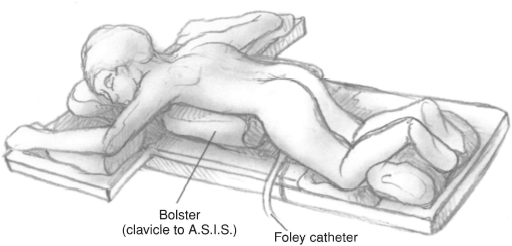
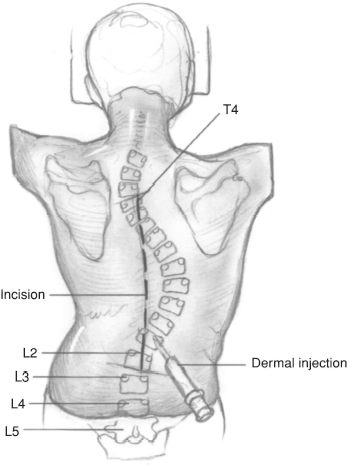
CHAPTER 50 Erik C. King and John J. Grayhack 1. Thoracic curve greater than 50 degrees 2. Thoracolumbar curve greater than 40 degrees 3. Progressive curve greater than 40 degrees in a skeletally immature patient that is associated with significant spinal imbalance or that cannot be controlled with a brace 4. Cosmetically unacceptable spinal deformity 1. Active infection or sepsis (absolute) 2. Anemia 3. Cardiac, pulmonary, or other medical comorbidities that have not been optimally managed 1. Comprehensive physical examination including neurologic testing if indicated 2. Full-length (14 in × 36 in) standing coronal anteroposterior (AP) and sagittal (lateral) radiographs of the thoracic-lumbar-sacral spine. If desired by the surgeon, preoperative supine right and left side-bending radiographs to assist in the selection of spinal levels for fusion. 3. The planned instrumentation pattern (hooks, wires, screws, and rods) is drawn on the coronal radiograph. 4. Two to four units of autologous or directed donor blood should be cross-matched. Intraoperative blood salvage (cell-saver) may also be utilized. 5. Pulmonary function tests if indicated 6. Discussion of indications, goals, perioperative care, and common potential risks with the patient and family 1. Spinal components and techniques are selected pre-operatively. 2. Prone positioning device, such as the Hall-Relton or Wilson frame, which cushions pressure points and permits free expansion of the thorax and abdomen; minimizing abdominal pressure decreases venous pressure, and aids in reducing intraoperative bleeding. 3. Multiple self-retaining retractors such as Weitlaner, Gelpi, and Adson-Beckman retractors 4. Somatosensensory-evoked potential (SSEP) monitoring; motor-evoked potential (MEP) monitoring is also used by some spine surgeons. 5. Headlamp 6. Bone graft substitute and/or bone graft extender products 7. Gelfoam and thrombin 8. The procedure is performed under general anesthesia. 1. Carefully document the preoperative neurologic examination (motor, sensory, and reflexes) so that a comparison can be made in the event that a neurologic deficit is detected during the postoperative period. 2. Prepare and drape the surgical area widely in case surgical extension is required. 3. Scrutinize preoperative radiographs for: a. Anatomic anomalies that may predispose the patient to unexpected neurologic injury (e.g., spina bifida occulta, hemivertebra) b. Sagittal imbalance c. Anatomic relationships that will aid intraoperative decision making (e.g., apex of deformity, relationship of iliac crest to lower vertebral bodies) 4. Intravenous antibiotics should be administered prior to the skin incision and repeated at appropriate intervals. Because of blood loss and fluid shifts, the dosing interval is shorter than in nonoperative situations. 5. Ensure that the anesthesiologist monitors the patient’s coagulation status. Baseline health status, duration of procedure, intraoperative blood loss, and temperature influence coagulation. 6. A separate skin incision to harvest iliac crest bone may be used if the caudal end of the planned fusion ends in the upper lumbar spine. Alternatively, the crest may be approached through the spine incision by subcutaneous dissection and a separate fascial incision directly over the iliac crest. 1. Avoid straying from the subperiosteal plane when exposing the spine. 2. Avoid incorrect placement of instruments in the vicinity of the dura and/or nerve roots. 3. Avoid inserting implants at unintended levels. Do not accept a less than adequate intraoperative scout radiograph when identifying vertebral levels. If necessary, repeat the radiograph. 4. Avoid ending the implanted construct in the apices of secondary coronal or sagittal curves. Chronic instability and late deformity progression may result from partially fusing a curve. 5. Avoid imprecise use of instrumentation implants (e.g., stripping or cross-threading screws/nuts). 1. A suction drain is optional. If a drain is used, a closed suction drain should be placed superficial to the deep fascial closure. 2. Neurologic examination should be performed immediately after termination of general anesthesia and repeated frequently during the postoperative period. If a significant neurologic deficit develops, consider removal of the implanted instrumentation. 3. Consider patient controlled anesthesia (PCA) for postoperative analgesia. Alternatively, epidural anesthesia can be used if adequate pain control can be obtained without motor blockade. 4. Postoperative immobilization is not mandatory. However, some surgeons may elect to use a brace if they are concerned with the quality of the internal fixation. 5. The patient is allowed to sit up and take a few steps with assistance on the day after surgery. 6. The surgical dressing is changed on the second postoperative day. It is discontinued on the fifth postoperative day if there is no wound drainage. This chapter describes basic surgical techniques for performing a selective thoracic fusion for an idiopathic thoracic curve, King-Moe type II or III curve. There are several alternative techniques to those described. Successful techniques have in common the following principles: meticulous subperiosteal dissection, clear understanding of the biomechanics of spinal deformity, precise technical handling of spinal implants, and thorough decortication of posterior elements. Several spinal instrumentation systems are available for selection. Figure 50–1 Patient position. The patient is positioned prone on a positioning device or on longitudinal bolsters. The abdomen and genitalia should not be compressed. Figure 50–2 Skin incision. Plan the skin incision so it is straight in the midline. It should extend from the spinous process proximal to the most cephalad-planned instrumented vertebra to the spinous process of the most caudal-planned instrumented vertebra. A solution of 1:500,000 epinephrine in normal saline is injected into the dermis and subdermal tissues along the planned incision.
Idiopathic Scoliosis
Posterior Spinal Instrumentation and Fusion
Indications
Contraindications
Preoperative Preparation
Special Instruments, Position, and Anesthesia
Tips and Pearls
What To Avoid
Postoperative Care Issues
Operative Technique
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








