Intertrochanteric Fractures: Use of a Sliding Hip Screw
Kenneth J. Koval
Indications/Contraindications
The primary goal of fracture treatment is to return the patient to his/her prefracture level of function. There is general agreement that in the patient who sustains an intertrochanteric hip fracture, this can best be accomplished through surgery. Nonoperative management is appropriate only in nonambulators, often with multiple medical co-morbidities, who experience minimal discomfort from the injury. Occasionally, younger healthy patients who have a completely nondisplaced intertrochanteric fracture can be managed nonoperatively; however, these patients must be closely followed to detect evidence of fracture displacement. All patients treated nonoperatively should be rapidly mobilized to avoid the complications of prolonged recumbency, such as decubitus, deep venous thrombosis (DVT), aspiration, and the like.
Numerous authors have proposed classification schemes for intertrochanteric fractures; however, the most important aspect of any classification is the determination of fracture stability. Stability is provided by the presence of an intact posteromedial cortical buttress. Unstable fracture patterns include those with loss of the posteromedial buttress, fractures with subtrochanteric extension, and reverse obliquity fractures.
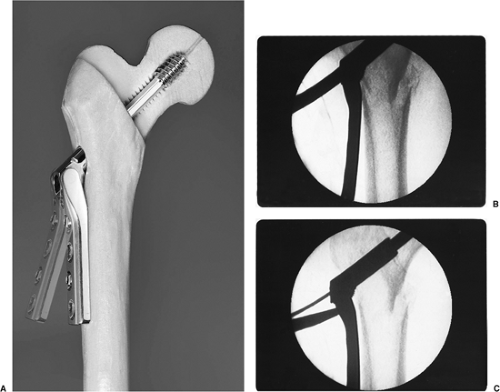
I currently use a sliding hip screw with a two-hole side plate for stable intertrochanteric hip fractures and an intramedullary nail for unstable fracture patterns, particularly in younger individuals. Following fixation of intertrochanteric fractures with a stable fracture pattern, there should be minimal fracture settling, limb shortening, or medialization of the distal fragment. I prefer a variable angle hip screw (VHS) (EBI, Parsippany, NJ) because it allows some adjustment of the fracture alignment once the screw and plate assembly has been implanted (Fig. 16.1). The use of this implant also helps with inventory control as a single plate can allow a range of plate angles, from 89 to 159 degrees. For unstable fracture patterns, I prefer use of an intramedullary hip screw (IMHS) device because it prevents excessive fracture collapse and deformity. The lag screw portion of the intramedullary devices can telescope within the nail only until the femoral head and neck segment abuts the intramedullary nail.
Preoperative Planning
The range of clinical deformity of the involved lower extremity varies depending on fracture displacement and comminution. Nondisplaced fractures may present with virtually no clinical deformity, while displaced fractures present with the classic shortened and externally rotated extremity. Range of motion of the hip can be painful and should be avoided. Neurovascular injuries are rare, but a careful evaluation should be performed. Hip fractures following high-energy trauma require a careful work-up to rule out the possibility of associated injuries.
Standard radiographic examination for patients with suspected hip fractures include an anteroposterior (AP) view of the pelvis, and an AP and cross-table lateral of the injured proximal femur (Fig. 16.2). A cross-table lateral radiograph is necessary to evaluate the posteromedial cortex for signs of comminution. In situations where the fracture geometry is not clear due to deformity, an AP view of the hip internally rotated 15 to 20 degrees may be helpful (Fig. 16.3). An AP view of the contralateral side is helpful, particularly as a means of assessing the size and angle of the implant for intramedullary fixation.
