29 Incomplete Resection of Sarcoma at the Hand
29.1 Patient History Leading to the Specific Problem
An 88-year-old woman presented in our clinic with a painless lump in the proximal phalanx of her left ring finger. She reported that, because of the tumor, she was operated on the same finger 3 months previously in an outpatient setting. During the previous procedure, the team attempted to remove the tumor, but were interrupted. The swelling did not disappear and increased since the intervention. Recently, the finger started to become painful. The previously excised tissue was histologically analyzed. The diagnosis of a chondrosarcoma with G2 grading was established. Surgical margins were not evaluated; therefore, the resection status was unclear.
29.2 Anatomic Description of the Patient’s Current Status
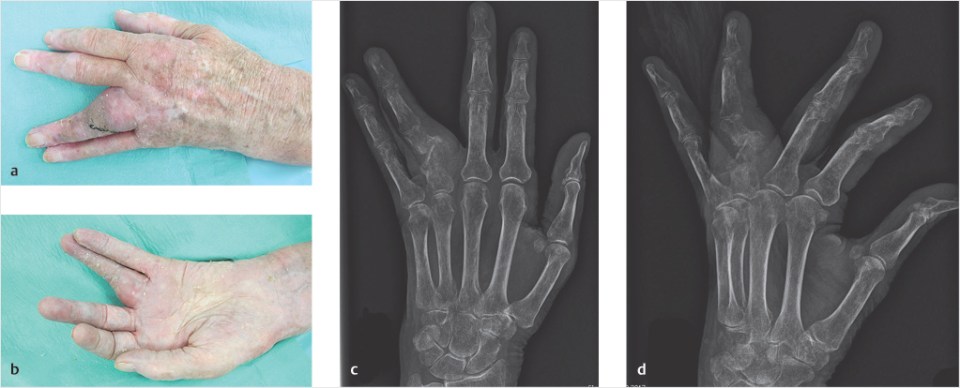
The patient presented with a 2 × 3 × 1 cm large mass at the radial aspect of the proximal phalanx of the left ring finger (▶Fig. 29.1a, b). At inspection, there was an apparent ulnar displacement of the finger because of the tumor. There was an oblique scar on the ulnodorsal border of the finger from the previous surgery. Circulation and sensitivity of the finger were intact. On X-ray examination of the finger in anteroposterior and lateral views, the proximal phalanx showed a pathological fracture, signs of osteolysis, and a potential invasion of the soft-tissue tumor in the bone (▶Fig. 29.1c, d). In the MRI scan, which was performed before the initial surgery, the tumor semicircumferentially enclosed the proximal phalanx from dorsally (▶Fig. 29.1e, f).
29.3 Recommended Solution to the Problem
When treating patients with sarcoma of the hand and forearm, we typically aim to receive clear (negative) margins. Moreover, we routinely check for distant metastasis, which usually occurs in the lungs. Thus, initially a pulmonary CT scan was performed. Given the destruction of the proximal phalanx, the size of the tumor and the accompanying pain, we recommended to perform an amputation by exarticulation of the ring finger at the level of the metacarpophalangeal joint. The patient demanded a simple solution, so we did not discuss and evaluate in detail techniques such as a ray transposition in order to reduce the generated gap. Transpositions have mixed results in many hands; therefore, we aim to adapt our recommendations according to the patient’s situation. When performing an exarticulation, we wanted to ensure we had sufficient skin and soft tissue for defecting coverage; otherwise, a local flap such as a reversed dorsal metacarpal artery would have been necessary. Intraoperatively, there was a moveable layer surrounding the tumor, thus ensuring an excision without the necessity of flap coverage.
29.3.1 Recommended Solution to the Problem
• Confirming the diagnosis with biopsy.
• Staging of the patient and presentation of the case in an interdisciplinary tumor board.
• Tumor resection with clear margins.
• Exarticulation of the affected finger at the level of the metacarpophalangeal joint.
• Sufficient soft-tissue coverage.