6
Imaging Techniques of Cartilage Injury
CHRISTINE B. CHUNG, AUREA MOHANA-BORGES, AND DONALD L. RESNICK
By the year 2020, arthritis will have the largest increase in number of new patients of any disease in the United States, making the symptomatic degeneration of articular cartilage among the most prevalent chronic conditions encountered. Not only is it a significant cause of morbidity in affected patients, it is second only to heart disease in causing work disability. The direct traditional medical costs and indirect economic and wage loss from arthritis in the United States has reached in excess of $65 billion annually.1
Although arthroscopy has been the gold standard for diagnosing and monitoring cartilage damage and repair, this is less than optimal, for several reasons: It is both invasive and expensive. Moreover, this method relies largely on visual inspection of the articular surface to indicate the need for further evaluation by physically probing the cartilage surface to find abnormalities in texture or hidden defects within the midsubstance of the tissue.
Though several imaging methods exist for cartilage evaluation, magnetic resonance imaging (MRI) has emerged as the imaging method of choice due to its excellent soft tissue contrast and multiplanar imaging capabilities. MRI has proven both sensitive and specific in the diagnosis of high-grade cartilage lesions (those involving partial- or full-thickness lesions). The limitations of MRI lie in the detection of early degenerative change in the cartilage that heralds the presence of structural alteration at the macromolecular level. It is detection of abnormality at this level that will ultimately further the understanding of the etiology and progression of cartilage lesions, and begin an era of prevention of osteoarthritis, rather than palliation.
This chapter focuses on existing, widely available MRI techniques, as well as advances in the MRI evaluation of articular cartilage.
 Magnetic Resonance Imaging of Articular Cartilage
Magnetic Resonance Imaging of Articular Cartilage
The general goal of imaging is the accurate depiction of the structure and composition of a tissue to evaluate its integrity. The imaging of articular cartilage proves particularly challenging in this respect due to its zonal changes in structure and biochemical composition over the distance of a few millimeters.
It is for these reasons that the normal MRI appearance of articular cartilage remains a controversial and debated issue, particularly with respect to its structure. It is generally accepted that high-resolution MRI of articular cartilage demonstrates a multilaminar appearance. The departure from and subsequent details of this finding become more complex in almost every aspect. There is much variability in both the number of laminar layers that have been reported to occur in articular cartilage and the signal characteristics of those layers. Moreover, the exact designation of what the layer represents is also debated. Although some studies advocate the hypothesis that the layers reflect the zonal anatomy of this tissue, others emphasize the contribution of truncation artifact in producing this multilaminar appearance.2–5 In either case, the disruption of the multilaminar pattern suggests an irregularity in the structure of the tissue.
The composition of articular cartilage, chondrocytes within an extracellular matrix composed primarily of water, collagen, and proteoglycans, is perhaps less controversial. Although the exact ratio of each of the above demonstrates zonal variability, the overall composition explains the general signal characteristics that will be discussed with the individual imaging sequences.
 Current Clinical Magnetic Resonance Imaging Applications
Current Clinical Magnetic Resonance Imaging Applications
T1-Weighted Spin-Echo Images
One common way to evaluate tissue with MRI is by its intrinsic relaxation times, T1 and T2, which are a reflection of the local tissue properties. T1-weighted spin-echo sequences were initially advocated due to their excellent anatomic detail and high contrast between cartilage and subchondral bone.6 This is an imaging sequence in which the range of contrast is bordered by bright or high signal intensity seen in fatty tissues such as bone marrow, and by dark or low signal intensity seen in osseous cortex. The signal intensity characteristics of articular cartilage are isointense to muscle or intermediate as compared with the internal standards of fat and cortex. Normal cartilage on this imaging sequence demonstrates homogeneous signal intensity with no multilaminar appearance. Though focal defects are identified by intrasubstance signal hypointensity, the suboptimal contrast between joint fluid (also isointense to muscle) and articular cartilage makes identification of surface irregularity and focal defects difficult.
