Tendon
Anatomic landmark
Dimensions (mm)
Supraspinatus
Maximum medial-to-lateral length
6.9 ± 1.4
Anteroposterior width of medial margin
12.6 ± 2.0
Anteroposterior width of lateral margin
1.3 ± 1.4
Infraspinatus
Maximum medial-to-lateral length
10.2 ± 1.6
Anteroposterior width of medial margin
20.2 ± 6.2
Anteroposterior width of lateral margin
32.7 ± 3.4
Articular capsule
Medial-to-lateral length at posterior edge of the supraspinatus footprint
4.5 ± 0.5
The rotator cuff serves as a dynamic stabilizer for the glenohumeral joint and dynamically compresses the head of the humerus into the glenoid socket. Study of individual tendon origins and insertions highlights rotator cuff vectors of force and predicts individual tendon function. The subscapularis internally rotates the humeral head in relation to the scapula. The infraspinatus and teres minor externally rotate the humerus. The primary function of the supraspinatus is to initiate the first 30° of forward elevation and assist the deltoid in the first 90° of abduction. In addition, it serves as a humeral head compressor. The supraspinatus also plays a role in rotation. From a neutral or externally rotated starting position, the supraspinatus externally rotates the humerus, and when starting from a position of internal rotation, the supraspinatus internally rotates the humeral head [9, 10]. It has been hypothesized that interaction between cuff regions may explain why some patients retain strength after partial rotator cuff tears [10]. Restoration of the anterior and posterior force couple may adequately restore the centering force of the rotator cuff and provide a stable fulcrum for glenohumeral motion. Some studies have demonstrated that partial repair of the posterior portion of an irreparable two-tendon tear may restore function to a cuff-deficient shoulder [11]. Rotator cuff repair surgery aims to alleviate symptoms and reestablish rotator cuff function.
The enthesal sites of insertion are composed of specialized fibrocartilaginous tissue, which serve to minimize stress concentrations at the tendon-bone interface [12]. The enthesis is composed of well-organized zones of tissue, including the tendon proper, fibrocartilage, mineralized fibrocartilage, and bone [13]. Interruption of the enthesis does not spontaneously heal after initial injury, and these zones of interface are not histologically preserved after rotator cuff repair. Thus, structural integrity is compromised, and healing proceeds with disorganization and decreased strength as compared to the native rotator cuff construct [13]. Several studies have documented a correlation between symptomatic and functional results of rotator cuff repair and quality of healing [14–23]. As such, a robust repair that allows for anatomic healing is the primary goal of rotator cuff repair, and techniques to maximize tendon healing are of great interest for their potential to improve clinical outcomes.
History of Rotator Cuff Repair
Traditionally, both open and arthroscopic rotator cuff repairs were performed using a single row of suture anchors. The suture anchors are traditionally placed linearly along the anterior to posterior aspect of the greater tuberosity. Investigators have attempted to correlate the integrity of these repairs with postoperative function with varying results [24–27]. Outcomes after repair have been hypothesized to be related to biomechanical strength, contact area, implant failure, and suturing pattern. Concerns over the adequacy of the strength of single-row techniques have motivated the development of new repair approaches. One such development has been double-row fixation, which better restores the anatomic footprint of the rotator cuff and provides a biomechanically stronger construct compared to single-row repair [28]. This represents a major advancement in arthroscopic technique, incorporating a linear row of anchors placed medially at the articular margin and a second row along the lateral aspect of the rotator cuff footprint on the tuberosity [29–31].
Repair Failures
Individual rotator cuff tears vary greatly in their configuration and prognosis. Clinical outcomes are reported as good to excellent in only about 85 % of repairs [24, 32–35] and are worse with increasing preoperative tear size and poorer tissue quality [22, 23, 25, 28, 36–38]. Gerber et al. hypothesized that initial fixation strength and minimal gap formation upon stress would improve rates of healing for rotator cuff repair [39]. Tendon-bone healing has been a much-debated topic of recent research investigations. Studies have demonstrated that the degree of rotator cuff atrophy and fatty infiltration, quality of repair, and postoperative restoration of shoulder flexibility and strength have all proven to be important determinants of the ultimate success of rotator cuff repair [25–27, 40, 41]. Reasons for failure can be roughly grouped into four categories: technical, biologic, mechanical, and anatomic.
Increased surgeon comfort with arthroscopy and improvements in suture material, anchor, and arthroscopic technology have reduced concern for technical causes of rotator cuff repair failure such as suture anchor failure [42]. Additionally, recent studies have demonstrated that functional results after arthroscopic repair versus those after open or mini-open repair are equivalent, and patients report less postoperative pain and increased satisfaction with this method [5, 35, 43–49]. In addition, technical advances have fostered improvement in fixation via suture anchor design. As stronger suture materials have been introduced, constructs have greatly surpassed previously achieved biomechanical strength parameters and have shown impressive healing rates after arthroscopic rotator cuff repair [50].
Biologic failures are those related to tendon-bone healing. These failure modalities are often highly dependent on the individual patient and can be attributable to factors such as age, smoking status, history of corticosteroid injection, diabetes, vascular disease, or tear chronicity, resulting in fatty atrophy of muscle [51]. Of these factors, age appears to be the leading biological determinant regarding success or failure of rotator cuff repair. Tashjian et al. reported that of 49 repairs, only 51 % were healed by examination on ultrasound 6 months postoperatively, with age at surgery and longer duration of follow-up being significantly associated with lower healing rates after rotator cuff repair [52]. Intrinsic patient factors such as tobacco use have been less well established by the literature, with conflicting findings reported in various publications. For example, animal studies have demonstrated nicotine’s effect in delay of tendon-to-bone healing; however, these effects have not been consistently confirmed clinically [53–56].
Mechanical failures are related to the inability of the repair to overcome the exertional force placed upon the repaired tendon. The rotator cuff endures significant mechanical forces with shoulder motion and loading. Forces on the cuff muscles differ according to position during loading. The durability of cuff repair is dependent on repaired tendons to maintain integrity in the setting of forces applied across the glenohumeral joint. Specifically, most tears originate at the junction between the supraspinatus and infraspinatus tendons, roughly 13–17 mm posterior to the biceps tendon [57], and force vectors applied across these tendons will cause differential relative stress across the tendons. The supraspinatus experiences maximal loading in a position of internal rotation and abduction [58]. Conversely, the infraspinatus experiences maximum force in a position of external rotation and adduction [58]. Finally, anterior cuff tears are less common and result in tears to the subscapularis tendon, which endures relatively high forces in both internal rotation with abduction and adduction [58]. Given differential tendon loading, some surgeons advise tailored postoperative rehabilitation protocols based on tear size and location, though there is no definitive study on the effectiveness of this strategy and more research is required to advise these strategies. In general, however, it is known that early motion and loading may compromise tendon-bone healing. A study by Lee et al. demonstrated that aggressive early passive rehabilitation was associated with retear rate more than twice that of limited passive rehabilitation [59].
Anatomical failures are related to inability to restore the native insertional footprint of the rotator cuff or failure to restore resting tension of the tendons. Apreleva et al. introduced the concept of the anatomical footprint of the rotator cuff [60], and, since, multiple studies have sought to develop techniques to improve upon the restoration of repair site insertion. It is hypothesized that superior restoration of the native footprint of the rotator cuff fosters improved healing of the tendinous insertion, as the footprint is thought of as the maximum two-dimensional healing zone [61]. Repairs that do not restore the cuff footprint endure greater force across the repaired site and suture anchors and may predispose these repairs to higher failure rates [31].
Double-row repair, while mechanically advantageous, may present unique problems. Unlike the typical modes of leading edge failure related to rotator cuff repair in general, double-row cuff repairs appear to present a previously unreported mode of failure. Trantalis et al. reported this unique failure pattern in patients who underwent double-row rotator cuff repair in a subset of five patients. In these patients footprint repair appeared to be well fixed to the greater tuberosity with normal thickness. However, on arthroscopic examination, each of these patients incurred a full-thickness tendon tear medial to the intact footprint [62]. Such failures have been hypothesized to be related to tension overload of the suture-tendon interface at the medial repair site. This mechanism of loading has been supported by Mazzocca et al., who demonstrated that cyclic loading of a double-row repair first resulted in failure of the medial site by mattress sutures pulling through the tendon medial to the repair site [63]. Similar findings were reported in a case report by Yamakado et al. in which the authors found tendon avulsion at the medial row with concomitant exposure of knots on the bony surface of the rotator cuff footprint [64]. The authors hypothesize that the requirement of pulling the tendon more laterally for double-row repair results in a relatively high tensile stress compare to single-row repair [65]. In spite of these reports, double-row rotator cuff repair appears to be successful and further studies are required to evaluate the long-term impact of medial row stress on repair as well as the incidence of failures.
Rationale for Double-Row Rotator Cuff Repair
Double-row rotator cuff repair has been hypothesized to result in superior fixation for a number of reasons including increased restoration of the rotator cuff footprint, increased mechanical strength and contact pressure, as well as decreased gap formation across the repair.
Restoration of Rotator Cuff Footprint
Success of rotator cuff repair is dependent on tendon-to-bone healing. Tendon healing is initiated by the development of fibrovascular tissue interface [66]. Woven bone formation begins at the bone-tendon interface, eventually resulting in collagen fiber continuity between tendon and bone [67]. Aoki et al. demonstrated that an increase in available healing surface at the bone-tendon junction increased the potential for bone-to-tendon healing and formation of such a collagenous interface. Thus, repairs with greater coverage of the native footprint of the rotator cuff theoretically offer greater healing potential than those that do not provide as much interface, with the footprint being described as the maximum two-dimensional healing zone.
Meier et al. utilized three-dimensional mapping to determine the area of the footprint recreated with transosseous simple suture technique, fixation with a single row of suture anchors, and double-row suture anchor technique fixation. This study demonstrated that double-row suture anchor fixation consistently reproduced 100 % of the original supraspinatus footprint. In contrast, single-row suture anchor fixation and transosseous simple suture techniques reproduced only 46 % and 71 % of the insertion site, respectively [68]. Brady et al. demonstrated similar results, finding that after an isolated lateral-row repair, 52.7 ± 9.2 % of the rotator cuff footprint remains uncovered, and, on average, the double-row repair offered over twice the footprint coverage yielded by a single-row repair [69]. Thus, double-row fixation may provide a tendon-bone interface better suited for biologic healing and restoration of normal anatomy.
Mechanical Strength
In biomechanical studies of the initial mechanical strength of rotator cuff repair, double-row repair has proven to have superior strength as compared to single-row repair. In a study by Meier and Meier, the authors studied repair strength in 30 fresh-frozen cadaveric shoulders with full-thickness supraspinatus tears; the authors found that the fixation strength of the double-row repair suture anchor technique proved to be significantly greater than that of single-row suture anchor repair or transosseous technique. Samples were subjected to cyclic load testing from 5 N to 180 N at a rate of 33 mm/s until complete failure or a total of 5000 cycles. The transosseous repair group failed at an average of 75.3 ± 22.49 cycles, single-row repairs failed at an average of 798.3 ± 73.28 cycles, and the double-row suture anchor repair group had no failures because all samples were stopped when 5000 cycles had been completed [68]. Thus, both the increased footprint apposition and increased strength afforded by double-row constructs minimize gap formation during cyclic loading.
Contact Area and Pressure
In addition to the establishment of the native footprint of the rotator cuff, contact pressure is an important factor in the establishment of native cuff dynamics. Tuoheti et al. studied full-thickness cuff tears treated with transosseous, single-row, and double-row repairs in ten cadaveric specimens and determined that contact area of the double-row technique was 42 % greater than that of the transosseous technique and 60 % greater than that of the single-row technique. Moreover, the average pressures of the single-row and double-row techniques were 18 % and 16 % greater, respectively, than that of the transosseous technique. There was no demonstrated significant difference between contact pressure in the single-row and double-row techniques [70]. In the study of time zero contact pressure over the rotator cuff footprint in an established sheep model, Baums et al. investigated contact pressure across rotator cuff repair sites in 40 fresh-frozen shoulders, demonstrating that contact pressure was lowest for single-row repair and for simple stitch configurations. Double-row repair and arthroscopic Mason-Allen/horizontal mattress stitches significantly increased repair contact pressure [71]. Park et al. demonstrated that a transosseous-equivalent (TOE) rotator cuff repair via tendon suture bridges improves pressurized contact between the tendon and tuberosity when compared with a double-row technique [72]. These results support the use of double-row repair, more complex arthroscopic Mason-Allen stitches, and suture bridging techniques in the setting of a complex tear requiring additional aid in healing. Such techniques may improve the environment for healing of the repaired rotator cuff tendons and should be weighed against the risk of potential increased tension, tissue strangulation, and devascularization that TOE configurations may confer.
Gap Formation
As alluded to above, the minimization of gap formation is another key factor in the restoration of the anatomical configuration and mechanical performance of tendon-bone insertion to sufficiently sustain loading associated with functional activity. In a study by Smith et al., the investigators found that gap formation during static loading was significantly greater in the single-row group than in the double-row group [73]. Under cyclic loading gap formation was not found to be significantly different between groups; however, double-row repairs endured significantly greater loading forces prior to failure [73]. Thus, double-row repair reconstruction may provide a more reliable construct with superior resistance to gap formation and greater loading prior to failure. The early postoperative period is a critical phase prior to healing, during which time the load transfer from tendon to bone is entirely carried through the means of the repair construct. Thus, it is reasonable to presume that if a repair is predisposed to increased gap formation, this would be detrimental for appropriate healing as tendon-bone contact would be reduced. This is of particular concern in the setting of constant postoperative static loading with the patient’s arm held in a sling.
Repair Techniques
A number of techniques are available to the shoulder surgeon in order to execute the repair appropriate for any given patient. Among these, the workhorse repairs include simple single- and double-row repairs and can be additionally augmented by suture linking techniques as well as TOE repair.
Single-Row Repair
The single-row technique involves repair of a rotator cuff tear with a single row of medial anchors. Different types of anchors are available with variation in size, screw thread pattern, material, number of preloaded sutures, and type of fixation. These properties all result in variation in strength of fixation. Vented anchors are now available, which are hypothesized to cause migration of bone marrow elements to the repair site through the holes of the anchor (Fig. 18.1).
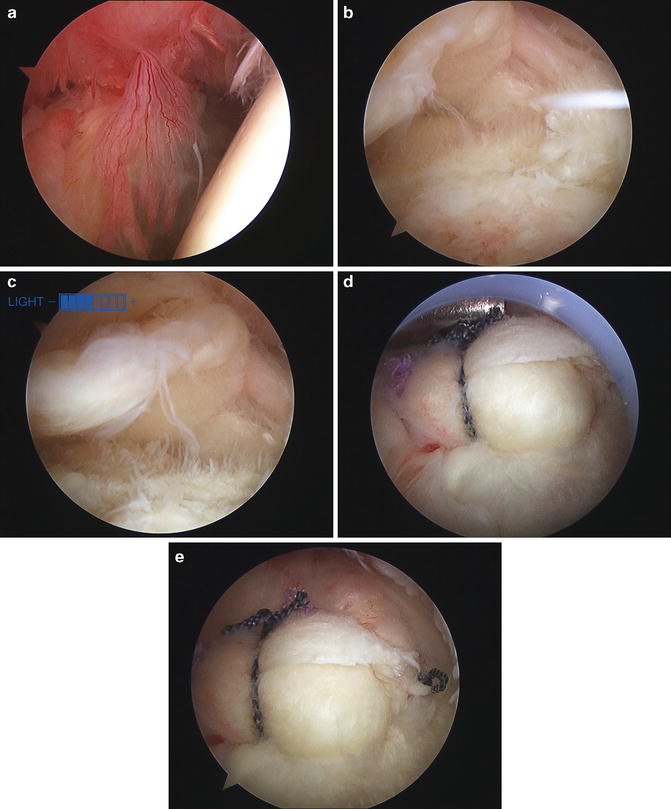
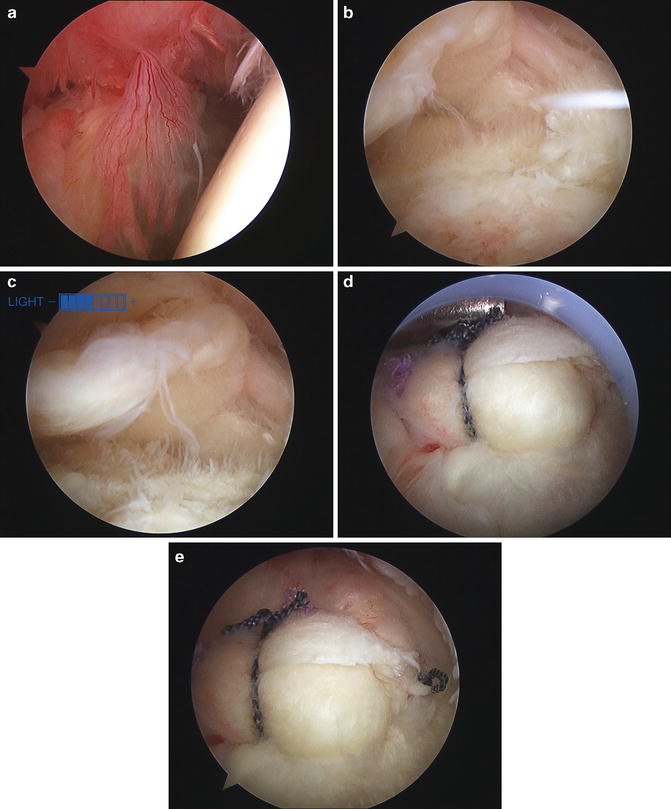
Fig. 18.1
Single-row rotator cuff repair, performed in this case secondary to significant synovitis and concern for postoperative stiffness. (a) Beach chair position, right arm, viewing from posterior portal demonstrating extensive synovitis. (b and c) Beach chair position, subacromial space of right shoulder demonstrating rotator cuff tear. (d and e) Viewing from lateral portal, repaired rotator cuff with single row
Double-Row Repair
The double-row technique implies two rows of anchors: a medial row and a lateral row. Similar to single-row repair, this technique may include the use of suture anchor with a broad variation in properties. Additionally, these repairs vary in configuration of suture anchor placement (Fig. 18.2).
