Fig. 10.1
Topographic classification of the flexor tendons according to Verdan and Michon
10.1.1.1 The Long Fingers
Zone 1
Located below the distal insertion of the flexor digitorum superficialis, it is the area of the distal insertion of the flexor digitorum profundus. It is one of the areas where the tendon is poorly vascularized, which makes its healing longer and random in case of injury.
Zone 2
Starts at the entrance of the digital sheath and ends at the medium part of the 2nd phalanx (lower than the 2 tendon strips of the flexor digitorum superficialis).
This zone used to be called the “no man’s land” by Bunnel, because it seemed impossible to repair the injuries that occurred there. The injuries in that zone are still the most complex to treat.
The 2 flexors divide the digital canal, made up of the periosteum and the palmar ligaments of the metacarpophalangeal and proximal interphalangeal joint from behind and the annular ligaments and cruciate pulleys in the front (Fig. 10.2).
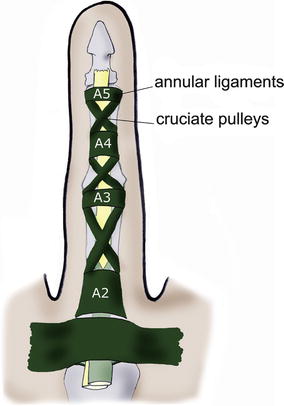
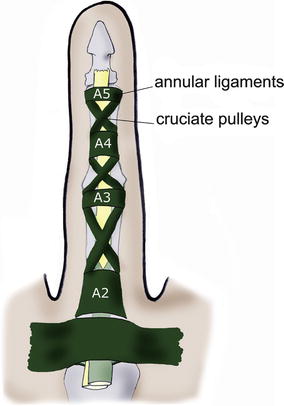
Fig. 10.2
Location of the annular ligaments and cruciate pulleys
The aim of these pulleys and annular ligaments is to maintain the flexors against the bone levers, thus permitting the complete finger winding and avoiding the bowstring effect.
Lastly, the flexor digitorum superficialis splits into two strips near the base of the 1st phalanx, to let the flexor digitorum profundus pass. Below this chiasma, the flexor digitorum profundus becomes superficial and the flexor digitorum superficialis becomes deep (Fig. 10.3).
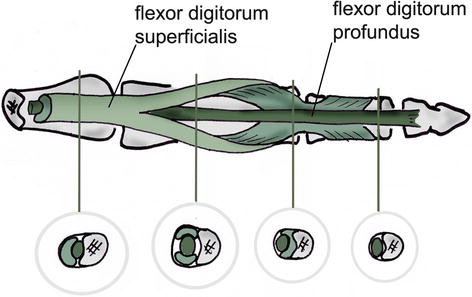
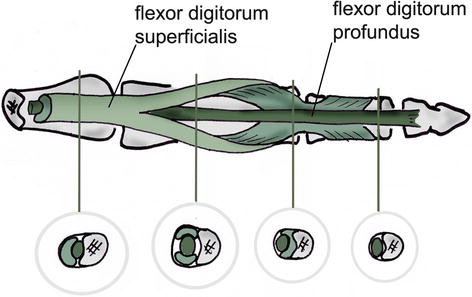
Fig. 10.3
Flexor digitorum superficialis’ chiasma (area of frequent adherences) – according to Kapandji
Zone 3
Situated between the distal part of the flexor retinaculum (or transverse carpal ligament) and the entrance of the digital sheath.
Zone 4
Corresponds to the carpal tunnel where the flexor retinaculum acts as the first pulley for the flexor system.
Zone 5
Located between the musculotendinous junction proximally (inferior 1/3 of the forearm) and the proximal part of the flexor retinaculum.
10.1.1.2 The Thumb
The only extrinsic muscle that makes the flexion of the thumb is the flexor pollicis longus.
The T1 zone corresponds to the ending of the flexor pollicis longus, and the T2 zone is between the A1 pulley and the proximal part of the A2 pulley. The T3 zone is located at the level of the thenar eminence (possible area of adherences with the 2 heads of the flexor pollicis brevis) (Fig. 10.4). Zones 4 and 5 are the same than for the long fingers.
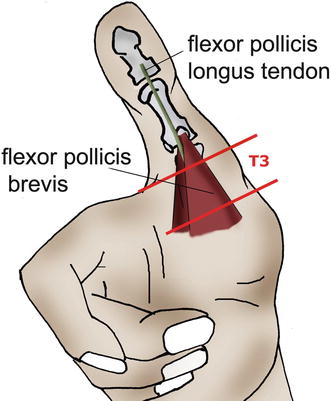
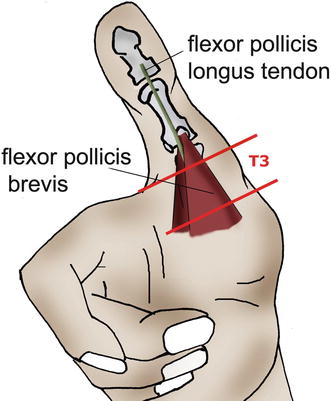
Fig. 10.4
Trajectory of the flexor pollicis longus between the 2 heads of the flexor pollicis brevis
10.1.2 The Pulleys [1]
They are fibrous bands maintaining the flexor system in contact with the skeleton and therefore avoiding the bowstring effect (Fig. 10.5).
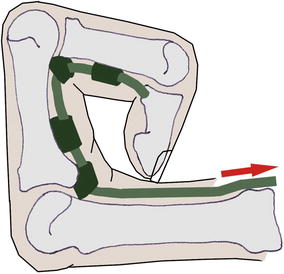
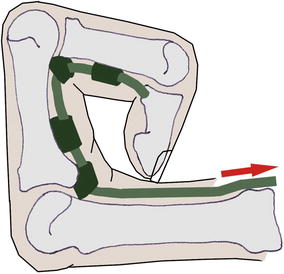
Fig. 10.5
The pulleys keep the flexor tendons against the skeleton to avoid the bowstring effect
There are 5 annular ligaments and 3 cruciate pulleys at the digital level, to which must be added the flexor retinaculum at the level of the carpal tunnel (Fig. 10.6).
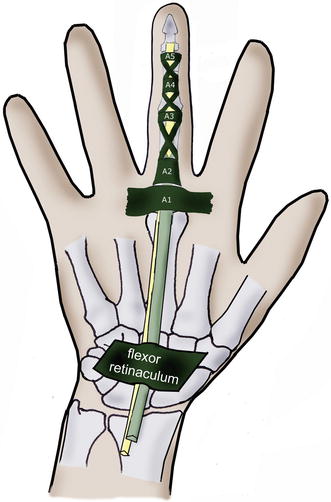
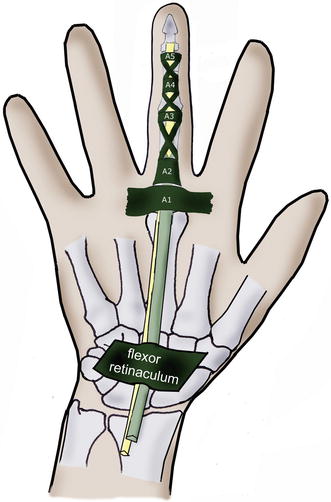
Fig. 10.6
The flexor retinaculum participates in the action of the digital pulleys
They are essential for winding the fingers, especially the A2 and A4 pulleys. Their isolated tear is in fact enough to lower the mobility (Fig. 10.7).
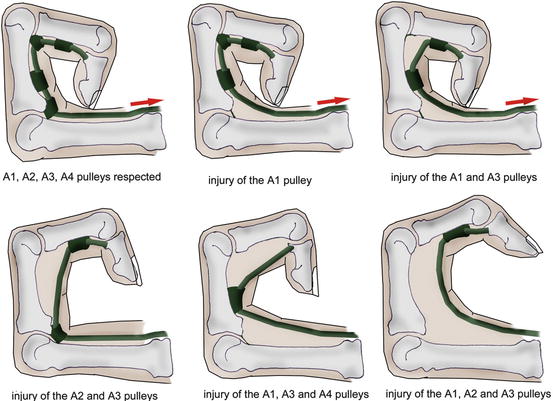
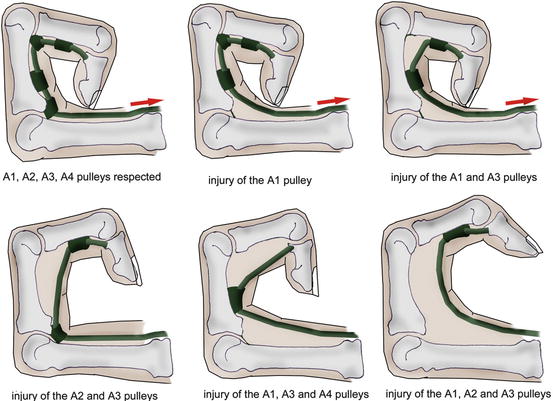
Fig. 10.7
The integrity of the annular ligaments, A2 and A4 in particular, is essential in the complete fingers winding
10.1.3 Nutrition of the Flexor Tendons
It depends on 2 complementary systems:
10.1.3.1 The Vascular System
Outside the digital sheath: the flexor tendons are vascularized from their 2 endings (periosteum and musculotendinous junction) and by the intratendinous vascular system for the areas far from the extremities of the tendon.
The paratendon, surrounding the tendon, sends a structure to carry the vessels (the mesotendon) which enters the tendon, allowing its vascularization.
Inside the digital sheath: the mesotendon condenses to form the vincula, supplied by anastomosis with the collateral arteries.
The 2 flexors each have 2 vincula, a short one near their ending and a long one higher, which infuse their dorsal part.
There still are 3 areas that are badly vascularized, in front of the A2 and A4 pulleys. The first one is proximal to the flexor digitorum superficialis’ chiasma, and the 2 others are above and below the vinculum longus that approaches the flexor digitorum profundus at the level of the proximal interphalangeal joint (Fig. 10.8).
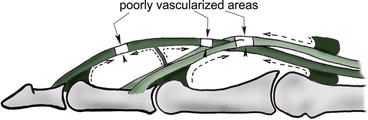
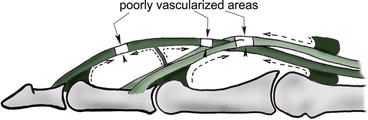
Fig. 10.8
Vincula system, participating in the vascularization of the flexor system but leaving some avascular areas
10.1.3.2 The Synovial Pump [2]
The synovial sheaths have different organizations, depending on the finger (Fig. 10.9a). The flexor pollicis longus has its own sheath, from zone 4 to the T1 zone.
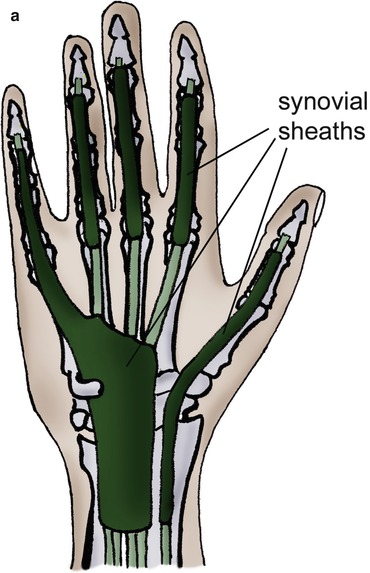
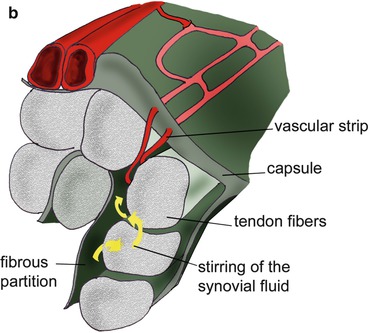
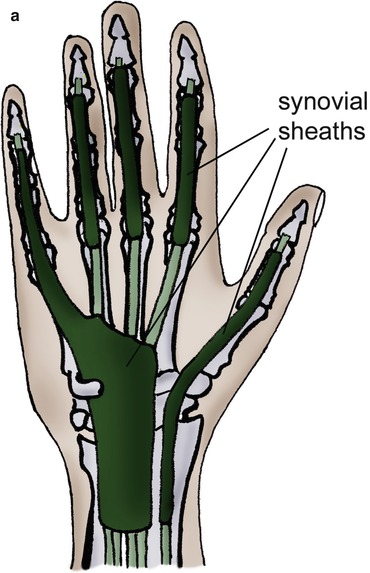
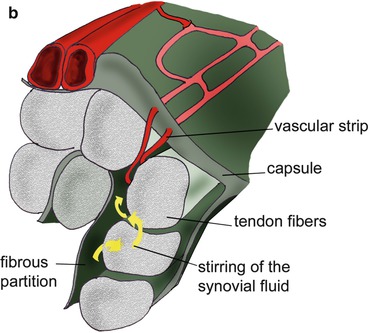
Fig. 10.9
(a) Topography of the synovial sheaths. (b) Nutrition of the tendon by stirring the synovial fluid or synovial pump
The index, middle and ring fingers share a sheath with the little finger in zone 4. They each have their individual sheath in the digital canal. The little finger’s sheath, shared with the other long fingers, continues until the digital canal.
The synovial fluid in the sheaths plays an important role of lubrication and nutrition, by soaking the tendons in the digital canal (Fig. 10.9b).
It is important to note that, in the digital canal, the nutrition of the flexor digitorum superficialis is twice as important through this method as through the vascular system and 5 times more important for the flexor digitorum profundus.
Thanks to these 2 systems, we obtain the healing of the tendon by extrinsic healing (vascular mechanism) and intrinsic healing (synovial pump).
The extrinsic healing corresponds to a fibroblastic invasion, which causes adherences. On the other hand, the intrinsic healing is related to a phenomenon of synovial imbibition that doesn’t create adherences.
A surgery as atraumatic as possible and an immediate active rehabilitation favour the intrinsic healing, providing a better functional recovery.
10.1.4 Lag Time
The lag time is the decrease of the resistance of the sutured tendon until the 5th postoperative day and then the improvement of this resistance until it reaches the immediate postoperative resistance on the 15th day.
This phenomenon can only be observed in case of postoperative immobilizations and doesn’t exist in the active protocols.
10.1.5 The Quadriga Effect
Forcing the extension of 3 long fingers leads to a “blocking” of the free finger, which can mobilize the proximal interphalangeal joint in flexion but not the distal interphalangeal joint (Fig. 10.10).


Fig. 10.10
The quadriga effect; it is impossible to flex the distal interphalangeal joint in one finger if the others are maintained in extension, because the flexor digitorum profundus is the same for all the long fingers and the proper tendons of each finger become separated very distally
This phenomenon can be explained by the fact that the flexor digitorum superficialis tendons are very well individualized in the forearm, whereas the flexor digitorum profundus tendons are individualized only in the hand, thus preventing (or limiting) their isolated contraction.
10.1.6 Winding Dynamic and Tendon Gliding
From an analytic point of view, the role of each tendon during the finger flexion is well known and defined:
Flexion of the distal interphalangeal joint produced by the flexor digitorum profundus
Flexion of the proximal interphalangeal joint produced by the flexor digitorum superficialis
Flexion of the metacarpophalangeal joint produced by the interossei through the dorsal expansion
The finger winding starts with the proximal interphalangeal joint which unlocks the distal interphalangeal joint by relaxing the lateral strips, putting in tension the median strip and relaxing the retinacular ligament.
The distal gliding of the extensor system, during this phase, puts in tension the interossei and the lumbrical muscles, which start a flexion of the metacarpophalangeal joint due to the tenodesis effect (related to the slant path of these tendons).
The flexion of the metacarpophalangeal joint moves the dorsal expansion of the interossei distally, in an efficient position to produce a flexion of the first phalanx (when the metacarpophalangeal joint is extended, the contraction of the interossei leads to an extension of the interphalangeal joints) (Fig. 10.11).
