Osteochondritis dissecans (OCD) is a localized process that affects the subchondral bone and can progress to the overlying articular cartilage. The cause of this lesion remains elusive. With the vague clinical symptoms and signs of OCD, imaging plays a vital role in making the diagnosis and helping with the prognosis of OCD lesions. This article reviews current imaging modalities for the assessment of OCD including conventional radiography, nuclear medicine, computed tomography (CT), CT arthrography, magnetic resonance (MR) and MR arthrography. The role of imaging in evaluating healing of the OCD and articular congruity after surgical and nonsurgical management is discussed.
Osteochondritis dissecans (OCD) is an uncommon, localized process that affects the subchondral bone and can result in delamination and destabilization of the overlying articular cartilage. This condition has been seen with increased frequency as children of younger age are participating in more competitive sports. The incidence of OCD has been estimated to be between 0.02% and 0.03% by radiography, and as high as 1.2% by arthroscopy. Prevalence of this condition ranges between 15 and 29 per 100,000, with an increased male predominance of 2:1. The knee is the most common location for OCD and the condition is bilateral in 15% to 30% of cases. The classic location for OCD in the knee is the posterolateral aspect of the medial femoral condyle (69%). Less common locations include the lateral femoral condyle (15%), patella (5%), and femoral trochlea (1%). Although not the focus of this discussion, other joints that can be affected include the ankle, elbow, hip, and wrist.
The etymology of the term osteochondritis dissecans is worthy of discussion. The itis suffix of osteochondritis denotes the previously understood cause of inflammation of the osteochondral joint surface. Dissecans is derived from Latin and means to separate. Franz Konig introduced the term osteochondritis dissecans in 1888, although it was originally described by Paget some years earlier.
Although many researchers have attempted to determine the cause of OCD, there remains considerable debate and no clear consensus. Hereditary, traumatic, and vascular causes have been proposed, with conflicting evidence supporting each. The ultimate cause of OCD lesions is unknown at this time, but is likely multifactorial, with mechanical causal factors being most important.
Clinical presentation
Early presentation of OCD often consists of vague pain in and around the knee. The pain is worse with activity and can be associated with an antalgic, externally rotated gait. If the lesion is unstable, mechanical symptoms may be present. On evaluation of the knee, the clinician may notice atrophy of the quadriceps and pain with range of motion. The Wilson test is a special provocative test that has been described with attempts to impinge the tibial spine on the OCD lesion. This test has more recently been shown to lack a satisfactory sensitivity and specificity, but can be used as a test after treatment to assess for clinical healing.
Imaging work-up
Because of the nonspecific nature of the clinical signs and symptoms of OCD, imaging plays a central role in the diagnosis and prognosis of this disease. The role of the different imaging modalities has evolved with time. Imaging modalities used for assessment of OCD include conventional radiography, nuclear medicine, computed tomography (CT), CT arthrography, magnetic resonance imaging (MRI), and magnetic resonance (MR) arthrography.
Conventional Radiography
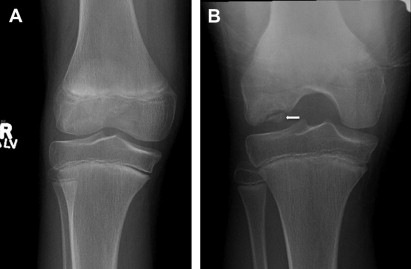
Conventional radiographs allow determination of the size and location of the lesion as well as assessment of the skeletal maturity of the patient. Initial radiographic evaluation of patients with suspected OCD should include anterior-posterior (AP), lateral, tunnel, and skyline views. The tunnel view provides improved visualization of the posterior aspect of the femoral condyle as it is brought into view with knee flexion ( Fig. 1 ). The skyline view allows for visualization of the femoral trochlea, an uncommon but problematic location for OCD lesions. Imaging of the contralateral knee should be considered if symptoms warrant it.
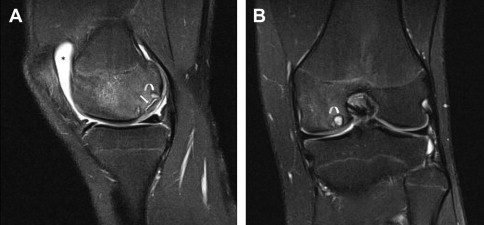
Characteristic radiographic findings include a well-circumscribed area of subchondral bone separated by a crescent-shaped radiolucent outline of the fragment. Although the radiographic examination can establish the diagnosis of OCD correctly, it is not adequate for prognostic and therapeutic decisions. This limitation is often caused by discrepancies between surgical and radiographic manifestations of the disease. Discrepancies include underestimation of fragment size, or fragments that appear radiographically separated can be covered by normal cartilage at surgery, and vice versa ( Fig. 2 ). In general, conventional radiographs are poor at establishing the stability and size of the lesion and are unable to assess the status of the overlying cartilage. In addition, radiographs may not always show OCD lesions consistently or definitively.

Bone Scan
Nuclear medicine technetium-99m methylene diphosphonate (MDP) bone scans have been investigated and used as a potential dynamic study to evaluate the healing potential of OCD defects. In comparison with radiography, scintigraphy has superior sensitivity to changes in the stability of OCD lesions. This technique was initially thought useful in determining the need for operative intervention for lesions that show increased activity on bone scan despite conservative treatment. Another proposed advantage of scintigraphy is its ability to differentiate anomalies of ossification versus true OCD, with ossification anomalies having minimal, if any, increased radiotracer uptake.
With radionuclide scanning, findings between stable and unstable fragments overlap. Bone scintigraphy also provides no anatomic information on articular surface deformity. Hence, although bone scintigraphy can serve to localize a lesion to a specific joint, it often offers little specificity in distinguishing OCD lesions from other joint abnormalities. Bone scintigraphy has not been shown to provide reliable information about an OCD lesion’s stability; as such, it has limited usefulness in differentiating surgical versus nonsurgical lesions. In addition, bone scintigraphy requires exposure to ionizing radiation, can be time consuming, and requires an intravenous injection.
CT
CT offers excellent anatomic delineation of mineralized/ossified structures within the knee joint. However, conventional CT is poor at assessing articular cartilage and other noncalcified aspects of a joint. As such, conventional CT is limited in providing diagnostic information regarding OCD lesion stability or healing potential.
In contrast with conventional CT, CT arthrography has been used for cartilage imaging, providing reliable information regarding the integrity of articular cartilage overlying an OCD lesion. CT arthrography consists of thin-slice CT evaluation following intra-articular administration of iodinated contrast. The introduction of spiral CT has provided the additional ability to obtain thin, overlapping CT sections with excellent secondary sagittal and coronal reformations. This evolution has resulted in a resurgence of CT arthrography for the assessment of intra-articular lesions, including OCD lesions. However, given the young demographics of the typical OCD patient, the ionizing radiation associated with CT scanning has tempered widespread adoption.
MRI
MRI has been shown to be an ideal diagnostic technique for evaluation of OCD lesions because of its noninvasive nature, absence of ionizing radiation, excellent anatomic detail, and soft tissue contrast allowing cartilage visualization.
MRI has been shown to be diagnostically valuable in the differentiation of variations in ossification from true OCD lesions. Ossification variability is typically seen as irregularity in the farposterior condyles without intercondylar extension, and without associated edema ( Fig. 3 ). In contrast, true OCD lesions on MRI are seen as defects in the posterior femoral condyles with intercondylar extension and significant edema.

MRI is now commonly used to evaluate and confirm the presence of an OCD lesion but, more importantly, to assess stability of OCD lesions of the knee. Stability is the most important prognostic factor for determining the likelihood of an OCD lesion healing with nonoperative therapy.
Multiple studies have described the MRI findings in patients with stable and unstable OCD lesions. There are 4 widely used MRI criteria for OCD instability that were described by De Smet and colleagues ( Fig. 4 ). These MRI criteria include (1) a rim of high signal intensity surrounding an OCD lesion on T2-weighted images (hereafter referred to as high T2 signal intensity), (2) cysts surrounding an OCD lesion, (3) a fracture line of high T2 signal intensity extending through the articular cartilage overlying an OCD lesion, and (4) a fluid-filled osteochondral defect.
Despite the popularity of these criteria, there is no apparent consensus in the literature regarding the most appropriate MRI criteria for defining OCD instability. The widespread difference of opinion may relate to a lack of distinction between the juvenile and adult forms OCD and the potentially different imaging features of stability/instability seen between juvenile and adult forms of the disease.
Recently, Kijowski and colleagues proposed revised criteria for OCD instability based on skeletal maturity of the patient. In a study of 32 skeletally immature patients using arthroscopy as the reference standard, Kijowski and colleagues found that the presence of T2 signal intensity rim or cysts surrounding an OCD lesion may be a sign of instability only in adults. In their cohort of juvenile patients, a rim of high T2 signal intensity surrounding an OCD lesion indicated instability only if it had the same signal intensity as adjacent joint fluid, was surrounded by a second outer rim of low T2 signal intensity ( Figs. 5 and 6 ), or was accompanied by multiple breaks in the subchondral bone plate. Cysts surrounding a juvenile OCD lesion indicated instability only if they were multiple or large (>5 mm) in size.
The De Smet criteria initially revealed a sensitivity and specificity of 92% and 90% respectively for differentiating unstable lesions from stable lesions. However, subsequent studies using the revised criteria of Kijowski and colleagues showed sensitivities and specificities approaching 100%.
Some investigators have also recommended using direct MR arthrography for evaluating patients with OCD, looking for signs of instability and differentiation of partial versus complete separation of fragments indicated by contrast subsiding the OCD fragment ( Fig. 7 ). Direct MR arthrography also provides advantages of distention, increased intra-articular pressure from the fluid volume, and increased signal/noise ratio on T1-weighted imaging. However, these advantages come at the cost of converting a noninvasive examination (conventional MRI) to an invasive procedure, and there are the potential complications inherent to intra-articular injection of contrast material.
MRI Sequences/Protocol
An ideal MRI protocol for accurate assessment of OCD lesions and OCD repair should provide accurate assessment of cartilage thickness, signal changes within cartilage, the cartilage and bone interface, and the subchondral bone. It should also provide valuable information about articular cartilage repair tissue after surgery.
There are multiple existing and developing MRI pulse sequences that are valuable in assessment of osteochondral lesions. Two classes of pulse sequence acquisition have been most widely used in this regard: intermediate and T2-weighted fast spin echo (FSE) techniques, and three-dimensional (3D) spoiled gradient echo (SPGR) or fast low-angle shot (FLASH) sequences.
Fat-suppressed 3D SPGR and FLASH acquisitions provide high-resolution images with high contrast between the bright cartilage and dark fluid, bone, fat, and muscle. In these sequences, cartilage abnormalities are seen as morphologic abnormalities of contour. Potential limitations of such sequences include their long acquisition times as well as their susceptibility to metal artifacts, which may be an important consideration after surgery.
Intermediate-weighted and T2-weighted FSE acquisitions provide high-resolution, high-contrast imaging of articular cartilage in a short acquisition time. Intermediate-weighted FSE imaging combines T2 weighting and relative fatty marrow signal preservation to generate images with bright joint fluid and subcortical bone marrow. This process results in an arthrogramlike effect and highlights the usually low-intermediate signal cartilage. The addition of fat saturation to FSE techniques can help in the evaluation of articular cartilage by optimizing the dynamic range of the images. FSE imaging also allows diagnostic evaluation of other intra-articular structures, including subchondral bone. Fluid-sensitive (T2) sequences should be obtained in all 3 standard planes. For example, OCD involving the trochlear sulcus is best evaluated on axial and sagittal images.
MRI Higher Field Imaging and Advanced Techniques
MRI at 3.0 T has the potential advantage of imaging with higher spatial resolution at similar imaging acquisition times, compared with 1.5-T imaging. This higher resolution may in turn improve diagnostic accuracy. These higher field strength scanners are increasingly available in clinical practice; however, randomized controlled trials are necessary to evaluate the diagnostic efficacy of this new technology.
Emerging MRI sequences have shown great potential for the physiologic assessment of cartilage repair tissue. The main quantitative sequences are T2 mapping and delayed gadolinium contrast-enhanced MRI of cartilage (dGEMRIC). Quantitative T2 mapping has been correlated with type II collagen matrix organization within normal hyaline articular cartilage. The dGEMRIC imaging technique, which displays the distribution of negatively charged gadolinium-based MRI contrast material (gadopentetate dimeglumine) within cartilage, has been validated as an accurate marker of cartilage tissue glycosaminoglycan (GAG) concentration. These techniques have been investigated as potential tools to characterize the histologic and biochemical composition and temporal maturation of repair tissue following osteochondral repair procedures. However, the clinical usefulness of these quantitative techniques remains uncertain.
Imaging work-up
Because of the nonspecific nature of the clinical signs and symptoms of OCD, imaging plays a central role in the diagnosis and prognosis of this disease. The role of the different imaging modalities has evolved with time. Imaging modalities used for assessment of OCD include conventional radiography, nuclear medicine, computed tomography (CT), CT arthrography, magnetic resonance imaging (MRI), and magnetic resonance (MR) arthrography.
Conventional Radiography
Conventional radiographs allow determination of the size and location of the lesion as well as assessment of the skeletal maturity of the patient. Initial radiographic evaluation of patients with suspected OCD should include anterior-posterior (AP), lateral, tunnel, and skyline views. The tunnel view provides improved visualization of the posterior aspect of the femoral condyle as it is brought into view with knee flexion ( Fig. 1 ). The skyline view allows for visualization of the femoral trochlea, an uncommon but problematic location for OCD lesions. Imaging of the contralateral knee should be considered if symptoms warrant it.
Characteristic radiographic findings include a well-circumscribed area of subchondral bone separated by a crescent-shaped radiolucent outline of the fragment. Although the radiographic examination can establish the diagnosis of OCD correctly, it is not adequate for prognostic and therapeutic decisions. This limitation is often caused by discrepancies between surgical and radiographic manifestations of the disease. Discrepancies include underestimation of fragment size, or fragments that appear radiographically separated can be covered by normal cartilage at surgery, and vice versa ( Fig. 2 ). In general, conventional radiographs are poor at establishing the stability and size of the lesion and are unable to assess the status of the overlying cartilage. In addition, radiographs may not always show OCD lesions consistently or definitively.