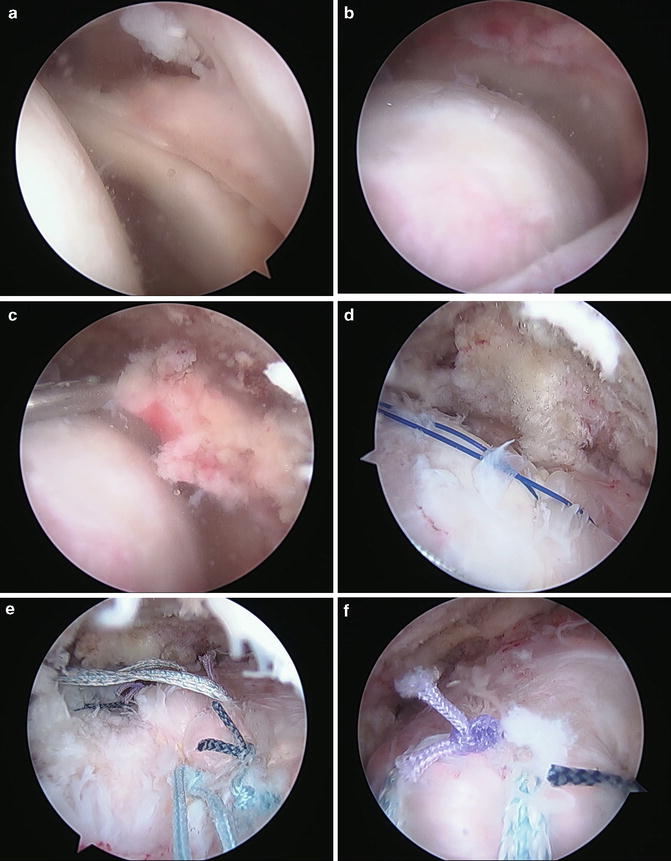
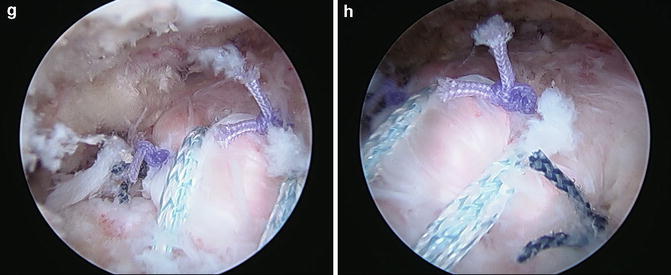
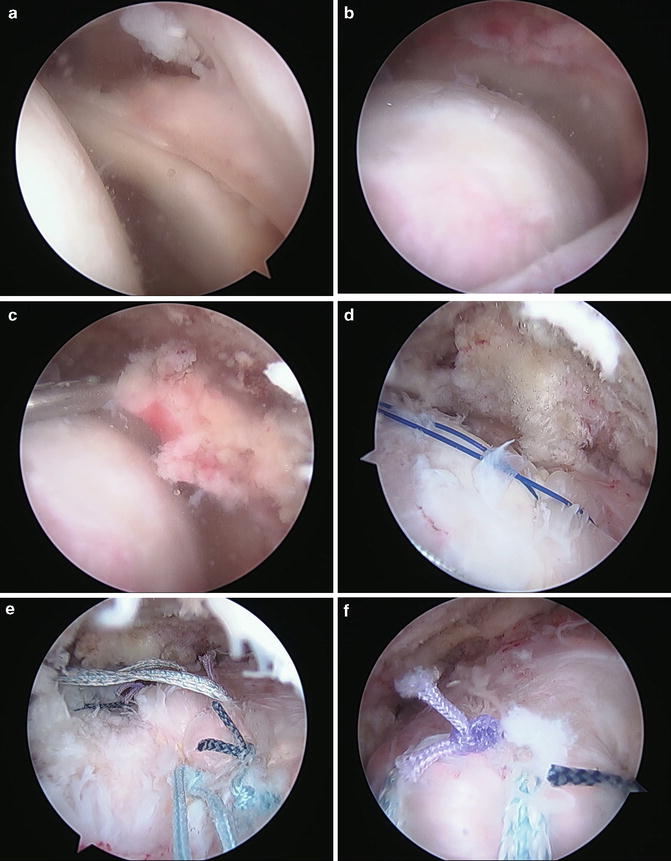
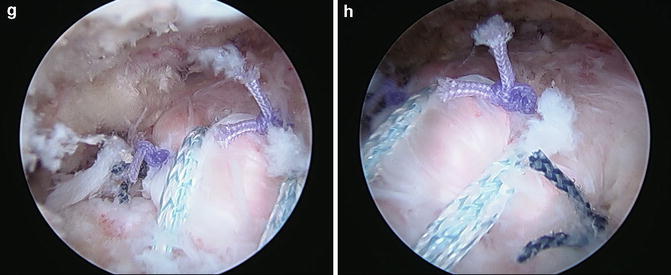
Fig. 18.2
Single-row rotator cuff repair with a tension relaxing stitch to a lateral-row anchor performed because the repair was felt to be under high tension after a single-row repair. (a and b) Beach chair position viewing from posterior, left shoulder, showing retraction of rotator cuff to glenoid. (c and d) Viewing from posterior demonstrating difficulty to mobilize cuff to footprint using arthroscopic grasper and a traction suture. (e–h) Repair completed with single-row technique in “e” and then additional sutures that were passed through the rotator cuff in a horizontal mattress fashion were taken to lateral-row anchors to take tension off of the medial row repair
Linked Double-Row Repair
Linked double-row repair represent a variation in double-row repair. This technique links the medial and lateral rows by passing limbs of suture from medial to lateral row, thus creating a crisscross suture configuration, ensuring large contact area and contact pressure at the bone-tendon interface (Fig. 18.3).
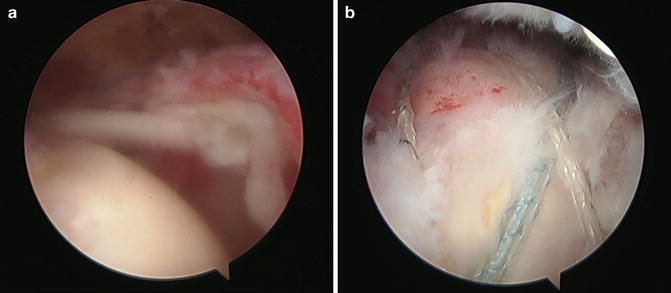
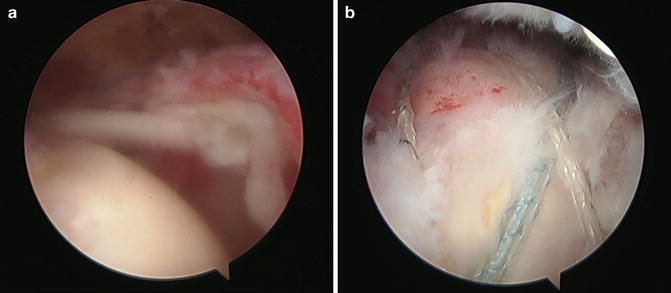
Fig. 18.3
Double-row rotator cuff repair performed in this case as the tendon was easily mobilized to the footprint, and there was no sign of synovitis or arthritis on diagnostic arthroscopy of the glenohumeral joint. (a) Beach chair position, left shoulder, viewing from posterior demonstrating a rotator cuff tear retracted almost to the level of the glenoid, which mobilized easily to the footprint when traction was applied. (b) Completed double-row repair viewing from a lateral portal
Anchorless and Transosseous-Equivalent Double-Row Repair
Anchorless repairs have been introduced in order to improve upon current cuff repair options. This technique involves the creation of two converging bone tunnels: one where medial anchors are generally placed and one where lateral anchors are placed in parallel line. With this system, it is possible to perform a transosseous technique in a reproducible fashion. This novel technique combines the clinical advantages of minimally invasive arthroscopic surgery and the biomechanical advantages of open transosseous procedures [74]. The TOE repair involves the creation of a medial row of suture anchors that utilize mattress repairs and lateral fixation points, roughly 1-cm distal-lateral to the lateral edge of the tuberosity footprint insertion. After the medial row is repaired, the suture limbs are then used to create suture bridges over the tendon [72].
