Chapter 3 Imaging
The Basis for a Sound Decision in Joint Preservation
Introduction
Radiologic assessment of the knee may provide a tremendous amount of information when proper radiographs are performed and patterns of wear are recognized. A standard series of digital radiographs that we perform at our center include a 54-inch anteroposterior (AP) axial alignment x-ray (with radiographic markers for magnification), standing bilateral AP, 45-degree bent standing posteroanterior (PA; Rosenberg views1), and a tangential patellar skyline view at 45 degrees supine. Supine AP radiographs of the knee should not be performed because they are not useful for determining the cartilage joint space and hence the potential for joint preserving-surgery.
Radiologic patterns of osteoarthritis
Advanced tricompartmental osteoarthritis is exceedingly rare except in the presence of advanced unicompartmental disease with tibiofemoral subluxation. Ahlback2 reviewed a Swedish population in the region of Stockholm and published his report in 1968. He reviewed weight-bearing radiographs of 1,800 knees from approximately 1,200 patients. A series examining arthrosis reviewed 281 patients comprising 370 knees with joint space narrowing. Standing AP projections (but not PA projections) were taken: loading 20 degrees bent axial patellofemoral views and supine lateral views. The Venn diagrams shown in Figure 3–1 were constructed depicting the wear patterns noted.
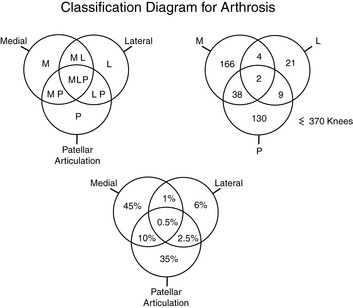
Figure 3–1 Venn diagrams demonstrating the predominance of osteoarthritic joint space narrowing in the medial and patellar articulations of the knee. In this classic study, which was the basis for the classification proposed by Ahlback,2 tricompartmental arthritis was exceedingly rare in a Swedish cohort of 370 knees examined in the 1960s in the Stockholm region.
The predominant arthritic wear patterns in the medial and patellofemoral articulations occur in 80% patients. The lateral compartment usually wears posteriorly.1 These numbers may change slightly if standing PA views are included. In any case, the Venn diagrams demonstrate that unicompartmental and bicompartmental wear are more common than tricompartmental wear. Therefore, total knee arthroplasty may be an overly aggressive solution to osteoarthritis in a younger patient population. Cartilage repair, possibly combined with osteotomy, or unicompartmental or bicompartmental resurfacing arthroplasty when bone-on-bone changes are present may be more suitable in an attempt to preserve the joint for as long as possible.
Medial Osteoarthritis
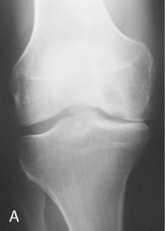
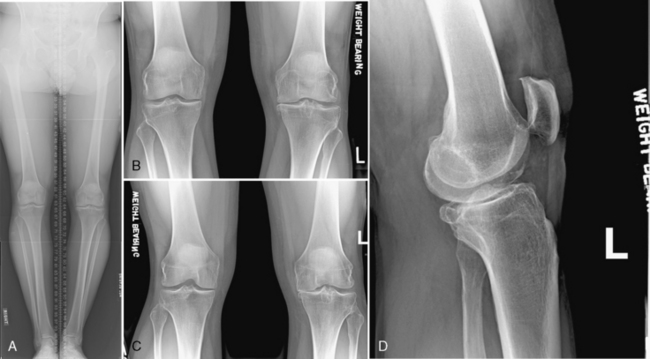
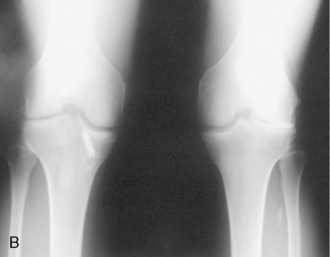
Standing AP x-ray films generally demonstrate early joint space narrowing for the medial wear pattern of osteoarthritis (Figure 3–2). With medial osteoarthritis, a standing PA x-ray film may demonstrate increased posterior joint space unless anterior cruciate ligament (ACL) deficiency is present, in which case tibial translation anteriorly permits a posterior wear pattern on the medial side (Figure 3–3).3
Lateral Tibiofemoral Osteoarthritis
Lateral osteoarthritic changes usually occur in the central to posterior aspect of the lateral tibial plateau, regardless of whether the changes are due to valgus malalignment or ACL deficiency or occur after meniscectomy. Early joint space narrowing with peripheral osteophyte formation may be noted in a standing AP x-ray film; however, the standing 45-degree Rosenberg PA x-ray film usually demonstrates loss of articular space and always should be included (Figure 3–4).1
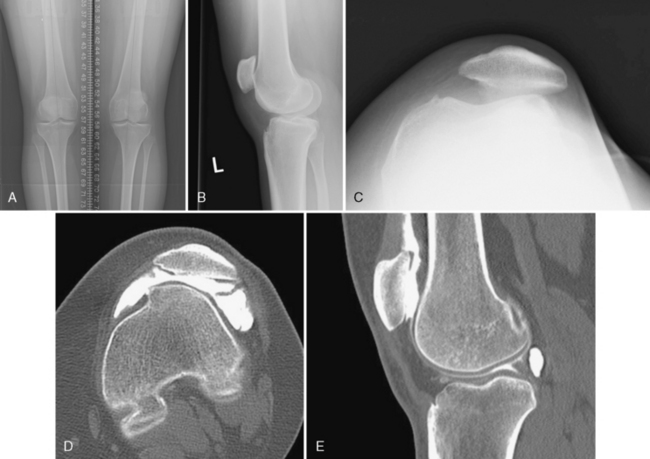
Dysplasia and Degenerative Osteoarthritis of the Patellofemoral Joint
Just as dysplasia of the hip joint results in early osteoarthritis secondary to abnormal contact forces in patients in their early 40s and 50s, a similar condition exists in the patellofemoral joint. Dysplasia of the trochlea has been discussed in Europe, especially France, since the 1970s but has just started being recognized in the United States in the last decade. Dejour4 has done much work demonstrating the radiographic abnormalities present in a patient with dysplasia of the trochlea (Figure 3–5). Dysplasia may present as a poorly formed or flattened sulcus or a convex trochlea (see Chapter 10). The lateral x-ray film does not demonstrate the “crossing sign,” which is characteristic of a patient with dysplasia, because a poorly formed sulcus does not show a double dip on lateral x-ray film. These patients frequently present with an adolescent dislocation of the patella, anterior knee pain, or both. The pain may persist through young adulthood and by the fourth or fifth decades presents with end-stage patellofemoral isolated osteoarthritis (see Figure 3–5).