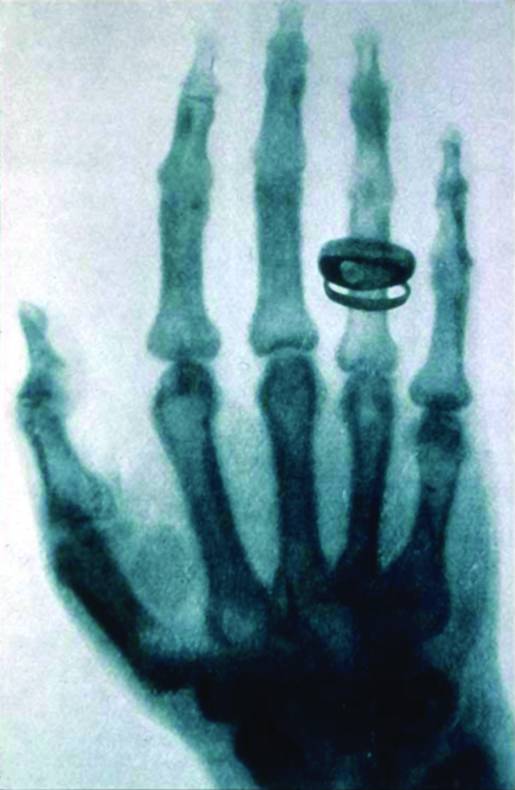
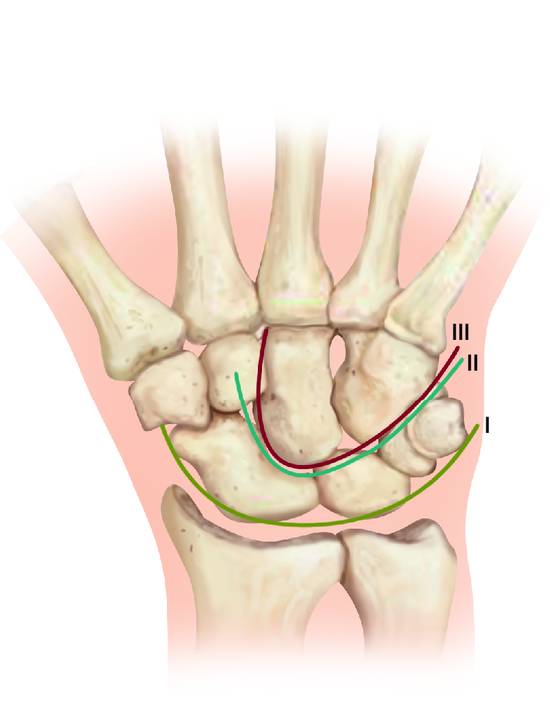
Introduction The first radiograph ever taken was of the hand of Anna Bertha Röntgen in 1895. The following year an image was published of Albert von Kölliker’s hand and wrist (▶ Fig. 4.1) and the same year this new technique was used clinically to diagnose a Colles fracture.1 More than 100 years later radiography is still the main diagnostic tool in wrist imaging but new techniques and other investigations have evolved with time. It started with a simple two-dimensional (2D) picture of the skeleton and now it is possible to create a 3D picture of the wrist including soft tissue2 (▶ Fig. 4.2) and furthermore to visualize activity in the tissue (▶ Fig. 4.3). Fig. 4.1 First X-ray of a hand and wrist by Wilhelm Röntgen. (With kind permission of the Deutsches Roentgen-Museum) Fig. 4.2 CT and cryomicrotomy of a cadaveric specimen visualizing wrist ligaments. (Reprinted from Buijze GA, Dvinskikh NA, Strackee SD, Streekstra GJ, Blankevoort L. Osseous and ligamentous scaphoid anatomy: Part II. Evaluation of ligament morphology using three-dimensional anatomical imaging. J Hand Surg Am 2011;36(12):1936-1943. With permission from Elsevier.) Fig. 4.3 Late phase technetium-99m bone scan visualizing a high uptake in the trapezium bone (fracture). Because the wrist joint has a complex anatomy and is situated in a compact region, it is a challenge to evaluate whether symptoms are intra-articular or extra-articular. Modern imaging consists of many modalities and a targeted interview to clarify the patient’s history together with a careful clinical investigation to guide the use of these imaging tools and help constrain the expense and avoid unnecessary irradiation. The techniques in a wide variety of imaging modalities have different combinations of different properties: Digital radiography (DR) Magnetic resonance imaging (MRI) Computerized tomography (CT) Ultrasonography (US) Technetium-99m bone scintigraphy (BS) Radiography can be either static or dynamic; the dynamic mode may be cineradiography (motion series radiographs) or fluoroscopy (direct dynamic examination). The different modalities can be enhanced by infusion of contrast medium, either systemically (gadolinium in MRI) or intra-articularly (in arthrography) and may be combined as in single-photon emission computed tomography (SPECT) with CT in a fusion of BS and CT (▶ Fig. 4.4). Fig. 4.4 SPECT/CT 3D in a left hand with posttraumatic osteoarthritis in CMC 2 and 5 joint. (Courtesy: Paw Holdgaard.) In modern radiography, X-ray signals are recorded on flat-panel detectors and stored digitally. Fluoroscopes capable of dynamic radiographic recording are available in most hospitals, making wrist investigations in emergency situations (fractures) more accessible and carpal instability diagnostics convenient in the office. MRI is still an expensive investigation but low-field scanning is often adequate to diagnose even minor carpal fractures.3 , 4 When intra-articular ligament injuries are suspected, high-field scanning with thin slices is needed, and when used together with arthrography will be able to diagnose many such injuries. Scanners operating at 7 tesla (7 T) with dedicated wrist coils will in the future probably be able to diagnose the notoriously difficult acutely injured scapholunate (SL) ligament and perform much better in triangular fibrocartilage complex (TFCC) injuries.5 Availability of CT scanners is high and when a fracture is diagnosed multislice scans with 3D reconstruction are helpful to guide the surgeon in choosing the most appropriate treatment in both intra-articular distal radius