TOE anchorless repair has controversial supporting data. The repair was developed in order to maximize the utility of a single-row repair technique by preserving the suture limbs of the medial single-row and bridging these sutures over the footprint insertion with distal-lateral interference screw suture fixation [72]. The geometry of the construct is thought to compress the tendon, optimizing tendon-to-tuberosity contact dimensions while additionally providing appropriate repair strength to withstand forces placed on the rotator cuff. In a study by Park et al., transosseous rotator cuff repair technique was shown to restore greater anatomic footprint contact and provide greater ultimate strength, compared with a double-row repair technique [75, 76]. A follow-up study by Salata et al. compared TOE repair to a curved bone tunnel and with a repair technique utilizing a simple or X-box suture configuration. TOE resulted in superior contact area, pressure, and failure rates compared to non-bridging double-row repair [72, 77].
Clinical Outcomes
Clinical outcomes of single- and double-row rotator cuff repair have borne out to be roughly equivalent. Multiple studies have investigated the effects of double-row repair with various outcomes scores and have failed to delineate differences in clinical outcomes based on the repair technique; however, in a study by Parks et al., the authors delineated groups based on preoperative tear size and found an improved functional outcomes scores with double-row fixation for large or massive tears (>3 cm), suggesting that double-row repair configurations may have a clinically relevant role in the treatment of large to massive cuff tears [78]. A meta-analysis by Millet et al. also suggested that stratification of tear size suggests superiority of double-row repair in treatment of large rotator cuff tears [79]. This investigation additionally suggested that longer-term studies might be necessary to delineate clinical effects of repair method as the progression to full-thickness retear may be more commonly seen in single-row repairs and be correlated with poorer clinical outcomes [79] (Table 18.2). Given these results, it is reasonable to consider tear size and patient age in consideration of approach to rotator cuff repair, though larger-sized and longer-term clinical trials are required to better understand the implications of repair in these patients.
Study | Intervention | N | Population difference | Tear length (sagittal plane) | Mean follow-up (months) | Outcomes | Relevant findings |
|---|---|---|---|---|---|---|---|
Gartsman et al. (2013) | SR versus DR retear rate | 83 (40 SR, 43 DR) | Included any repairable full-thickness tear; excluded smokers, steroid users, bilateral cuff repairs, suprascapular nerve decompressions | SR: <2.5 cm DR: <2.5 cm | SR: N/R DR: N/R Mean: 10 (6–12) | Subjective: N/R Objective: N/R Imaging: US | DR had significantly decreased retear rate (7 %) compared with SR (25 %) (P = 0.024) |
Carbonel et al. (2012) | SR versus DR; clinical outcome and retear rate | 160 (80 SR, 80 DR) | Excluded OA, tears >5 cm, Fuchs >4, steroid users | SR 1–3 cm: 51 SR 3–5 cm: 29 DR 1–3 cm: 53 DR 3–5 cm: 27 | SR: 24 DR: 24 MRI SR: 24 MRI DR: 24 | Subjective: ASES, UCLA, constant Objective: physical examination, SSI, ROM in degrees Imaging: MRI | DR significantly improved over SR in 1- to 3-cm tears with respect to degrees of flexion and abduction, internal rotation SSI, and external rotation SSI; DR significantly improved over SR with respect to all measured variables in 3- to 5-cm tears except for Constant score, abduction SSI, and external rotation SSI |
Lapner et al. (2012) | SR versus DR; clinical outcome and retear rate | 80 (40 SR, 40 DR) | Included any full-thickness tear; excluded SSx <6 months, GFDI >3, ACH distance <7 mm
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|