Surgery
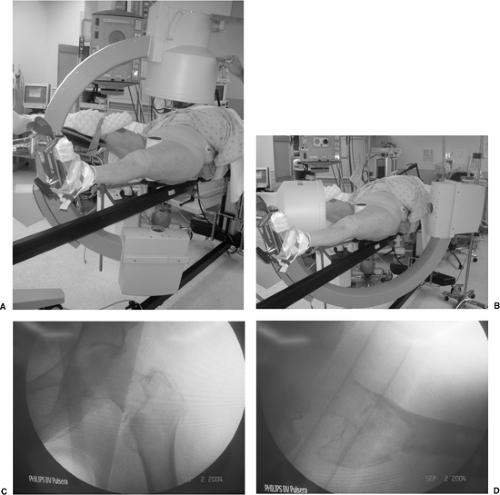
Following satisfactory general or spinal anesthesia, the patient is positioned supine on a fracture table, with care taken to pad and protect the labia or scrotum against the peroneal post. Once the patient is properly positioned, a mobile c-arm intensifier is positioned to allow visualization of the hip in AP and lateral planes. Most intertrochanteric hip fractures can be reduced using gentle longitudinal traction with the leg externally rotated followed by varying degrees of internal rotation. The uninvolved leg must be positioned so that it does not block positioning of the image intensifier for a lateral view (Fig. 16.4).
The surgeon must confirm satisfactory fracture reduction before prepping the patient and be certain that nonobstructive, biplanar, radiographic visualization of the entire proximal femur, including the hip joint, is obtainable (Fig. 16.5). Inadequate visualization of the entire proximal femur can result in technical errors, such as inappropriate lag screw
positioning or length. Varus angulation often results in guide pin positioning in the inferior femoral neck and superior femoral head. The surgeon must be prepared to deal with residual varus angulation, posterior sag, or malrotation. Varus angulation can usually be corrected by placing additional traction on the lower extremity to disengage the fracture fragments. Occasionally, one may need to abduct the lower extremity to correct a varus malreduction. If residual varus remains, one should check the position of the fracture fragments on the lateral radiographic view, as posterior sag may prevent adequate fracture reduction. In this situation, traction should be released and the fracture manipulated to disengage the fragments. Attempting fracture fixation with varus angulation or posterior sag can lead to difficulty centering the lag screw in the femoral head.
positioning or length. Varus angulation often results in guide pin positioning in the inferior femoral neck and superior femoral head. The surgeon must be prepared to deal with residual varus angulation, posterior sag, or malrotation. Varus angulation can usually be corrected by placing additional traction on the lower extremity to disengage the fracture fragments. Occasionally, one may need to abduct the lower extremity to correct a varus malreduction. If residual varus remains, one should check the position of the fracture fragments on the lateral radiographic view, as posterior sag may prevent adequate fracture reduction. In this situation, traction should be released and the fracture manipulated to disengage the fragments. Attempting fracture fixation with varus angulation or posterior sag can lead to difficulty centering the lag screw in the femoral head.
 Figure 16.3. Use of internal rotation with gentle traction to evaluate a right, proximal, femur fracture. |
 Figure 16.4. Patient positioning for stabilization of a left intertrochanteric fracture with the uninvolved leg flexed, abducted, and externally rotated. |
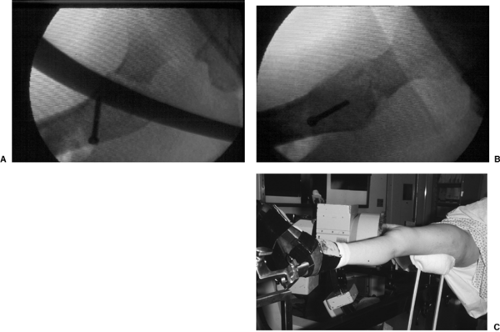 Figure 16.6. A. Posterior sag after intertrochanteric fracture reduction can be corrected with use of a (B,C) crutch placed under the proximal thigh. |
Posterior sag requires manual correction using a crutch, bone hook, or periosteal elevator (Fig. 16.6). If unrecognized, posterior sag can result in guide pin positioning in the anterior femoral neck and posterior femoral head. After a satisfactory reduction has been achieved, I rotate the lower extremity under fluoroscopy to determine whether the fracture fragments move as a single unit. In those patients where the femoral shaft moves independently of the proximal fragment, excessive internal rotation of the leg should be suspected. In these cases, the lower extremity should be placed in neutral or slightly external rotation. Once the fracture is fully reduced, the patient is prepped and draped.
Approach and Implant Insertion
A straight lateral incision is made starting just distal to the greater trochanter and extending distally in line with the femoral shaft (Fig. 16.7). The length of the incision depends upon the patient’s size. The iliotibial band is exposed and incised in line with its fibers (Fig. 16.8). The vastus lateralis is elevated from the intermuscular septum and the lateral aspect




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree