Innominate Osteotomy of Salter
Simon P. Kelley
John H. Wedge
DEFINITION
The Salter innominate osteotomy is commonly performed in conjunction with an open reduction for the dislocated hip in developmental dysplasia of the hip (DDH) after 18 months of age.
The osteotomy can also be performed to treat acetabular dysplasia in the child with a concentrically reduced hip.6
ANATOMY
The Salter innominate osteotomy rotates through the symphysis pubis to increase anterior and lateral coverage of the femoral head.
The center of the hip undergoes slight distal, posterior, and medial displacement in addition to rotation.4
A 30-degree bone wedge inserted in the osteotomy site consistently increases femoral head coverage by 25 degrees anteriorly and 15 degrees laterally.4
PATHOGENESIS
Acetabular dysplasia is caused by the following:
Lack of a reduced, spherical head within the growing acetabulum
Abnormal interstitial or appositional growth within the acetabular and triradiate cartilage
Abnormal development of the secondary centers of ossification of the ilium, pubis, and ischium
In the developmentally dislocated hip, the acetabular labrum is flattened, hypertrophied, everted, and is referred to as the Limbus.
Acetabular dysplasia in the infant and young child with DDH is predominantly anterior and lateral.7
NATURAL HISTORY
The natural history of the dysplastic hip with subluxation is worse than the hip with acetabular dysplasia alone.
Patients with subluxated dysplastic hips develop pain and disability and radiographic evidence of osteoarthrosis. The age of onset of symptoms depends on the degree of subluxation, with severe subluxation leading to symptoms in the third decade of life.10
Patients with acetabular dysplasia without subluxation develop radiographic evidence of osteoarthrosis in the sixth decade of life and some will develop pain and disability, depending on the degree of dysplasia.10
PATIENT HISTORY AND PHYSICAL FINDINGS
Patients with developmental hip dislocation may have a positive family history and are usually female and firstborn children.
There may be a history of breech presentation at birth.
Children with a dislocated hip usually meet their gross motor milestones within the appropriate timeframe.
In children with bilateral dislocations, walking is frequently delayed until 16 to 18 months.
The pertinent physical examination findings in the walking child (the timeframe when this operation is typically performed) are listed in the following text.
Gluteus medius lurch: Trunk lean over the stance phase leg signifies a positive test, which is a nonspecific sign of hip pathology caused by dislocation, coxa vara, or painful hip conditions.
Trendelenburg sign: If the pelvis dips away from the affected leg during single-limb stance, the test is positive. Like the gluteus medius lurch, a positive test is a nonspecific sign of hip pathology caused by dislocation, coxa vara, or painful hip conditions.
Galeazzi sign: Knees at different levels signify a positive test, which indicates unilateral hip dislocation or congenital shortening of the femur.
Limitation of hip abduction: Normal abduction range of motion is 70 to 80 degrees tested in flexion in the newborn and infant. Asymmetric abduction suggests unilateral hip dysplasia, subluxation, or dislocation. Bilaterally decreased abduction suggests bilateral disease.
Hamstring tightness test: Normally, the hamstrings will tighten with passive knee extension, and no knee hyperextension should be possible. A positive test implies hip dislocation or flaccid paralysis of the hamstring muscles.
Inspection of inguinal skin folds: Normal inguinal skin folds are symmetric and stop short of the anal aperture posteriorly. Asymmetric skin folds are a relatively nonspecific finding in the dislocated hip.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Standing anteroposterior (AP), supine frog-leg lateral, supine abduction-internal rotation view, and standing false-profile view pelvic radiographs may be used.
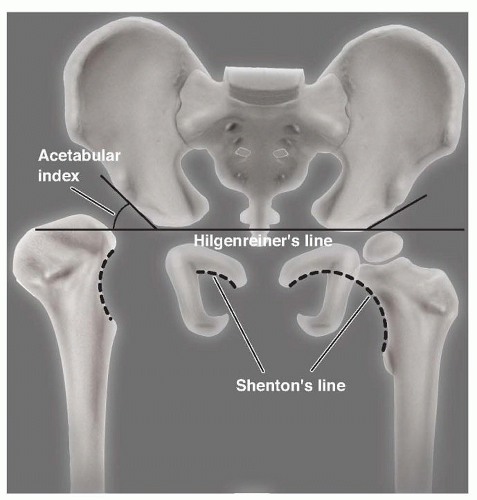
On the AP film, the acetabular index should be measured to diagnose acetabular dysplasia. Normal values are 35 degrees at birth, 25 degrees at 1 year of age, and 20 degrees at 2 years of age (FIG 1).8
Also on the AP film, Shenton line is inspected for discontinuity, which represents hip subluxation (see FIG 1).
Widening of the acetabular teardrop can be seen with persistent acetabular subluxation due to inadequate loading of the medial acetabular wall.
A false-profile view of the hip can identify more subtle cases of acetabular dysplasia, particularly in the walking child.
The abduction-internal rotation view demonstrates the likely position of correction following Salter innominate osteotomy.
Advanced imaging studies (three-dimensional [3-D] computed tomography [CT] scanning of the acetabulum, magnetic resonance imaging [MRI] of the hip) may be of value in older children to assess acetabular morphology.
DIFFERENTIAL DIAGNOSIS
Congenital femoral deficiency
Developmental coxa vara
Legg-Calvé-Perthes disease
NONOPERATIVE MANAGEMENT
The acetabular index should be observed for improvement over 12 to 18 months after successful closed reduction in the child younger than 18 months of age.
Indications for a Salter innominate osteotomy include residual acetabular dysplasia with an increased acetabular index, widening of the acetabular teardrop, a broken Shenton line, and adductor tightness on clinical examination.
A child younger than 18 months old who fails closed reduction can be treated with an isolated open reduction of a dislocated hip and observed for improvement in the acetabular index into the normal range over 12 to 18 months. Salter innominate osteotomy is only indicated as per the criteria stated earlier.
SURGICAL MANAGEMENT
Indications
Age 18 months to 9 years5
Concentric hip reduction on an abduction-internal rotation radiograph (either preoperatively or intraoperatively after an open reduction)5
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree