Fig. 9.1
Synovial sheath of the extensor system, allowing its lubrication and nutrition
The tendons are flat, composed by longitudinal fibres and located directly under the skin.
9.2 Topographic Anatomy [1, 2]
The International Federation of Societies for Surgery of the Hand made a classification allowing us to study their physiology depending on their topography (Fig. 9.2).
Fig. 9.2
Topographic classification of the extensors numbers of the finger zones described in the topographic anatomy
9.2.1 Long Fingers
Zone 1
It is the area where the lateral strips end and come together and insert on the base of the dorsal side of the 3rd phalanx. The tendon is not vascularized much at this level [3].
The injuries lead to a mallet finger, characterized by a drop in flexion of the distal phalanx (Fig. 9.3). These deformities can evolve to a swan-neck deformity, especially when the volar plate of the proximal interphalangeal joint is slack (Fig. 9.4).
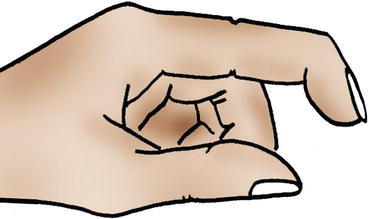
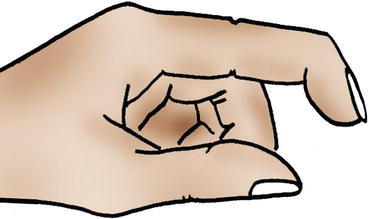
Fig. 9.3
Mallet finger
Fig. 9.4
Swan-neck deformity after a mallet finger badly treated. The tension normally applied on the 2nd and 3rd phalanges is now only applied on the 2nd phalanx. In case of slackness of the proximal interphalangeal joint, this excess of tension leads to a joint in hyperextension
Zone 2
In this zone we find the lateral strips, next to the diaphysis of the 2nd phalanx. The deformity is the same as in zone 1, but there can be an associated injury of the oblique retinacular ligament, leading to a faster swan-neck deformity especially if the volar plate of the proximal interphalangeal joint is slack.
Zone 3
Next to the proximal interphalangeal joint is the area of trifurcation of the extensor system, forming the 2 lateral strips and the median strip ending on the base of the 2nd phalanx.
An isolated injury of the median strip leads to a boutonnière deformity (Fig. 9.5). The lateral strips bend towards the palm, putting the proximal interphalangeal joint in flexion and the distal interphalangeal joint in extension.
Fig. 9.5
Boutonnière deformity
Zone 4
It is the zone next to the diaphysis of the 1st phalanx, at the level of the dorsal expansion of the interossei.
Zone 5
It is the zone next to the metacarpophalangeal joint. At this level, the extensor tendons are stabilized on the metacarpals by the sagittal strips that insert on both sides of the tendon on the inter-glenoidal ligaments (Fig. 9.6).
Fig. 9.6
At the level of the metacarpophalangeal joints, the sagittal strips stabilize the extensor tendons in the frontal plane
These stabilizing elements are tensed when the metacarpophalangeal is flexed and relaxed when it is extended.
An injury in the sagittal strip leads to a dislocation of the extensor tendon in the ulnar inter-metacarpal area, as the extensor system is decentred relative to the axis of the metacarpophalangeal joints. Therefore, the injuries of the ulnar sagittal strip do not lead to a dislocation of the extensor tendon in the radial inter-metacarpal area (Fig. 9.7).
Fig. 9.7
Injury of the radial sagittal strip of the index, leading to a dislocation of the extensor tendon in the inter-metacarpal area
Zone 6
The extensor tendons pass along the dorsal side of the metacarpals. At this level, there are some inter-tendinous junctions that connect the extensor tendons. If there is an injury above the inter-tendinous junctions, the extension deficit will be small, because it is partly compensated by the adjacent tendons (Fig. 9.8).
Fig. 9.8
Inter-tendinous junctions in zone 6
Zone 7
The tendons slide in the synovial sheath next to the extensor retinaculum. Unlike the extensor indicis, the extensor digiti minimi has its own sheath (Fig. 9.9).
Fig. 9.9
Unlike the extensor indicis, the extensor digiti minimi has its own sheath
Zone 8
It is the zone above the extensor retinaculum, until the myotendinous junction.