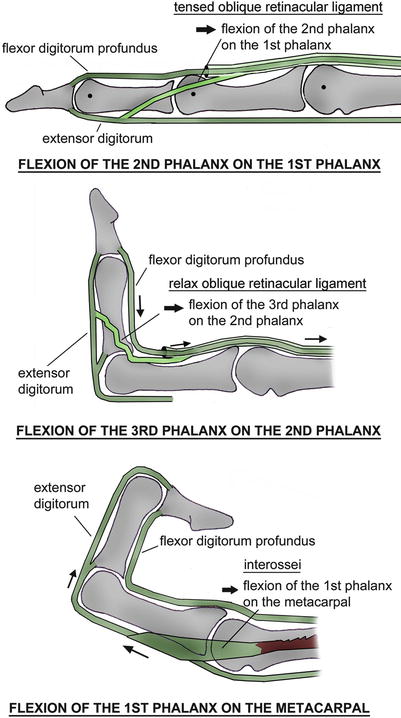
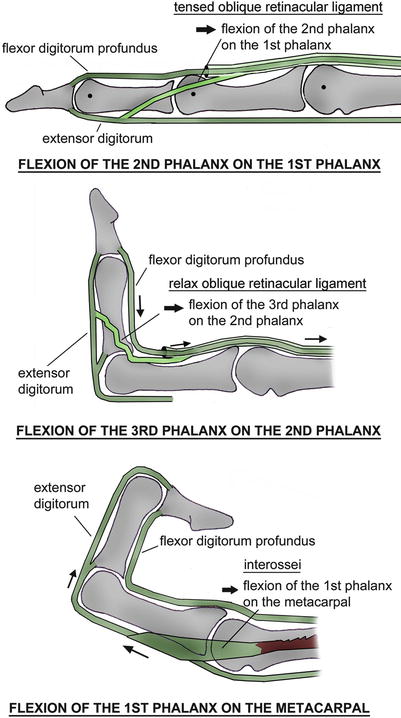
Fig. 10.11
Dynamic of the winding in the long fingers. (1) The contraction of the flexor digitorum profundus doesn’t allow the distal interphalangeal joint to move in flexion while the proximal interphalangeal joint is extended (tension in the retinacular ligament). (2) The flexion of the proximal interphalangeal joint relaxes the retinacular ligament and allows the flexion of the distal interphalangeal joint. (3) The combined flexion of the proximal and distal interphalangeal joints puts the dorsal expansion of the interossei distally in relation with the metacarpophalangeal joint. It then allows the flexion of this joint
The finger winding is made according to an equiangular spiral, described by Littler in 1960.
This spiral respects the divine proportions from the Fibonacci sequence (1-1-2-3-5-8-13-21, etc.) (Fig. 10.12).
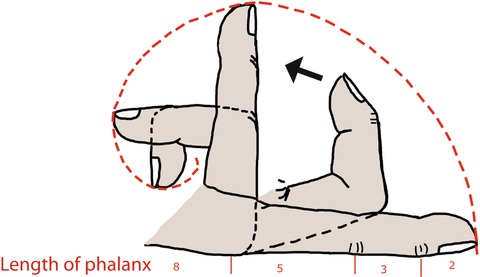
Fig. 10.12
The digital winding describes an equiangular spiral
The path of the flexor tendons in complete flexion is 85 mm above the wrist.
The metacarpophalangeal joint takes care of 77 % of the movement, the proximal interphalangeal joint of 20 % and the distal interphalangeal joint of 3 %.
10.1.7 The Essential Function of the Flexors
The flexor muscles ensure that we can pick up and hold objects tight, with a cocontraction of the extensor and intrinsic systems. They usually work in closed chain, in a concentric way. It corresponds with maintaining and moving an object, for example (Fig. 10.13).


Fig. 10.13
The functional role of the flexors in a closed chain
10.2 Physiopathology
It is most frequently due to direct traumas caused by sharp objects (knife, steel plate, etc.).
However, there are 3 seriousness factors that can lower the functional prognosis:
10.2.1 Sharp Cut or Shredding
The surgical repair is easier in case of sharp cut.
10.2.2 Contamination of the Injury
In case of infection, the risks of adherences and breaks are far more important.
10.2.3 Clamping at the Moment of the Trauma
The flexors can retract higher, pulling out the vincula, which makes the repair more difficult and the healing random.
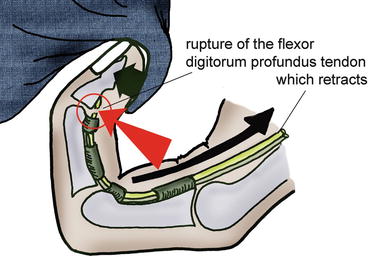
The jersey finger (or rugby finger) is the typical example of this type of injury, where the player (often a rugby player) holds back his opponent by the jersey, which leads to a rupture of the flexor digitorum profundus (often in the ring finger). The tendon can retract until the palm of the hand (Fig. 10.14).