting residual gap formation and step-off of the joint surface.3–5 Some authors even recommend primary arthrodesis of the radiocarpal joint and the whole wrist joint.6,7 This situation has scarcely been changed by the introduction of fixed-angle implants. Nowadays locking plates specially designed for the distal radius allow secure fixation even if the metaphysis is severely comminuted, minimizing the risk of a secondary loss of reduction. This gives us the chance to focus much more on the restoration of the multifragmented articular surface of the distal radius.
These considerations lead to the question of how precisely the articular surface has to be restored. No one can really answer this question. There are patients with an exceptional clinical result and less pain despite severe damage to the articular surface of the radius. Others complain of permanent pain even at rest and severe deficits in their activities of daily living due to relatively mild degenerative changes of the radiocarpal joint. From a paper by Knirk and Jupiter2 we know that in young adults a persisting articular step-off of more than 2 mm will lead in 100% of cases to osteoarthritis of the radiocarpal joint. Jupiter is known to be no longer happy with this paper, believing that some of the patients had a scapholunate ligament tear that was not recognized at the time of surgery and that caused the degenerative changes. However, cadaveric studies showed a higher persisting step-off as more load transmitted from the hand to the distal radius becomes concentrated on the rim of the step-off, which may lead over time to osteoarthritis of the radiocarpal joint. With all of this controversial information in mind, and being convinced that a more anatomical reconstruction is related to a better clinical outcome, we try to restore the distal radius as anatomically as possible, with special focus on the articular surface.
While some authors prefer an arthroscopic approach to reconstruct the multifragmented articular surface of the distal radius, we favor an open approach for a number of reasons. Nearly all of these complex intra-articular fractures of the distal radius require plate fixation. Even if the articular surface is fixed arthroscopically, there is a need for an open approach. On the day of injury and in the first days after injury there is often a hematoma in the radiocarpal joint, making a good arthroscopic visualization of details difficult irrespective of whether a “dry” or “wet” arthroscopy is performed. Therefore, arthroscopic fracture treatment should not be carried out in the first days after the injury. Although on the day of injury the wrist is often not much swollen, some days later there is frequently significant swelling that makes the surgical procedure more demanding. In comparison, a hematoma in the radiocarpal joint can easily be removed using an open approach to the wrist joint at any time, allowing a clear visualization of the joint surface.
For simple intra-articular fractures of the distal radius we have found it helpful to analyze the fracture pattern using the 3-column concept outlined by Rikli and Regazzoni.23 But for complex intra-articular fractures we prefer the 5-column concept developed by Medolf from Hawaii and Pechlaner from Austria, which addresses not only the radial styloid and the intermediate column but also the central part of the articular surface as well as the palmar and dorsal rim of the radius.
For such sophisticated analysis of the fracture pattern, computed tomography (CT) of the distal radius is a sine qua non. In simple intra-articular fractures of the distal radius we prefer an arthro-CT to diagnose intracarpal lesions such as scapholunate ligament tears. For complex intra-articular fractures of the distal radius we favor a noncontrast CT scan with three-dimensional reconstruction for planning the surgical intervention. A CT scan of complex intra-articular fractures should show each fragment precisely, so that the surgeon can appreciate what fragments have to be addressed and how they can be fixed.
With respect to the articular surface, the CT scans are analyzed to answer the following questions: (1) Is the fracture located distal to the “watershed line”? (2) Is there an impression of the articular surface? (3) Are the fragments large enough for screw and plate fixation? (4) Is there a loss of cartilage? In addition, the CT scans are analyzed regarding metaphyseal comminution in terms of whether a stable fixation of the metaphysis can be achieved securely, avoiding a secondary collapse, or whether there is need for a long-lasting unloading of the metaphysis by bridge-plating.
The strategy for the reconstruction of these complex intra-articular fractures with comminution of the radial metaphysis and extension of the fracture in the diaphysis addresses four objectives:
Fixation of the smallest joint-bearing fragments that cannot be stabilized by standard implants.
Replacement of irreversibly lost articular cartilage.
Replacement of extended subchondral/metaphyseal bony defects.
Secure fixation of the metaphysis, and if that not possible, long-term unloading of the metaphysis.
For the solution, the following corresponding approach was adopted:
Fixation of the smallest fragments was achieved by thin subchondrally placed Kirschner wires that were countersunk in the bone.
In the case of defective articular cartilage, a silicon foil was temporarily implanted to induce cartilage-like regenerative tissue.
Subchondral/metaphyseal bony defects were filled using iliac crest bone grafts.
The comminuted metaphysis was stabilized by combined palmar and dorsal locking plating. In the case of extremely metaphyseal defect with extension of the fracture in the diaphysis, the metaphysis was unloaded by bridging the defect with a plate from the radial diaphysis to the third metacarpal.
The use of K-wires described here differs fundamentally from the technique of K-wire stabilization that is usually applied in distal radius fractures. The K-wires are much smaller and are placed subchondrally only for the adaptation of very small fragments. The K-wires are countersunk in the bone to avoid irritation of adjacent structures (see ▶ Fig. 20.1). This technique alone does not guarantee stable reduction. To avoid loss of reduction, additional stability is provided by one or several buttressing plates, and bone grafting. The application of silicon foils to induce a cartilage-like regenerative tissue for the treatment of cartilage loss of the articular surface in acute fracture of the distal radius has already been described by Stanković et al.8 The operative techniques for dorsal and palmar plate fixation of fractures of the distal part of the radius have been described in detail.9,10 Bridge-plating of the distal radius is a well-accepted treatment option for fractures of the distal radius with a severely comminuted metaphysis with no bone-to-bone contact either on the palmar or the dorsal aspect of the radius and extension of the fracture into the diaphysis.
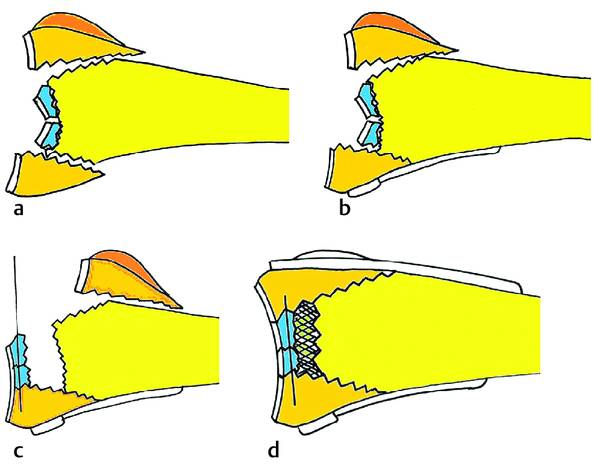
Fig. 20.1 (a–d) Schematic description of the strategy described with a palmar buttress plate using short screws distally, allowing dorsal manipulation of intra-articular fragments; subchondral K-wire fixation of tiny, cartilage-bearing fragments; iliac bone grafting of the subchondral-metaphyseal bone defect; and dorsal buttress plating of the radius.
20.2 Indications and Contraindications
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