9.2.2 Thumb
The extensor system of the thumb also depends on an extrinsic system made by the extensor pollicis brevis and the extensor pollicis longus and an intrinsic system made by the sesamoid muscles. The abductor pollicis brevis and the flexor pollicis brevis form the radial part of the dorsal expansion, and the adductor pollicis forms the ulnar part.
9.3 Physiology
9.3.1 Nutrition of the Extensor Tendons
Like the flexor tendons, the nutrition of the extensor tendons depends on an intrinsic system and an extrinsic system. Unlike the flexor tendons, the extrinsic system is the main actor during the tendon healing.
The extensor system is, in fact, mostly extra-synovial, which limits the synovial imbibition role it has at the level of the extensor retinaculum (intrinsic healing by a “synovial pump” effect), and favours the extrinsic healing.
This type of healing leads to important adherences.
9.3.2 Biomechanics
The finger extension depends on two synergic systems:
9.3.2.1 Extrinsic System
This system is made by the extensor digitorum, the extensor indicis and the extensor digiti minimi.
Its isolated contraction brings the metacarpophalangeal joint in extension but does not lead to an extension of the interphalangeal joints. The extensor digitorum exhausts its action on its proximal insertions, leading to a “claw” deformity.
9.3.2.2 Intrinsic System
It is composed by the interossei and the lumbrical muscles that join the extrinsic system at the level of the dorsal expansion of the interossei to form a complex group that ensures the harmony of the digital extension.
The interossei have various endings along the digital chain, which allows them to have various actions, depending on the situation:
On a deep plane, the endings on the lateral tubercles of the 1st phalanx allow them to separate the fingers and bring them closer to each other and to participate in the lateral stability of the metacarpophalangeal joint.
On a superficial plane, they form the dorsal expansion of the interossei next to the metacarpophalangeal joint and give off more distal fibres that reinforce the median strip of the extensor tendon and others associated to the corresponding lumbrical muscles to join the lateral strips. If the metacarpophalangeal joint is extended, the contraction of the interossei brings the interphalangeal joints in extension. If the metacarpophalangeal is flexed, it favours the interphalangeal flexion by relaxing the extensor system (Fig. 9.10).
Fig. 9.10
The interossei realize an extension of the interphalangeals when the metacarpophalangeal is extended but favour the flexion of the interphalangeals when the metacarpophalangeal is flexed
The lumbrical muscles insert on the flexor digitorum profundus at the level of the palm, pass in front of the inter-glenoidal ligament on the radial side and end on the corresponding lateral strip. They play a proprioceptive role, dividing the tension between the 2 systems, which explains the incredible number of mechanoreceptors they contain (Fig. 9.11).


Fig. 9.11
The lumbrical muscles are very sarcomeric and contain a lot of mechanoreceptors. They play an important proprioceptive role regulating the tensions between the flexor system and the extensor system
They also have an extension action in the distal phalanx, regardless of the position of the metacarpophalangeal joint.
9.3.2.3 Retinacular Ligaments
The retinacular ligaments also play an important role in the coordination of the 2 last phalanges by a tenodesis effect:
Transverse retinacular ligament, anchored on the A3 pulley for the proximal half and on the volar plate and the capsule of the proximal interphalangeal joint for the distal part. It goes vertically towards the corresponding lateral strip of the extensor system. It favours the palmar movement of the lateral strips during the flexion of the proximal interphalangeal joint. It forms, with the oblique retinacular ligament, the lateral retinacular ligament (Fig. 9.12).
Fig. 9.12
The transverse retinacular ligament participates in the stabilization of the lateral strips, preventing their movement towards the dorsal area. The median strip prevents their movement towards ventral area
Oblique retinacular ligament, anchored on the flexor sheath next to the diaphysis of the 1st phalanx. It passes in front of the flexion axis of the proximal interphalangeal joint to join the extensor system at the level of the distal interphalangeal joint. This ligament allows the coordination of the distal and proximal interphalangeal joints in flexion and extension. During the flexion of the distal interphalangeal joint, the oblique retinacular ligament gets tensed, automatically leading to a flexion of the proximal interphalangeal joint. During the extension of the proximal interphalangeal joint, the oblique retinacular ligament gets tensed, automatically bringing the distal interphalangeal joint in extension (Figs. 9.13 and 9.14).
