Fig. 7.1
A 27-year-old football player presenting with left calf pain, clinically diagnosed as grade II injury. a On ultrasound at initial presentation, a hypoechoic area measuring 1.0 × 0.4 cm was noted (arrow), corresponding with a partial tear of the medial head of the gastrocnemius (GM). Color Doppler imaging was normal (not shown). No evidence of hematoma or other abnormality was observed. Soleus muscle (SO) appears intact. Magnetic resonance imaging (MRI) was not performed on this patient at this time. b–d Follow-up imaging 2 months after initial presentation. b Axial and c coronal FS T2-w TSE images reveal areas of hyperintensity with feathery appearance, consistent with a partial tear of the medial head of the gastrocnemius muscle with intramuscular edema (arrow). Note the peritendinous edema. d On ultrasound, a persistent hypoechogenic area was noted that appeared to have increased in extent (arrow). Color Doppler imaging was normal (not shown). A 7-month follow-up MRI showed complete recovery (not shown). (From [1] ©Springer)
Ultrasound can also be used as a convenient and inexpensive follow-up study for muscle strains . If symptoms have persisted longer than expected or the appropriate return of function has not occurred, a repeat ultrasound can be performed to assess healing and evaluate for complications. Typically, follow-up studies would be performed in 2–3 week intervals as needed.
In addition to assessing muscle injuries, ultrasound has the added benefit of evaluating for the presence of a deep venous thrombosis (DVT) or a ruptured Bakerʼs cyst; two conditions frequently on the differential diagnosis of posterior leg pain and swelling. Moreover, ultrasound can be used for needle guidance in aspiration of fluid collections associated with muscle injuries in the posterior leg [3].
MRI
Magnetic resonance imaging has been standard for imaging muscle injuries for over a decade. MRI is particularly effective in determining the location, severity, and the extent of muscle injuries in the posterior leg. MRI is also useful in assisting the clinician to objectively predict the time required for an athlete to return to their sport with low risk of injury recurrence, to evaluate for possible complications, surgical planning, and to exclude alternative disorders such as stress fracture. MRI is indicated when the clinical diagnosis is uncertain, the patient has an atypical presentation for muscle injury or when a prompt diagnosis is needed to begin the appropriate initial management [5].
A typical MRI protocol uses a combination of T1- and T2-weighted sequences to emphasize the anatomy and any pathologic edema [3] (Fig. 7.2). T1-weighted images highlight fatty structures (fat planes, lipomas, and muscle atrophy), mature myositis ossificans, degenerative tendon conditions, and aid in the characterization of hemorrhagic lesions (hematomas, contusions, hemorrhagic tumors, etc.). Since T2-weighted images are generally fluid sensitive, they are more sensitive to the accumulation of edema in muscle strain injuries and especially useful in a setting of known trauma. It is important to include both short- and long-axis imaging of the leg with a fat- and water-sensitive sequence for each imaging plane. Sagittal and axial images are especially helpful for distinguishing the anterior and posterior aspects of the leg, as the presence of bony structures aid in anatomic reference. A marker can be used on the patient’s skin to allow the clinician to correlate clinical symptoms with imaging abnormalities. Contrast is rarely used in evaluation of routine muscle injury but should be included if infection, tumor, or myositis is in the differential .
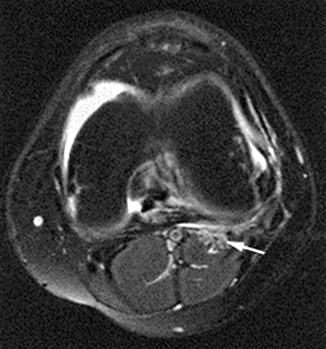
Fig. 7.2
Axial image showing increased fluid signal in the proximal lateral gastrocnemius consistent with a mild strain although the location is somewhat atypical (arrow). (From [3]. Reprinted with permission from Elsevier Limited)
Acute or sub-acute grade I strains demonstrate bright signal on fluid-sensitive sequences illustrating the edema and hemorrhage at the site of injury. Generally, there is less than 5 % involvement of the muscle fibers and a normal appearing myotendinous junction. Grade II strains typically show thinning of the myotendinous junction or muscle fiber disruption in addition to edema and hemorrhage. Grade III strains (high grade or complete tears) show distinct disruption of the muscle-tendon unit with extensive hemorrhage and a wavy appearance of the retracted tendon.
Tennis Leg
“Tennis Leg” is a diagnostic term for muscle injury to the posterior leg . More commonly described today as calf strain , tennis leg has a long and controversial history in the medical literature. It has been described clinically as the sudden onset of sharp pain in the mid-calf during athletics. It most commonly refers to a strain of the medial head of the gastrocnemius and, rarely, the plantaris tendon or soleus muscle . The lack of specificity in the diagnosis of tennis leg stems largely from historical disagreement and the difficulty in being able to differentiate between posterior leg muscle injuries on history and physical exam. Modern imaging and injury classification schemes have made the diagnosis of tennis leg or calf strain antiquated. Should clinical uncertainty about the specificity of the injury exist, both MRI and ultrasound can be used to clarify the location and extent of the injury (Fig. 7.3).
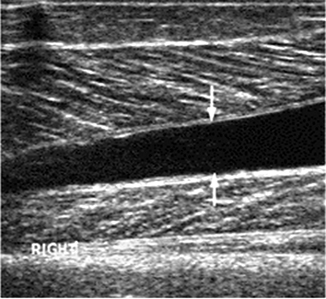
Fig. 7.3
Intermuscular fluid collection between medial gastrocnemius and soleus muscle on ultrasound (arrows) in a patient clinically with tennis leg. (From [3]. Reprinted with permission from Elsevier Limited)
Plantaris Tendon Injury
Injury to the plantaris tendon can clinically mimic a medial head gastrocnemius strain but can be differentiated by imaging. Plantaris tendon ruptures commonly result in an intermuscular fluid collection between the soleus and gastrocnemius with visible retraction of the plantaris muscle appearing as a mass on MRI (8-107) (Fig. 7.4) .
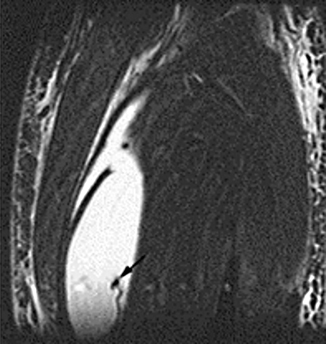
Fig. 7.4
Coronal IR images showing large intermuscular fluid collection between gastrocnemius and soleus muscle as a result of distal plantaris tendon rupture (arrow shows retracted tendon). (From [3]. Reprinted with permission from Elsevier Limited)
Achilles Tendon Injury
Athletes, particularly runners, have a high incidence of Achilles tendon overuse injuries that range from paratendonitis to complete tears [2]. A healthy Achilles tendon appears flat or concave anteriorly except for the focal convexities at the proximal and distal tendon where it is joined with the calf muscles and the calcaneus, respectively. In tendonitis, the tendon volume increases and becomes oval or round in cross section. The plantaris tendon (present in 90 % of people) runs medial to the Achilles tendon prior to its insertion on the calcaneus and should not be mistaken for an Achilles tendon tear , or in the case of a complete tear, not be mistaken for residual intact fibers of the Achilles [2]. MRI or ultrasound can be used to characterize Achilles tendon pathology and diagnosis Achilles tendon tears that are not obvious on physical exam. In a partial tear, fluid signal intensity will be seen within the tendon but can be difficult to distinguish from tendinosis. A tear is more likely if there are findings of edema/hemorrhage surrounding the site of increased signal intensity. The clinician should carefully evaluate any muscle atrophy, underlying tendinosis, and the distance between torn edges of the tendon as each factor will play a role in determining management options. A complete tear will show fiber disruption with a visual gap between the two edges of the retracted tendon. The most common location of Achilles tendon injury is the middle to distal portion and is usually attributed to underlying tendinopathy. Particular attention should also be paid to the insertion site where pain and anterior constriction of the Achilles tendon from a Haglund’s deformity can result in tendinopathy. Posterior constriction of the Achilles tendon can occur from direct compression often aggravated by ill-fitting shoes .
Muscle Contusion
Muscle contusions result from direct trauma that causes a series of events that include microscopic rupture and damage to muscle cells, macroscopic defects in the body of the muscle, infiltrative bleeding, and inflammation. These changes tend to occur deep in the muscle and are often less symptomatic than strains. On ultrasound, contusions are described by discontinuity of the normal musculature with indistinct hyperechogenicity that may cross fascial boundaries [1]. In the acute setting, the muscle appears swollen and may be isoechoic with respect to the unaffected adjacent muscle. If there is moderate to severe trauma, disruptions of muscle fibers occur with associated hemorrhage resulting in hematoma formation. Fluid sensitive MRI findings are characterized by hyperintense signal that may have a diffuse appearance with feathery margins. Unlike strains, the location of the contusion is usually not limited to the myotendinous junction and may result in increase in muscle diameter due to the intramuscular hemorrhage and edema. It should be noted that functional recovery from a contusion tends to precede resolution of abnormalities on MRI .
Table 7.1 describes how the typical appearance of new, old, and recurrent injuries differ between ultrasound and MRI .
Table 7.1
Differentiation between new, old, and recurrent injuries by imaging. (From [1]. ©Springer)
Type of injury | Imaging findings | |
|---|---|---|
MR imaging | Ultrasound | |
New (acute) | ||
Grade I strain | Intramuscular “feathery” hyperintensity on fluid-sensitive sequences without muscle fiber disruption | Areas of intramuscular hyperechogenicity and perifascial hypoechogenicity (fluid collection)
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|




