Juvenile idiopathic arthritis is a broad term used to describe a series of chronic arthritis occurring in children younger than 16 years of age. Even though the cause is not fully understood, several clues regarding the pathogenesis have been found. Diagnosis of the different types of juvenile idiopathic arthritis is made clinically, and imaging plays a role in answering specific questions pertaining to disease classification, staging, and outcome of treatment options.
Juvenile idiopathic arthritis (JIA) is a broad term that includes all forms of arthritis of unknown cause with onset before 16 years of age and that persist for at least 6 weeks in children and adolescents. A diagnosis of JIA is based mainly on clinical findings rather than on laboratory tests or imaging findings. Although the hallmark of all subtypes of JIA is synovial inflammation, the pathogenesis of each subtype differs. No imaging protocols have yet been established for JIA; however, a familiarity with imaging modalities and their indications proves helpful when attempting to answer specific questions to better define, classify, and treat patients with JIA.
Epidemiology
JIA is the most common chronic rheumatologic childhood disease, with an onset before 16 years of age and persisting for at least 6 weeks. It occurs in a worldwide distribution with regional variations thought to be due to differences in the distribution of HLA alleles and environmental factors. Among developed nations, JIA has a yearly incidence rate of 2 to 20 cases per 100,000 population and a prevalence of 16 to 150 cases per 100,000 population. In a comprehensive survey of data from 2002, the incidence of chronic arthritis of childhood ranged from 0.008 to 0.226 per 1000 children and the prevalence from 0.07 to 4.01 per 1000 children worldwide. The true incidence of JIA is believed to vary widely, however, in part because it is composed of a heterogeneous group of arthritic conditions that are clinically diagnosed. In a multiethnic cohort study by Saurenmann and colleagues, European ancestry was shown an important predisposing factor for developing all types of JIA, in particular the oligoarticular and psoriatic subtypes, except the rheumatoid factor (RF)-positive polyarticular type. In this study, native North American children were also found at a higher risk of developing polyarticular disease than children of European descent.
Classification
JIA is a broad term that was developed by the International League of Associations for Rheumatology (ILAR) to group chronic arthritis in patients younger than 16 years of age for research purposes. This task force created relatively homogeneous, mutually exclusive categories of JIA based on clinical findings, replacing the terms, juvenile chronic arthritis and juvenile rheumatoid arthritis . JIA encompasses a heterogeneous group of diseases classified into 7 subtypes according to age of onset, number of affected joints, presence of RF and HLA-B27, and clinical findings. These 7 subtypes are systemic arthritis, oligoarthritis, polyarthritis (RF positive), polyarthritis (RF negative), enthesis-related arthritis (ERA), psoriatic arthritis, and undifferentiated arthritis ( Box 1 ) .
Systemic arthritis
Oligoarthritis
Polyarthritis (RF positive)
Polyarthritis (RF negative)
Enthesis-related arthritis
Psoriatic arthritis
Undifferentiated arthritis
Systemic Juvenile Idopathic Arthtitis
Systemic JIA (sJIA) constitutes a small proportion (10%) of JIA but contributes to approximately two-thirds of the total mortality rate of JIA. sJIA has a prevalence of 3.5 per 100,000 and the range of incidence is between 0.4 and 0.9 per 100,00. sJIA is characterized by a preceding fever of at least 2 weeks’ duration and an association with one of the following: rash, lymphadenopathy, hepatosplenomegaly, or serositis. It demonstrates no gender predilection. The number of joints affected in patients with sJIA varies, and the arthritis may develop after the systemic symptoms have subsided. Although by definition, sJIA can present at any age before age 16 years, in a recent study, Behrens and colleagues reported that from a total of 136 patients, 74 presented with sJIA between 0 and 5 years of age with 2 years old the most common age at presentation (n = 7). Patients affected with sJIA characteristically display early joint destructive changes and ankylosis.
Oligoarthritis
Oligoarthritis is a term used to describe arthritis affecting 1 to 4 joints during the first 6 months of disease. Three exclusion criteria for a diagnosis of oligoarthritis are family history of psoriasis/spondyloarthropathy, positive RF, and presence of HLA-B27. Oligoarthritis is divided into 2 subcategories, persistent and extended types. The persistent type of oligoarthritis affects no more than 4 joints over the course of the illness and is more common in girls younger than 6 years of age. Monoarthritis is seen in 50% of the affected patients with the knees, ankles, and elbows as the most frequently affected joints in these children. The extended type of oligoarthritis affects more than 4 joints after the first 6-month period. This subtype has a poorer prognosis than the persistent type, because more than 50% of affected patients develop the active disease in their adulthood. A characteristic clinical feature of the extended type of oligoarthritis of JIA is the increased risk of iritis, especially in girls with positive antinuclear antibodies (ANAs). In North America and Europe, oligoarticular disease accounts for 30% to 60% of JIA cases.
Polyarthritis
Polyarthritis is a term designated for arthritis that affects 5 or more joints during the first 6 months of disease. The 2 subtypes of polyarthritis are RF positive and RF negative, the former accounting for 5% to 10% and the latter 10% to 30% of all JIA. In order to establish a definite diagnosis of the RF-positive subtype of polyarthritis, it must be confirmed on 2 separate occasions that are at least 3 months apart. The RF-positive subtype of polyarthritis often begins in late childhood or adolescence and is similar to adult rheumatoid arthritis with respect to clinical presentation and pathogenesis; however, the effects on the growing skeleton (accelerated or delayed growth) make up the major difference.
Enthesis-Related Arthritis
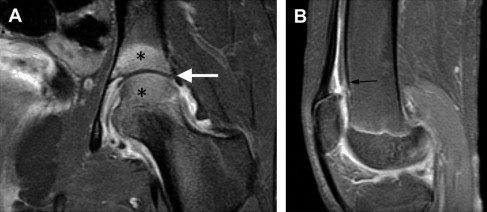
ERA is a subtype of arthritis that may be present alongside oligoarthritis or polyarthritis, affecting large or small joints as well as entheses. In addition, at least 2 of the following conditions must be present: sacroiliac pain, inflammatory lumbosacral pain, acute anterior uveitis, positivity for the HLA-B27 antigen, family history of uveitis, ankylosing spondylitis, Reiter syndrome or inflammatory bowel disease, and onset of oligoarthritis in boys over 6 years of age. Because ERA often begins as an undifferentiated disease in pediatric patients with an initial clinical presentation that differs significantly from that in adults, a definite diagnosis is frequently delayed. In contrast to adult patients with ERA, back pain is typically lacking in children with ERA and more cases of enthesopathy with knee and hip involvement are found in children ( Fig. 1 ). Using the ILAR classification, most childhood spondyloarthropathies are classified as ERA and the presence of, or a family history, of psoriasis is an exclusion criterion, which differs from criteria of adult patients with ERA.
Psoriatic Arthritis
Psoriatic arthritis is a subtype of JIA that is currently diagnosed when arthritis occurs in the presence of psoriasis or the presence of 2 of the following in conjunction with arthritis: a family history of psoriasis in a first-degree relative, dactylitis, and nail changes. The presence of RF is an exclusion criterion for a diagnosis of psoriatic arthritis. Accounting for approximately 5% of JIA, psoriatic arthritis tends to affect girls more frequently than boys and often begins earlier in childhood. It is still debated whether this subtype should be regarded as an entirely separate entity due to a heterogeneously distinct profile in children with early-onset and late-onset types. The early-onset type of psoriatic arthritis peaks at age 2 to 3 years, is more common among girls, and tends to be ANA positive with clinical features similar to oligoarticular/polyarticular JIA. The late-onset type of psoriatic arthritis, alternatively, peaks at approximately 10 to 12 years and is accompanied by features typical of spondyloarthritis, such as male predominance, HLA-B27 positivity, enthesis, and axial skeletal involvement. Both types of psoriatic arthritis are accompanied by a high frequency of dactylitis and arthritis that may precede skin manifestations.
Undifferentiated Arthritis
A diagnosis of undifferentiated arthritis should be made only after careful evaluation and exclusion of other types of arthritis.
Classification
JIA is a broad term that was developed by the International League of Associations for Rheumatology (ILAR) to group chronic arthritis in patients younger than 16 years of age for research purposes. This task force created relatively homogeneous, mutually exclusive categories of JIA based on clinical findings, replacing the terms, juvenile chronic arthritis and juvenile rheumatoid arthritis . JIA encompasses a heterogeneous group of diseases classified into 7 subtypes according to age of onset, number of affected joints, presence of RF and HLA-B27, and clinical findings. These 7 subtypes are systemic arthritis, oligoarthritis, polyarthritis (RF positive), polyarthritis (RF negative), enthesis-related arthritis (ERA), psoriatic arthritis, and undifferentiated arthritis ( Box 1 ) .
Systemic arthritis
Oligoarthritis
Polyarthritis (RF positive)
Polyarthritis (RF negative)
Enthesis-related arthritis
Psoriatic arthritis
Undifferentiated arthritis
Systemic Juvenile Idopathic Arthtitis
Systemic JIA (sJIA) constitutes a small proportion (10%) of JIA but contributes to approximately two-thirds of the total mortality rate of JIA. sJIA has a prevalence of 3.5 per 100,000 and the range of incidence is between 0.4 and 0.9 per 100,00. sJIA is characterized by a preceding fever of at least 2 weeks’ duration and an association with one of the following: rash, lymphadenopathy, hepatosplenomegaly, or serositis. It demonstrates no gender predilection. The number of joints affected in patients with sJIA varies, and the arthritis may develop after the systemic symptoms have subsided. Although by definition, sJIA can present at any age before age 16 years, in a recent study, Behrens and colleagues reported that from a total of 136 patients, 74 presented with sJIA between 0 and 5 years of age with 2 years old the most common age at presentation (n = 7). Patients affected with sJIA characteristically display early joint destructive changes and ankylosis.
Oligoarthritis
Oligoarthritis is a term used to describe arthritis affecting 1 to 4 joints during the first 6 months of disease. Three exclusion criteria for a diagnosis of oligoarthritis are family history of psoriasis/spondyloarthropathy, positive RF, and presence of HLA-B27. Oligoarthritis is divided into 2 subcategories, persistent and extended types. The persistent type of oligoarthritis affects no more than 4 joints over the course of the illness and is more common in girls younger than 6 years of age. Monoarthritis is seen in 50% of the affected patients with the knees, ankles, and elbows as the most frequently affected joints in these children. The extended type of oligoarthritis affects more than 4 joints after the first 6-month period. This subtype has a poorer prognosis than the persistent type, because more than 50% of affected patients develop the active disease in their adulthood. A characteristic clinical feature of the extended type of oligoarthritis of JIA is the increased risk of iritis, especially in girls with positive antinuclear antibodies (ANAs). In North America and Europe, oligoarticular disease accounts for 30% to 60% of JIA cases.
Polyarthritis
Polyarthritis is a term designated for arthritis that affects 5 or more joints during the first 6 months of disease. The 2 subtypes of polyarthritis are RF positive and RF negative, the former accounting for 5% to 10% and the latter 10% to 30% of all JIA. In order to establish a definite diagnosis of the RF-positive subtype of polyarthritis, it must be confirmed on 2 separate occasions that are at least 3 months apart. The RF-positive subtype of polyarthritis often begins in late childhood or adolescence and is similar to adult rheumatoid arthritis with respect to clinical presentation and pathogenesis; however, the effects on the growing skeleton (accelerated or delayed growth) make up the major difference.
Enthesis-Related Arthritis
ERA is a subtype of arthritis that may be present alongside oligoarthritis or polyarthritis, affecting large or small joints as well as entheses. In addition, at least 2 of the following conditions must be present: sacroiliac pain, inflammatory lumbosacral pain, acute anterior uveitis, positivity for the HLA-B27 antigen, family history of uveitis, ankylosing spondylitis, Reiter syndrome or inflammatory bowel disease, and onset of oligoarthritis in boys over 6 years of age. Because ERA often begins as an undifferentiated disease in pediatric patients with an initial clinical presentation that differs significantly from that in adults, a definite diagnosis is frequently delayed. In contrast to adult patients with ERA, back pain is typically lacking in children with ERA and more cases of enthesopathy with knee and hip involvement are found in children ( Fig. 1 ). Using the ILAR classification, most childhood spondyloarthropathies are classified as ERA and the presence of, or a family history, of psoriasis is an exclusion criterion, which differs from criteria of adult patients with ERA.
Psoriatic Arthritis
Psoriatic arthritis is a subtype of JIA that is currently diagnosed when arthritis occurs in the presence of psoriasis or the presence of 2 of the following in conjunction with arthritis: a family history of psoriasis in a first-degree relative, dactylitis, and nail changes. The presence of RF is an exclusion criterion for a diagnosis of psoriatic arthritis. Accounting for approximately 5% of JIA, psoriatic arthritis tends to affect girls more frequently than boys and often begins earlier in childhood. It is still debated whether this subtype should be regarded as an entirely separate entity due to a heterogeneously distinct profile in children with early-onset and late-onset types. The early-onset type of psoriatic arthritis peaks at age 2 to 3 years, is more common among girls, and tends to be ANA positive with clinical features similar to oligoarticular/polyarticular JIA. The late-onset type of psoriatic arthritis, alternatively, peaks at approximately 10 to 12 years and is accompanied by features typical of spondyloarthritis, such as male predominance, HLA-B27 positivity, enthesis, and axial skeletal involvement. Both types of psoriatic arthritis are accompanied by a high frequency of dactylitis and arthritis that may precede skin manifestations.
Undifferentiated Arthritis
A diagnosis of undifferentiated arthritis should be made only after careful evaluation and exclusion of other types of arthritis.
Pathogenesis
Immune-mediated diseases manifest differently, depending on the underlying abnormalities of the adaptive and innate immune responses. Autoimmunity is the result of immune reactions that are triggered by environmental factors in genetically susceptible individuals. Autoimmune diseases involve the adaptive immune system and are based on antigen-dependent T-lymphocyte and B-cell autoantibody production and have strong associations with the major histocompatibility complex. Alternatively, autoinflammatory diseases causing innate immunity disorders are due to underlying mutations associated with innate immune cells, such as monocytes and neutrophils, rather than to lymphocytes causing immune dysregulation. More recently, an immunologic disease continuum has been proposed, which classifies diseases according to adaptive or innate immune responses, with the majority of diseases involving variable interactions between these 2 systems. Tissue perturbations at target sites of inflammation, rather than the immune system per se, are the key to disease expression.
Oligoarticular/Polyarticular Arthritis
Currently, sufficient evidence supports a distinct pathogenesis of oligoarticular/polyarticular JIA and sJIA. Various known genetic and environmental factors are associated with the development of oligoarticular/polyarticular JIA. With respect to genetic associations, several studies have indicated specific genetic susceptibility with respect to the HLA and non-HLA types. Likewise, environmental factors, such as infectious agents, stress, maternal smoking, and weather changes, as well as vaccination have been associated with the onset or exacerbation of oligoarticular/polyarticular JIA. Oligoarticular/polyarticular JIA is believed to be an antigen-driven, lymphocyte-mediated autoimmune disease. An abnormality in the adaptive immune system, in which an imbalance exists between proinflammatory T cells (Th1 and Th17) and immunosuppressive regulatory T cells (CD4+, which play an important role in immune tolerance to self-antigen), leads to the failure of T-cell tolerance to self-antigens and eventually results in synovitis.
Systemic Idiopathic Arthritis
Systemic idiopathic arthritis is an autoinflammatory disease involving the innate immune system. Unlike with oligoarticular/polyarticular disease, there is no clear association between sJIA and infection, vaccination, or HLA genes. In the early course of the disease process, unknown factors cause loss of control of the alternative secretory pathway (which differs from the classical intracellular transport mechanism), leading to the activation of phagocytes and resulting in the release of proinflammatory cytokines, macrophage colony-stimulating factor, tumor necrosis factor (TNF), and proinflammatory proteins. Such complex underlying interactions are believed to contribute to the multisystemic inflammation seen in sJIA.
Enthesis-Related Arthritis
It is well known that genetics plays a major role in developing ERA. The classic example is patients with ankylosing spondylitis, 80% to 90% of whom are HLA-B27 positive. Not all of those patients are HLA-B27 positive, however, and not every person who has the antigen develops the disease, suggesting other associated factors. Traditionally, ERA has been thought of as an autoimmune disease, in which spondyloarthritis is triggered by gastrointestinal or urologic infections in the presence of HLA-B27– restricted CD8–T-cell clones that are reactive against bacterial antigens and self-proteins from cartilage in the inflamed joint. More recently, an autoinflammatory component of the disease has been suggested, with HLA-B27 playing a role in triggering the innate immune system rather than through antigen presentation. According to this hypothesis, the HLA-B27 molecule may be prone to misfolding within the endoplasmic reticulum of the cell, resulting in the stimulation of the innate immune system, with a greater impact on tissues exposed to either bacterial or mechanical stress, such as the gut and synovium. The concept of a synovial-entheseal complex proposed by Benjamin and McGonagle suggests a relationship between synovial-entheseal complex and spondyloarthropathies. This concept is based on entheses as sites of repeated biomechanical stress that undergo chronic microtrauma, causing the release of fibronectin and other molecules from the injured tissue. These molecules may activate synovial macrophages, resulting in the activation of stress-related genes. Other genetic factors have been identified, such as polymorphism in or near the TNF and interleukin-1 and interleukin-23 loci. These cytokines play an important role in the propagation and perpetuation of inflammation in spondyloarthropathies, providing additional evidence for the innate immune system’s contribution to ERA.
Psoriatic Arthritis
As discussed previously regarding classification of arthritis, there are 2 subtypes of the disease, based not only on different ages of onset but also on the underlying pathogenesis. The disease with the older onset shares features with spondyloarthropathies and, as such, has a similar pathogenesis. Innate immunologic mechanisms likely play a role in the older-onset psoriatic JIA, which typically manifests as inflammation of either the entheses, the intestinal tract, or both and is ultimately responsible for the synovitis. The early-onset subtype of psoriatic arthritis is more likely associated with HLA alleles with early presentation, ANA positivity, and chronic uveitis rather than with HLA-B27. The association suggests that adaptive immunity is more involved than it is in older-onset patients. One feature that remains unexplained is the presence of dactylitis, which is only seen in both subtypes of psoriatic JIA, thus suggesting that both adaptive immunologic and innate autoinflammatory mechanisms are involved in this type of arthritis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





