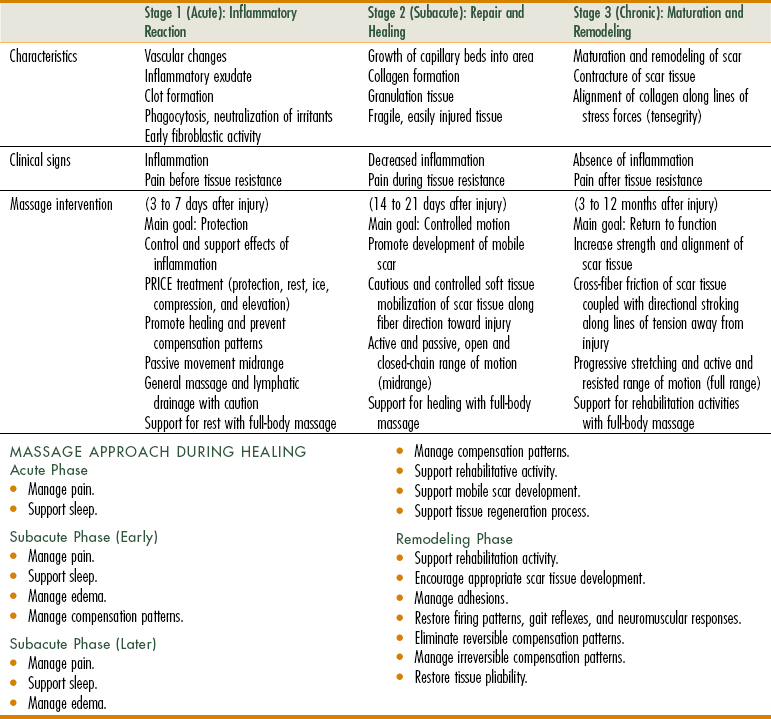
Chapter 9 After completing this chapter, the student will be able to perform the following: 1 List the general indications for massage. 2 Describe illness and injury and how they predispose a client to contraindication or caution for massage application. 3 Evaluate various medications for indications/cautions for massage. In general, massage is indicated for • Effective digestion and elimination • Efficient circulation of body fluids • Enhanced growth, development, and regeneration of injured tissue • Exercise recovery and performance 1. Stimulation from massage activates release of the body’s own antiinflammatory agents. 2. Certain types of massage promote the inflammatory process (therapeutic inflammation) to a small degree, triggering the body to complete the process. 3. Massage may facilitate dilution and removal of the irritant by increasing lymphatic flow. The processes of inflammation trigger tissue repair. Tissue repair is the replacement of dead cells with living cells. In the type of tissue repair called regeneration, the new cells are similar to those they replace. In another type of tissue repair called replacement, the new cells are formed from connective tissue and are different from those they replace, resulting in a scar. Often fibrous connective tissue replaces damaged tissue. Most tissue repairs are a combination of regeneration and replacement. A goal of the healing process is to promote regeneration and keep replacement to a minimum. Massage has been shown to slow the formation of scar tissue and to keep scar tissue pliable when it does form (Table 9-1). Client use of antiinflammatory medications is another factor that must be considered. If a person is taking such medication—steroidal or nonsteroidal—the effectiveness of therapeutic inflammation is negated or reduced, and restoration mechanisms are inhibited. When these medications are used, any methods that create inflammation are to be avoided (Table 9-2). TABLE 9-2 Disorders Related to Chronic Inflammation* *Seemingly unrelated disorders often have a common link—inflammation. This is a partial list of common medical problems associated with chronic inflammation. From Fritz S: Mosby’s fundamentals of therapeutic massage, ed 3, St Louis, 2004, Mosby. Pain is usually classified as acute, chronic, intractable, phantom, or referred. Pain has many characteristics. Location, for example, can be divided into four categories: 1. Localized pain is pain confined to the site of origin. 2. Projected pain is typically a result of proximal nerve compression. This pain is perceived in the tissue supplied by the nerve. 3. Radiating pain is diffuse pain, which is not well localized, around the site of origin. 4. Referred pain is felt in an area distant from the site of the painful stimulus.
Indications and Cautions
Indications for Massage
Inflammation
Disorder
Mechanism
Allergy
Mediators induce autoimmune reactions.
Alzheimer’s disease
Chronic inflammation destroys brain cells.
Anemia
Mediators attack erythropoietin production.
Aortic valve stenosis
Chronic inflammation damages heart valves.
Arthritis
Inflammatory mediators destroy joint cartilage and synovial fluid.
Asthma
Mediators close the airways.
Cancer
Chronic inflammation causes most cancers.
Congestive heart failure
Chronic inflammation causes heart muscle wasting.
Fibromyalgia
Mediators are elevated in fibromyalgia patients.
Fibrosis
Mediators attack traumatized tissue.
Heart attack
Chronic inflammation contributes to coronary atherosclerosis.
Kidney failure
Mediators restrict circulation and damage nephrons.
Lupus
Mediators induce an autoimmune attack.
Pancreatitis
Mediators induce pancreatic cell injury.
Psoriasis
Mediators induce dermatitis.
Stroke
Chronic inflammation promotes thromboembolic events.
Surgical complications
Mediators prevent healing.
Pain
Evaluation and Management of Pain
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Indications and Cautions
Only gold members can continue reading. Log In or Register to continue