and carpal fractures.6 , 7 , 8 US is widely available but its usefulness in wrist pathologies is less because of the inability to penetrate to deeper layers beyond the bone surface. However, as the equipment is improved and clinicians become more familiar with its use, the time when US can be used for diagnosing SL ligament injuries and other superficial intra-articular injuries is not far away. Nuclear imaging including SPECT is based on the detection of radioisotopes, typically technetium-99m which is taken up by bone tissue, and images are obtained early and late to detect both the passage through soft tissue and uptake by bone. SPECT can be combined with a CT scanner to provide both functional and anatomical information. The choice of investigations is guided by the patient’s history and the wrist examination and will vary for each individual. Important factors to note before using the imaging protocol include the following: Age, sex, physical condition, profession, sporting activity, musical activity, hobbies Type of trauma, time elapsed Pain, swelling, deformity Loss of motion Locking, clicking, crepitus The most used modalities in wrist injuries are radiography, MRI, and CT. Whenever there has been acute trauma to the hand and wrist, the first line of investigation after clinical evaluation is plain radiography (▶ Fig. 4.5). Fig. 4.5 Standard posteroanterior and lateral projections of the wrist. The concept of Gilula’s lines9 is used to identify signs of subluxation or dislocation and should always be part of the radiographic interpretation in wrist trauma (▶ Fig. 4.6). Any disruption of the lines or overlapping of the bones indicates further investigation to rule out dislocation (▶ Fig. 4.7a, b). Fig. 4.6 Gilula’s three arcs in a normal wrist seen in PA view. (Reproduced from Schmitt, R. and Lanz, U. Bildgebende Diagnostik der Hand; Stuttgart: Hippokrates Verlag; 1996. With kind permission from Hippokrates Verlag.) Fig. 4.7 (a and b) Broken Gilula’s lines and overlapping of the carpal bones indicate a perilunar dislocation in the PA view in the left image which is confirmed in the lateral view on the right. If a certain pathology is suspected, more specific projections are added. In scaphoid view (▶ Fig. 4.8) and radiocarpal view, subtle intra-articular fracture lines will show up. Other special projections are used if there is clinical suspicion of a particular carpal fracture or intrinsic ligament injury.1 Familiarity with the following is useful when using fluoroscopy in the acute situation: Capitate view: A posteroanterior (PA) projection with the X-ray beam angled 30° toward the fingers. Triquetral/pisiform view: A lateral projection with the wrist in 45° of supination. Hamate view: A lateral projection with the wrist in 45° of supination, maximal radial deviation, and the thumb abducted.


Pros: Cheap, good availability, quick, large field of investigation, skeletal advantage, dynamic.
Cons: Radiation, limited projections, double projection, soft tissue not visible.
Pros: Highly sensitive, soft tissue advantage, no radiation.
Cons: Expensive, slow, poor availability, small area coverage, metal artifacts.
Pros: Quick, highly specific, good availability, skeletal advantage, large area coverage.
Cons: Radiation, expensive.
Pros: Cheap, quick, good availability, soft tissue advantage, no radiation, dynamic.
Cons: User-dependent, not reproducible, poor deep penetration, cannot visualize bone/air.
Pros: Relatively cheap, highly sensitive.
Cons: Radiation hazard, slow, poor availability, low specificity.

4.2 The Modalities
4.3 Clinical Use of Imaging


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