T2-Weighted Spin-Echo Images
In the T2-weighted image, the borders of the range of contrast include fluid-like signal intensity that appears very bright (high in signal intensity) whereas osseous cortex appears dark (low in signal intensity). Both muscle and fat are intermediate in signal. T2-weighted images capitalize on the arthrogram-like effect produced by the high signal intensity of joint fluid, which accentuates any surface irregularity or focal defect in the articular cartilage.7–9 As with Tl-weighted images, the cartilage demonstrates homogeneous signal intensity in its normal state. Signal alterations generally consist of globular regions of increased signal intensity (Fig. 6–1). The disadvantages of T2-weighted images include decreased spatial resolution as compared with Tl-weighted images, a lack of contrast between cartilage and subchondral cortical bone, and insensitivity to the intrinsically short T2 relaxation time of the zones of cartilage. In addition, T2-weighted sequences are particularly susceptible to an artifact that produces increased signal in highly ordered structures. This artifact is referred to as the magic angle effect and is maximal when the structure imaged is oriented at 55 degrees to the main magnetic field.5

FIGURE 6–1 Coronal T2-weighted [repetition time (TR) 2367, echo time (TE) 90] fat-suppressed fast spin-echo image through the knee demonstrates an area of contour irregularity (arrow) of the lateral aspect of the medial femoral condyle. In addition, there is heterogeneous signal intensity in the cartilage in this region.
Fat Suppression and Fast Spin-Echo Sequences
The application of two techniques in image acquisition for evaluation of articular cartilage has proven quite important in optimizing its evaluation. The first is the utilization of fast spin-echo imaging techniques. These techniques allow improved efficiency in image acquisition with an increase in the signal-to-noise ratio (hence increased spatial resolution) and a decrease in imaging time, which can result in a decrease in motion artifact. Fast spin-echo sequences also introduce the magnetization transfer effect, which results in improved contrast between articular cartilage and adjacent tissues, as well as between normal and abnormal cartilage. With this in mind, it is logical that chondral defects are detected primarily as focal regions of signal abnormality.10–12
The second adaptation that has proven quite useful in cartilage evaluation is the addition of fat suppression to Tl-weighted images. By suppressing fat, the gray scale of Tl-weighted images is reset to include a much narrower range of values, allowing more contrast across the image, hence better delineation between cartilage and synovial fluid. In addition, fat suppression also eliminates chemical-shift artifacts that can distort the cartilage—bone interface.13,14
T1-Weighted Fat Suppressed Three-Dimensional Spoiled Gradient Echo Sequences
The augmentation of T1 contrast by fat suppression can be combined with high spatial resolution and a greater signal-to-noise ratio by using a three-dimensional gradient-echo (3D spoiled GRE) technique. This technique allows the acquisition of thin section images with high contrast between bright cartilage and surrounding tissues, which can be reformatted into multiple planes. The cartilage has relatively high signal intensity due to the Tl-weighting (Fig. 6–2). The intrinsic signal intensity in the cartilage is homogeneous, with the exception of a midline low signal intensity pseudolamina, believed to be produced by truncation artifact, not the zonal anatomy of cartilage demonstrated on higher resolution images. This artifact occurs at the junction of two abrupt interfaces such as cartilage and bone, and is the result of undersampling of high spatial resolutions. Chondral defects are detected primarily as regions of altered morphology rather than as areas of signal abnormality. This is currently the most sensitive clinical application for cartilage evaluation readily identifying higher grade lesions.15,16
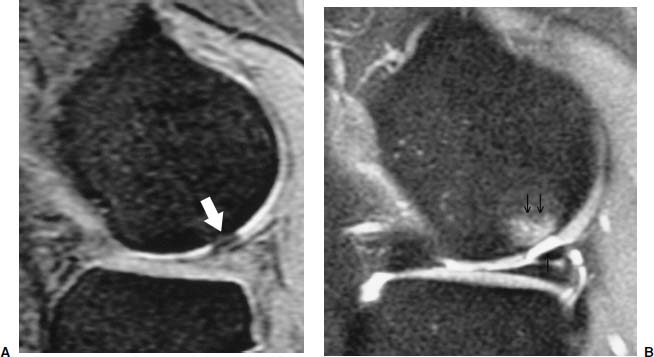
FIGURE 6–2 (A) Sagittal three-dimensional spoiled gradient recalled image (TR 60, TE 5, flip angle 50 degrees, slice thickness 1.5 mm) through the lateral femoral condyle demonstrates a focal full thickness (arrow) chondral defect. (B) Corresponding sagittal proton density weighted (TR 4000, TE 15, slice thickness 4 mm) fat-suppressed fast spin-echo image through the lateral femoral condyle also shows the full-thickness (single arrow) chondral defect. The edema (double arrow) in the subchondral bone is more prominent on this image.
Postarthrography Imaging
Postarthrography imaging capitalizes on the idea that fluid in an articulation can fill cartilage fissures and tears. In this instance, a high image contrast-to-noise ratio between joint fluid and other tissue can be very useful for diagnoses of cartilage damage or injuries. This high image contrast-to-noise has been achieved by both magnetic resonance (MR) arthrography, and more recently computed tomographic (CT) arthrography.
In the case of MR arthrography, a solution of a gadolinium-based contrast agent diluted to a 1 mmol/L concentration with normal saline is placed in the articulation under fluoroscopic guidance. MRI is subsequently performed using T1-weighted fat-suppressed sequences. This distention of the articulation with contrast allows optimal visualization of the articular surface contour (Fig. 6–3). Despite the increase in the dynamic range of contrast in the articular cartilage offered by fat suppression, the T1-weighted image does not allow detection of internal signal changes within the cartilage.17
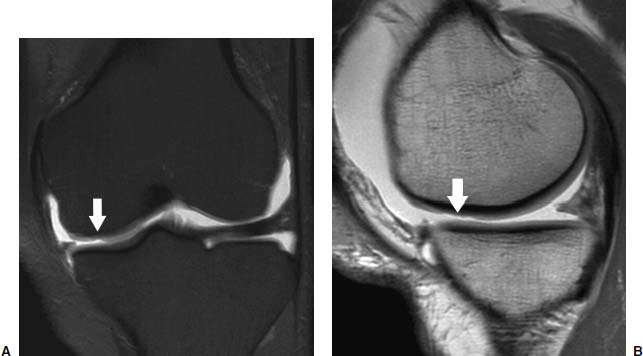
FIGURE 6–3 (A) Coronal T1-weighted (TR 616, TE 16) fat-suppressed fast spin-echo MR arthrogram image of the knee demonstrates a partial-thickness cartilage defect (arrow) in the weight-bearing surface of the medial femoral condyle. (B) Corresponding proton density weighted (TR 2900, TE 30) fast spin-echo MR arthrogram image shows the partial-thickness lesion.
More recently the technique of CT arthrography, using dual-detector spiral scanners, has been introduced for the evaluation of surface cartilage lesions. Similar to MR arthrography, a contrast solution is placed into the articulation. With CT arthrography, the contrast solution is iodine based. A recent study has reported accurate assessment of a surface cartilage lesion (Fig. 6–4). Moreover, no statistically significant difference between spiral CT arthrography and MRI in sensitivity and specificity for surface lesions was demonstrated.18

FIGURE 6–4 (A) Coronal three-dimensional spoiled gradient recalled image (TR 600, TE 24, flip angle 30 degrees, slice thickness 3.0 mm) through the knee demonstrates a region of focal high signal intensity (arrow) in the lateral tibial plateau. (Courtesy of Bruno C. Vande Berg, Hopital St. Luc, Brussels, Belgium.) (B) Corresponding helical dual detector computed tomographic (CT) arthrogram image better characterizes the focal cartilage lesion (arrow) that involves greater than 50% of the overall cartilage thickness. (Courtesy of Bruno C. Vande Berg, Hopital St. Luc, Brussels, Belgium.)
The intrinsic benefit of CT with respect to MRI is the superior resolution afforded by CT, as well as its availability for patients who cannot undergo MRI studies because of claustrophobia, a pacemaker, etc. The disadvantage for CT is the relative poor soft tissue contrast as compared with MRI that precludes evaluation of intrinsic cartilage lesions. The obvious disadvantage of both CT and MR arthrography is the invasive nature of the studies.
Quantitative Imaging Volume Measurement
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