Figs. 9.13 and 9.14
The oblique retinacular ligament favours the functional coordination between the distal and proximal interphalangeal joints. The extension of the proximal interphalangeal joint tenses it, which leads to an extension of the distal interphalangeal joint. The flexion of the distal interphalangeal joint is only possible if the proximal interphalangeal joint is flexed (relaxation of the oblique retinacular ligament). The flexion of the distal interphalangeal joint is impossible while the proximal interphalangeal is in extension, as the oblique retinacular ligament is in tension
Thanks to those two elements, there is a functional coordination between the two interphalangeals that can move only in the same direction, forming a functional unit: the interphalangeal system.
9.3.3 Extension Dynamics and Tendon Race [4, 5]
The extension of the fingers starts with the metacarpophalangeal joint, through the action of the extensor digitorum.
The contraction of the lumbrical muscles opposes the tension of the flexor digitorum profundus and therefore the formation of a “claw”.
The contraction of the interossei also participates, through the dorsal expansion, in this fight against the “claw”. Combined with the contraction of the extensor digitorum, it brings the proximal interphalangeal joint in extension.
The extension of the proximal interphalangeal joint brings the distal interphalangeal joint in extension by putting the oblique retinacular ligament in tension (tenodesis effect).
The tendinous race of the extensor system during the complete extension of the fingers is 15 mm on the back of the hand, 4 mm on the back of the 1st phalanx, 6 mm at the level of the proximal interphalangeal joint and 3 mm at the level of the distal interphalangeal joint.
9.4 Physiopathology [6–8]
There are two types of injuries of the extensor system:
Subcutaneous rupture: the most frequent is at the level of the distal interphalangeal joint and leads to a mallet finger. We can also observe this injury at the level of the metacarpophalangeal joint after a punch that causes a rupture of the sagittal strip and a dislocation of the extensor in the inter-metacarpal area. In the thumb, the injury is most often in the extensor pollicis longus at the level of the Lister tubercle, where the muscle changes its direction (Fig. 9.15).
Fig. 9.15
The Lister tubercle is a “risky” area for the extensor pollicis longus, as the muscle changes its direction at this level, which increases the constraints on it
Open traumas: they most often affect the index or the thumb. The severity depends on the nature of the device that has damaged the extensor system and on the associated injuries. In traumas by crushing, the dorsal abrasions and infectious factors worsen the functional prognosis.
9.5 Clinical and Paraclinical Signs [9, 10]
Various clinical tests make it possible to determine an injury of the extensor system:
Extensor pollicis longus: with the hand lying flat on the table, the patient is asked to lift the thumb from the table (Fig. 9.16).
Fig. 9.16
If the patient cannot lift his thumb from the table, the extensor pollicis longus is probably broken
Extensor pollicis brevis: we ask the patient to attempt an extension of the metacarpophalangeal joint.
Extensor indicis and extensor digiti minimi: we ask the patient to make a selective extension of the index and the little finger (“make horns”) (Fig. 9.17).
Fig. 9.17
“Horn” test verifying the integrity of the extensor indicis and extensor digiti minimi
Extensor digitorum: the patient must be able to realize a selective extension of the phalanges against resistance. If there is an injury above the inter-tendinous junctions, a relative compensation can be realized by the adjacent extensor tendons. The extension of the 3rd phalanx can only be realized with the proximal interphalangeal joint in extension, thanks to the relaxation of the median strip allowing an action of the lateral strips. If the extension of the distal interphalangeal joint is possible with the proximal interphalangeal joint in flexion, it means there is a rupture of the median strip. The tension of the median strip relaxes the lateral strips, making them inactive on the distal interphalangeal joint (we say that the 3rd phalanx is “dangling”). This phenomenon is the physiological base of the Elson test (Fig. 9.18).
Fig. 9.18
Elson test: if the median strip is broken, the flexion of the proximal interphalangeal joint does not relax the lateral strips. The lateral strips keep their efficiency and are able to realize an extension of the distal interphalangeal joint
9.6 Therapeutic Process and Surgical Treatment
9.6.1 Orthopedic Treatment
The subcutaneous injuries in zones 1, 2, and 3 are most often treated by a strict immobilization during 8 weeks, with a nocturnal immobilization for 15 more days if the patient cannot lock in extension at the end of the 8 weeks.
9.6.2 Surgical Treatment [11]
The wounds are the most frequent injuries of the extensor tendons. The extensor tendons are, in fact, very superficial, subcutaneous on the dorsal part of the hand and wrist. Therefore, they are very exposed in case of wound.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








