Intertrochanteric Fracture Fixation Using a Sliding Hip Screw or Cephalomedullary Nail
Patient Selection
Approximately 340,000 patients sustain hip fractures in the United States each year
Intertrochanteric fractures are extracapsular hip fractures occurring primarily in elderly patients or those with osteopenia or osteoporosis
Indications
Surgical treatment is standard of care for hip fractures
Nonsurgical management can lead to fracture displacement, pain, inability to transfer, decubitus ulcers, pulmonary complications, urinary tract infections, and deep vein thrombosis (DVT)
Contraindications
Elderly patients with dementia who have minimal pain and were nonambulatory before fracture
Rarely, patients with severe medical comorbidities precluding safe surgical intervention
Preoperative Imaging
Radiography
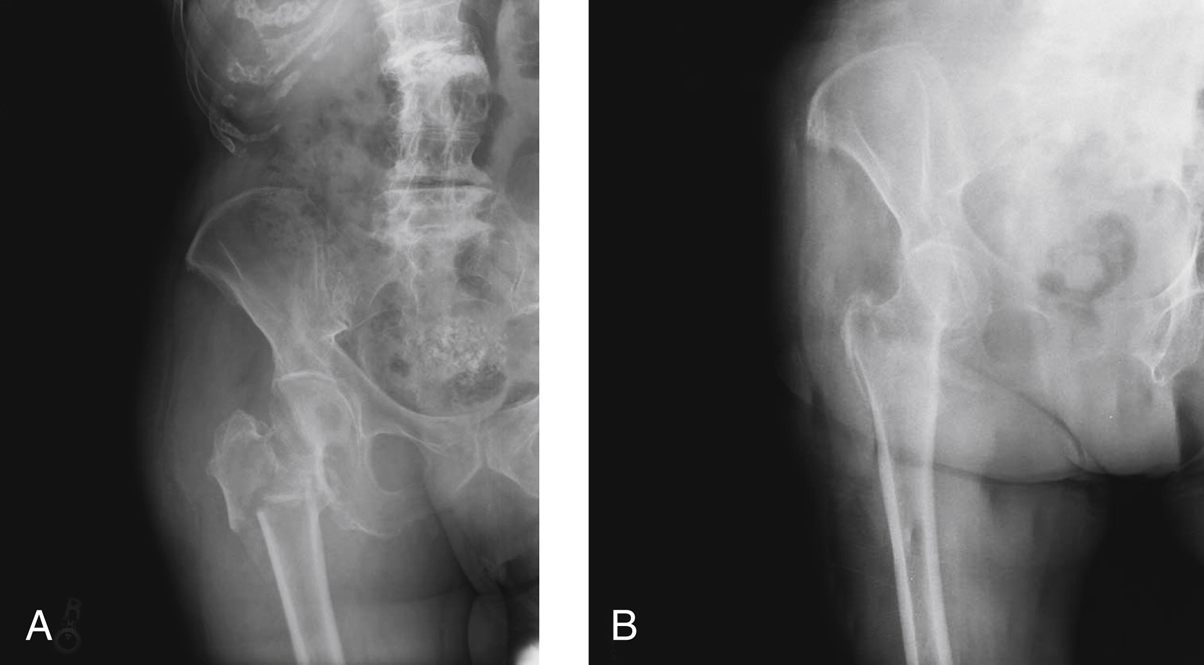
Figure 1Radiographs demonstrate a comminuted proximal femur fracture. A, AP view of the hip. B, AP view obtained with the lower extremity in manual traction and internal rotation. The alignment of the hip with traction enables better understanding of the fracture pattern and its behavior with closed reduction.
Good plain radiographs fully characterize fracture and enable appropriate treatment
AP pelvis and AP and lateral hip views
AP view with 15° internal rotation and gentle traction helps delineate fracture pattern (Figure 1)
Cross-table lateral is preferred; frog-lateral uncomfortable for patient
Two percent to ten percent of patients have negative radiographs; further imaging needed if history and examination consistent with fracture
CT scan or MRI are additional modalities commonly used
Bone scan was historically used when radiographs were negative for fracture, but it may not show positive results for up to 72 hours; may not accurately depict fracture pattern
Magnetic Resonance Imaging
More sensitive than CT
Completely characterizes anatomy of fracture
Improves diagnostic speed compared with CT and bone scan
Expensive and less available than CT
Procedure

Figure 2AP radiograph of the hip demonstrates an intertrochanteric fracture treated with a sliding hip screw. Excessive collapse has occurred because of a previously unrecognized lateral wall fracture.
Can treat standard obliquity intertrochanteric fractures with sliding hip screw (SHS) or cephalomedullary nail (CMN)
Despite regional variations and surgeon preferences, SHS considered standard treatment; CMN has higher rate of peri-implant fracture at nail tip
No differences in blood loss, surgical time, or recovery
Use CMN in treatment of reverse obliquity fractures, intertrochanteric fractures with lateral wall involvement, transverse intertrochanteric fractures, and fractures with subtrochanteric extension; SHS has high rate of failure due to excessive collapse (Figure 2)
Room Setup/Patient Positioning

Figure 3Photograph demonstrates typical setup and patient positioning on a fracture table for surgical fixation of an intertrochanteric fracture using an intramedullary (IM) nail. Note the proximal and posterior extent of draping required for IM nail fixation and the intraoperative use of a compression device on bilateral lower extremities.
Supine position; fracture table enables easy biplanar imaging and maintains reduction
Obtain reduction before incision; ensure C-arm can obtain AP and lateral images
Use boot traction; pad all bony prominences well on both legs, including perineal post
Scissor legs; surgical leg flexed, nonsurgical leg extended; avoid hyperextension and excessive traction on femoral nerve of nonsurgical leg
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


