Intertrochanteric Hip Fractures: Intramedullary Hip Screws
Michael R. Baumgaertner
Sudeep Taksali
Indications/Contraindications
The number of hip fractures in the United States is estimated at 250,000 per year and will double by the year 2040. Fifty percent of hip fractures are intertrochanteric, of which 50% to 60% are classified as unstable. These fractures typically occur in elderly females, with 90% of fractures occurring in patients older than 65 years. The etiology of intertrochanteric hip fractures is typically attributed to low-energy falls in the setting of osteoporosis.
The stability of the intertrochanteric fracture drives both the treatment strategy and the surgical outcome. Unstable fractures have significant disruption of the posteromedial cortex, including subtrochanteric extension, or are reverse obliquity fractures. Stable two-part fractures, once reduced, will resist medial and compressive loads, whereas unstable fractures will have a tendency to collapse into varus.
Intramedullary hip screws (IMHS) are indicated for all unstable intertrochanteric hip fractures and are ideal for subtrochanteric and reverse obliquity fractures. An additional indication is an impending or pathologic fracture of the proximal femur. Multiple studies have indicated that the IMHS offers no advantage over a sliding hip screw and side plate in a stable fracture pattern. However, its utilization with stable fractures will provide a means to improve and streamline one’s technique when dealing with the more challenging unstable fracture patterns.
Contraindications to using an IMHS include all femoral neck fractures, deformities of the femoral shaft, and hip ankylosis. An additional contraindication is the young patient because an excessive amount of trabecular bone is removed from the trochanteric block to accommodate these relatively large implants.
The IMHS combines a sliding hip screw with an intramedullary nail. Implant insertion can be performed in a closed, percutaneous manner, allowing minimal surgical insult to the fracture zone and reduced perioperative blood loss. The device functions as an
intramedullary buttress, effectively reestablishing the mechanical support of the posteromedial cortex and thus preventing excessive shaft medialization. By avoiding violation of the fracture zone, the surgeon facilitates fracture union.
intramedullary buttress, effectively reestablishing the mechanical support of the posteromedial cortex and thus preventing excessive shaft medialization. By avoiding violation of the fracture zone, the surgeon facilitates fracture union.
Preoperative Planning
Elderly patients will typically present after a fall with the affected limb shortened and externally rotated. It is important to obtain a thorough medical and social history as well as determine if the patient has an oncologic history. It is equally important that a complete physical examination is performed with care to examine the condition of the skin overlying the hip and to rule out any associated injuries.
The diagnosis of an intertrochanteric hip fracture is generally confirmed with standard anteroposterior (AP) and lateral radiographs. These radiographs should include at least the proximal half of the femur because deformities of the shaft may preclude the use of an intramedullary device. Internal rotation and traction radiographs can further aid in understanding the pathoanatomy.
Close perioperative medical management of patients with intertrochanteric hip fractures is critical to obtaining a successful postoperative outcome because the patient population is medically complex. Some issues of particular importance are the patient’s nutritional status, management of urinary tract infections, hemodynamic stability, coagulopathy, deep vein thrombosis (DVT) prophylaxis, and perioperative antibiotics. Typically, optimization should not be prolonged, as mortality is increased when surgery is delayed beyond 48 to 72 hours from admission.
Careful examination of the preoperative radiographs as well as the unaffected hip will help guide appropriate implant selection with respect to the neck angle, diameter, and screw length. We typically use a 135-degree neck angle with a 95-mm lag screw. It is important to note that the IMHS is not designed to fill the canal. A long stem device should be considered in the setting of a pathologic fracture or fractures with significant subtrochanteric extension.
Surgical Technique
We generally use a fracture table and position the patient supine (Fig. 17.1A). A well-padded post is placed in the perineum. The affected side is secured to the traction assembly. We prefer to use the heel stirrup and metatarsal bar as opposed to putting the foot in the Velcro-strapped boot. The heel and the forefoot are cushioned with an ABD pad, and heavy cloth tape is used to secure the foot to the stirrup (Fig. 17.1B). By locking the transverse tarsal joint and dorsiflexing the ankle, we gain greater control over the extremity for firm traction and internal/external rotation. The affected extremity is adducted with the torso shifted away from the surgical side. The unaffected extremity can be placed in the well leg holder with the knee flexed and the hip flexed and internally rotated. This allows for unhindered access for the image intensifier so that lateral radiographs of the fracture zone can be obtained (Fig. 17.1C). Unfortunately, this visualization may occasionally come at a price: There is no countertraction on the well leg. As a result, when strong traction is applied to the fracture, the pelvis has a tendency to rotate around the perineal post. This produces abduction of the operative side and can significantly hamper achieving the correct starting point, leading to a varus reduction (Fig. 17.2).
An alternate method of positioning the patient allows countertraction on the pelvis by placing both extremities parallel in foot traction. The extremities are “scissored,” with the operative side slightly flexed at the hip and the well side extended to allow for lateral plane fluoroscopic imaging (Fig. 17.3).
Once the patient has been appropriately positioned on the table, the extremity is manipulated. The primary goal is to gain access to the starting point; secondarily, we attempt fracture reduction. Most stable fracture patterns will reduce with axial traction and internal
rotation of the femur. However, unstable intertrochanteric hip fractures may require different maneuvers, such as slight external rotation. Prior to draping the field, we confirm that we can see the following areas via fluoroscopy: the anterior cortex of the proximal femur, the fracture zone, the anterior neck, the entire circumference of the femoral head, the posterior neck, and the trochanter.
rotation of the femur. However, unstable intertrochanteric hip fractures may require different maneuvers, such as slight external rotation. Prior to draping the field, we confirm that we can see the following areas via fluoroscopy: the anterior cortex of the proximal femur, the fracture zone, the anterior neck, the entire circumference of the femoral head, the posterior neck, and the trochanter.
In considering an ideal reduction, we determine an acceptable neck-shaft angle to be 130 to 145 degrees. More valgus is allowed because it reduces the bending forces on the implant and may offset the limb shortening that occurs with fragment impaction. Angulation greater than 15 degrees, as seen on the lateral view, is unacceptable.
Once a provisional reduction has been attempted, skin surfaces should be prepped in standard sterile fashion. Care should be taken to prep to the level of the knee in the event that a long nail is used such that a distal interlocking screw can be placed. We use a sterile shower-curtain type drape but add an extra sterile layer proximally to protect against puncture hole contamination from the instrumentation.
Before incision, the tip of the trochanter and the femoral shaft axis are marked in both planes with the skin marker (Fig. 17.4). This provides a visual aid for the correct insertion
of the guide pin and the IMHS. In addition, this helps reduce fluoroscreening time. Typically, prior to skin incision, the implant and insertion jig are preassembled per the preoperative plan. It is very helpful to insert and partially advance the set-screw that locks the nail to the sleeve prior to implantation because later it is often difficult to place through the percutaneous wound (Fig. 17.5).
of the guide pin and the IMHS. In addition, this helps reduce fluoroscreening time. Typically, prior to skin incision, the implant and insertion jig are preassembled per the preoperative plan. It is very helpful to insert and partially advance the set-screw that locks the nail to the sleeve prior to implantation because later it is often difficult to place through the percutaneous wound (Fig. 17.5).
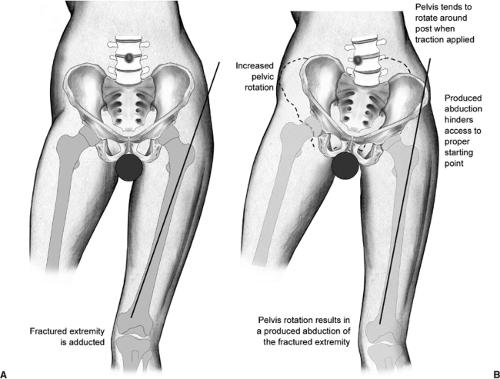 Figure 17.2. With the application of unopposed traction, the pelvis rotates around the perineal post. The hip abducts, hampering access to the starting point. |
 Figure 17.3. Alternate method of positioning with the legs scissored. This position provides countertraction on the pelvis and still allows for lateral plane imaging. |
Prior to creating the entrance channel, the reduction should be verified with bi-planar imaging. Using a freehand technique, we insert a 3.2-mm guide pin percutaneously (Fig. 17.6), about 3 to 4 cm proximal to the trochanter, engaging the bone at or just medial to the tip of the greater trochanter. This location will counteract the tendency toward varus and increased neck-shaft offset as well as minimize any damage to the gluteus medius insertion (Fig. 17.7




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree










