Hodgkin Disease
Kenneth L. McClain
EPIDEMIOLOGY
Lymphomas (Hodgkin disease [HD] and non-Hodgkin lymphomas) together make up the third largest group of malignant diseases in children 0 to 19 years of age. The annual incidence of HD per million children is 5.7 for those less than 15 years of age and 34.7 for 15 to 19 year olds. Lymphomas occur more often in white than in black children (1.5:1).
PATHOGENESIS
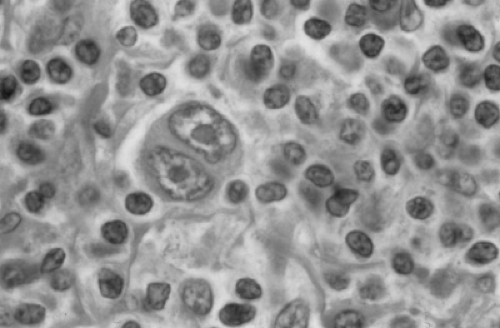
The pathologic Reed-Sternberg cell (Fig. 304.1) in HD is a B lymphocyte as defined by the immunophenotype and molecular studies of Carbone and associates. In HD lesions, the Reed-Sternberg cell is accompanied by varying amounts of fibrosis and lymphocytic infiltration described in the systems of typing for HD. Because more patients are from better socioeconomic conditions, delayed exposure to a common infectious agent, such as Epstein-Barr virus (EBV), may be relevant, as reported by Razzouk and colleagues. Patients with HD have a higher titer against the EBV viral capsid antigen than most children do years after infectious mononucleosis. However, this finding may be secondary to abnormalities of the immune system in HD. Data supporting the contagion theory of HD are controversial. Reported clusters of HD have been discounted on the basis of flawed statistical analysis. Molecular studies have identified EBV RNA and viral proteins in Reed-Sternberg cells. Molecular evidence of EBV DNA in 58% of all HD cases was reported from one institution. Of the nodular sclerosis cases studied, 42% tested positive for EBV, and in the mixed cellularity cases, 65% were positive. Seventy-six percent of cases from children younger than 10 years had positive test results, but only 22% of those from children older than 10 years had EBV in the tumor cells.
CLINICAL MANIFESTATIONS AND DIAGNOSIS
Presenting Signs and Symptoms
Most children present with painless lymphadenopathy in the cervical, supraclavicular, axillary, or inguinal nodes. Splenic or hepatic enlargement is infrequently found in early stages of HD. Fewer than 20% of patients have the systemic (B-symptoms) of fever, night sweats, or weight loss of more than 10%.
A mediastinal mass is seen on chest radiographic films in 17% to 40% of patients and is found more often in children older than 12 years with enlargement of low cervical or supraclavicular nodes. Nearly 30% have mediastinal masses greater than one-third of the chest diameter that may cause dysphagia, dyspnea, cough, or the superior vena cava syndrome.
Differences exist in the histologic type and the stage of disease in children younger than and older than 7 years. Almost 75% of the older group has the nodular sclerosing type of HD, compared with 50% of the younger group. The younger group has more cases of lymphocyte predominance and mixed-cellularity histology. Almost 60% of the younger and 33% of older children have limited-stage disease (i.e., stage I or IIA). Conversely, 38% of the older group and 12% of the younger group have stage IIIB or IV disease.
Staging
A complete evaluation (staging) of patients with suspected HD is mandatory before beginning chemotherapy treatment so radiotherapy (RT) can be appropriately directed to sites of disease. Evaluation and treatment of these diseases should be undertaken at a center that has a team of pediatric oncologists, pathologists, surgeons, radiotherapists, nurses, and social workers experienced in the diagnosis and care of children with cancer. Prompt and efficient care of the child in this setting is the only way to guarantee optimal treatment and the best outcome. This is especially true for the 15- to 19-year-old group of patients. Studies have shown that they are the least likely to be enrolled on clinical trials in which the most up to date therapy is available. Consequently, their overall survival is much lower than that of patients placed in the appropriate Children’s Oncology Group trials.
Routine evaluation of a patient with suspected HD should include a complete history, with emphasis on constitutional symptoms such as fever and weight loss, previous infections, family exposures to toxins, parental occupational hazards, and evidence for underlying immune deficiencies and familial cancer. A complete physical examination means assessment of general health, height and weight, size and location of lymphadenopathy, liver and spleen size, skin infiltrations, pulmonary findings, and neurologic signs. Laboratory evaluation should include a complete blood count, erythrocyte sedimentation rate, renal and liver function tests (including lactate
dehydrogenase levels), urinalysis, anteroposterior and lateral chest radiographic films, and computed tomographic scans of the abdomen and chest with oral and intravenous contrast. Positron emission tomography scans may provide additional sensitivity to identifying pathologic lymph nodes or infiltration of other organs. Because of increased resolution of computed tomographic scans and new treatment regimens, bipedal lymphangiography has largely been abandoned. Gallium-67 (67Ga) scans also can be helpful in defining the disease activity of mediastinal HD. Eighty percent of patients have uptake of 67Ga in their mediastinal masses at the time of diagnosis. After therapy, a patient with a residual mediastinal mass that continues to absorb 67Ga is likely to have active HD. Bone marrow biopsies have long been recommended as part of the routine evaluation of all patients with HD. However, data from our institution suggest that patients with clinical evidence of low-stage (I to IIIA) disease do not need these tests routinely. Of 110 patients, only two had bone marrow trephine biopsies with evidence of HD in them. Both these patients had clinical stage IIIB disease.
dehydrogenase levels), urinalysis, anteroposterior and lateral chest radiographic films, and computed tomographic scans of the abdomen and chest with oral and intravenous contrast. Positron emission tomography scans may provide additional sensitivity to identifying pathologic lymph nodes or infiltration of other organs. Because of increased resolution of computed tomographic scans and new treatment regimens, bipedal lymphangiography has largely been abandoned. Gallium-67 (67Ga) scans also can be helpful in defining the disease activity of mediastinal HD. Eighty percent of patients have uptake of 67Ga in their mediastinal masses at the time of diagnosis. After therapy, a patient with a residual mediastinal mass that continues to absorb 67Ga is likely to have active HD. Bone marrow biopsies have long been recommended as part of the routine evaluation of all patients with HD. However, data from our institution suggest that patients with clinical evidence of low-stage (I to IIIA) disease do not need these tests routinely. Of 110 patients, only two had bone marrow trephine biopsies with evidence of HD in them. Both these patients had clinical stage IIIB disease.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree