I. HIP DISLOCATION. Hip dislocation can be simple (without fracture) or complex (associated with femoral head, femoral neck, and/or acetabular fractures). High-energy trauma such as motor vehicle accident or pedestrian-automobile accident is often the mechanism of injury due to the inherent stability of this ball and socket joint. Advance Trauma Life Support (ATLS) protocols should be followed because of the high association of fractures and other systems injuries (head, thoracic, and abdomen).1 A fracture or fracture–dislocation at the hip can easily be missed when associated with an ipsilateral extremity injury. Such an injury emphasizes the rule: always visualize the joint above and the joint below the diaphyseal fracture. Because injuries about the pelvis can be missed in a seriously traumatized patient, most authorities advocate a routine pelvic roentgenogram for all patients involved in severe blunt trauma. This injury is viewed as an orthopaedic emergency. In general, the sooner the reduction is achieved, the better the end result.2,3 The goals are to minimize the complications (femoral head avascular necrosis [AVN], posttraumatic arthritis, sciatic nerve palsy) that are associated with this injury.4,5
II. CLASSIFICATION OF DISLOCATIONS
A. Anterior dislocations (Thompson and Epstein) (Fig. 23-1)
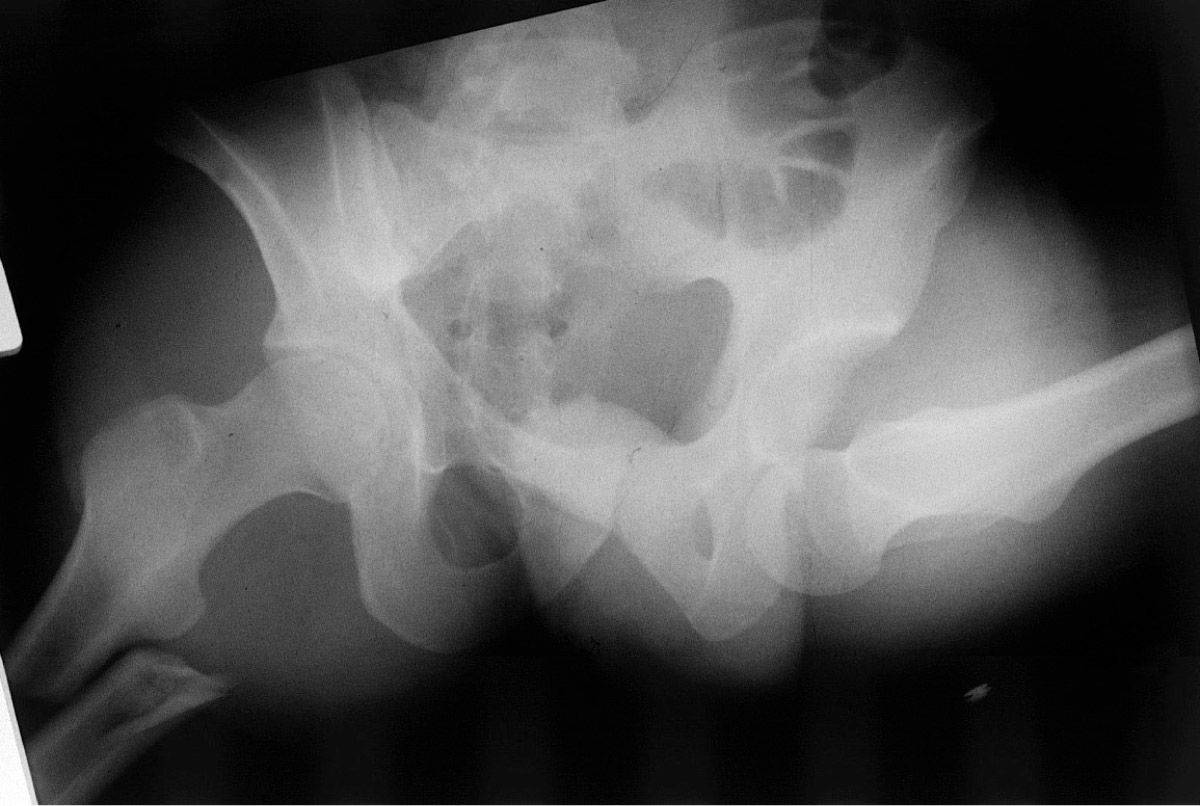
Figure 23-1. An anterior dislocation prior to reduction. (From Bucholz RW, Heckman JD, eds. Rockwood & Green’s Fractures in Adults. 5th ed. Philadelphia, PA: Lippincott, Williams & Wilkins; 2001; 1547-1578, with permission.)
- Obturator
- Iliac
- Pubic
- Associated femoral head fractures (see V)
B. Posterior dislocations (Fig. 23-2)

Figure 23-2. A posterior dislocation prior to reduction.
- Without fracture
- With posterior wall fracture (see IV)
- With femoral head fracture (see V)
III. ANTERIOR DISLOCATIONS
A. This injury usually occurs in an automobile accident, in a severe fall, or from a blow to the back while squatting. The mechanism of injury is forced abduction. The neck of the femur or trochanter impinges on the rim of the acetabulum and levers the femoral head out through a tear in the anterior capsule. If in relative extension, an iliac or pubic dislocation occurs; if the hip is in flexion, an obturator dislocation occurs. In many instances, there is an associated impaction or shear fracture of the superior articular surface of femoral head as the head passes superiorly over the anteroinferior rim of the acetabulum. These injuries are associated with poor long-term results.6,7
B. Examination. The initial key examination should include the following: the ATLS protocol to look for other injuries, visualizing the position or deformity of the leg (anterior or posterior dislocation), documenting the neurologic examination (peroneal nerve deficit is most common) before reduction, and obtaining an AP pelvis radiograph. On examination with an obturator dislocation, the hip is abducted, externally rotated, and flexed, but in the iliac or pubic dislocation, the hip may be extended. The femoral head can usually be palpated near the anterior iliac spine in an iliac dislocation or in the groin in a pubic dislocation. In all patients, one must carefully assess the circulatory and neurologic status of the patient before attempting a reduction. The diagnosis is readily apparent on roentgenogram, which shows the femoral head out of the acetabulum in an inferior and medial position.
C. Treatment. Early closed reduction is the treatment of choice, but open reduction may be necessary.4,5 Reduction is optimally attempted under spinal or general anesthesia, which ensures complete muscle relaxation. In the multiply injured patient, reduction may be attempted in the emergency department with sedation or pharmacologic paralysis. After the airway is controlled, initiate strong but gentle traction along the axis of the femur while an assistant applies stabilization of the pelvis by pressure on the anterior iliac crests. For the obturator dislocation, the traction is continued while the hip is gently flexed, and the reduction is accomplished usually by gentle internal rotation. A final maneuver of adduction completes the reduction, but should not be attempted until the head has cleared the rim of the acetabulum with traction in the flexed position. For the iliac or pubic dislocation, the head should be pulled distal to the acetabulum. The hip is gently flexed and internally rotated. No adduction is necessary. If the hip does not reduce easily, forceful attempts are not indicated. Failure to obtain easy reduction with the above maneuvers usually indicates that traction is increasing the tension on the iliopsoas or closing a rent in the anterior capsule, producing a “buttonhole” effect. Forced maneuvers only increase the damage. Because the closed reduction may fail, the patient is initially prepared for an open procedure. The open reduction can be accomplished through a muscle-splitting incision, using the lower portion of the standard anterior Smith-Peterson approach. The structures preventing the reduction are released. The postreduction treatment is the same as for a posterior dislocation of the hip, except it is important to avoid excessive abduction and external rotation.
D. Prognosis and complications. Excellent reviews of hip dislocations have been published; anterior dislocations occur in approximately 13% of hip dislocations. Early reduction is necessary if a satisfactory result is to be obtained, and although the end result is frequently excellent in the child, traumatic arthrosis and, occasionally, AVN make the prognosis guarded in the adult. Recurrent dislocation is rare in an adult.2,3,6
IV. POSTERIOR DISLOCATIONS
A. The mechanism of injury is usually a force applied against the flexed knee with the hip in flexion, as occurs most commonly when the knee strikes the dashboard of an automobile during a head-on impact. If the hip is in neutral or adduction at the time of impact, a simple dislocation is likely, but if the hip is in slight abduction, an associated fracture of the posterior or posterosuperior acetabulum can result. As the degree of hip flexion increases, it is more probable that a simple dislocation is produced.4,5
B. Physical examination reveals that the leg is shortened, internally rotated, and adducted. A careful physical examination should be carried out before reduction including sensory examination and muscle group motor strength grading. Sciatic nerve injury is associated with 10% to 13% of these injuries.8,9 Associated bony or ligamentous injury to the ipsilateral knee, femoral head, or femoral shaft is not uncommon. When associated with a femoral shaft fracture, a dislocation may go unrecognized because the classic position of flexion, internal rotation, and adduction is not apparent. In this situation, the diagnosis is confirmed by a single anteroposterior roentgenogram of the pelvis as part of the initial trauma roentgenographic series. This single examination does not allow adequate assessment of any associated acetabular fracture.10–12 Therefore, additional roentgenograms are needed for treatment planning before carrying out a reduction if an acetabular fracture is identified. The patient, not the X-ray beam, is moved to obtain the following films: the anteroposterior, obturator oblique, and the iliac oblique views.11,13 This is best accomplished by keeping the patient on a backboard and using foam blocks to support the oblique position of the board (Fig. 23-3). If necessary, computed tomography (CT) scanning can also be performed; optimally, this is done after the closed reduction of the hip joint to reestablish femoral head circulation. Although some authors question its routine use after uneventful closed reduction, others report a 50% incidence of bony fragments being identified with CT.13–15
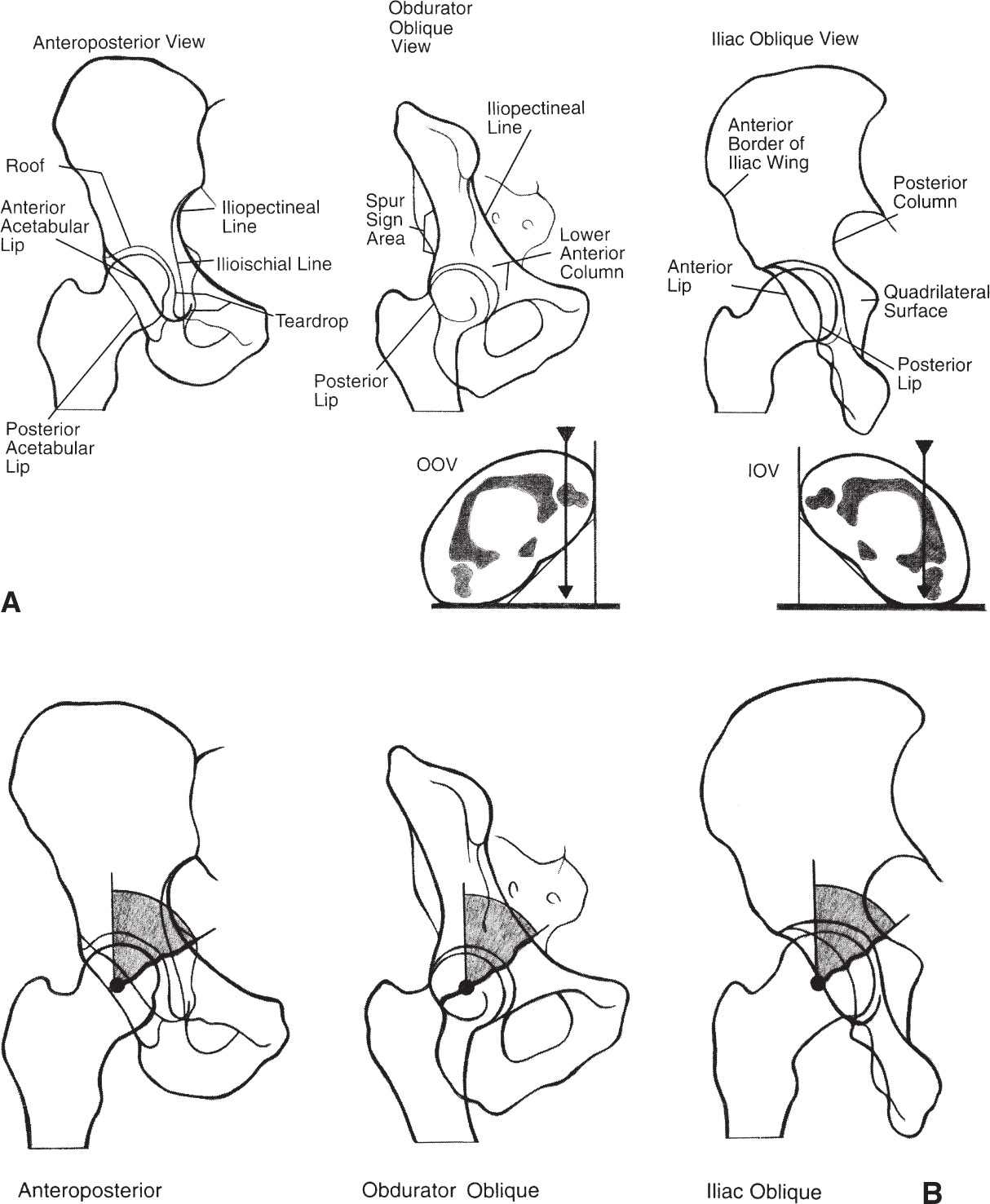
Figure 23-3. Radiographic assessment of acetabular fractures. A: The anteroposterior, obturator oblique, and iliac views are essential for the definition of the fracture. B: The “roof arc” measurement is made between a vertical line and the angle of the fracture. Angles greater than 40° on all three views indicate a fracture which may be treated nonoperatively. (From Hansen ST, Swiontkowski MF. Orthopaedic Trauma Protocols. New York, NY: Raven; 1993:249, with permission.)
C. Treatment
- Posterior dislocation without fracture. This dislocation is reduced as soon as possible and always within 8 to 12 hours when possible. Reduction is accomplished with the Allis maneuver under spinal or general anesthesia to overcome the significant muscle spasm. The essential step in a reduction is traction in the line of the deformity, followed by gentle flexion of the hip to 90° while an assistant stabilizes the pelvis with pressure on the iliac spines. With continued traction, the hip is then gently rotated into internal and external rotation, which usually brings about a prompt restoration of position. Because considerable traction is required, even with good muscle relaxation, the alternative method of Stimson may be attempted. The patient is placed prone with the hip flexed over the end of the table, and an assistant fixes the pelvis by extending the opposite leg. The same traction maneuvers described earlier are completed, but the pull is toward the floor with pressure behind the flexed knee. Although considerable traction is necessary, under no circumstances should rough or sudden manipulative movement be attempted. Postreduction stability should be confirmed on physical examination and by a roentgenogram obtained in the operating room to be sure that there are no fractures around the femoral head or neck.
a. Postreduction treatment. Complete AP pelvis and Judet views should be obtained after reduction to confirm concentric reduction and evaluate for other injuries such as acetabular, femoral head, and neck fractures. CT scan is recommended if a nonconcentric joint is seen on plain films to evaluate for chondral or bony loose bodies. Frick and Sims14 reported that a CT scan is not necessary if the hip joint is concentric on all three pelvic views (AP, Judets). Recently, Mullis and Dahners found loose bodies in seven of nine patients that they performed hip arthroscopy on after traumatic dislocation despite negative imaging studies showing concentric reduction and no loose bodies. However, further studies are needed to determine whether removal of these loose bodies in an already concentric joint makes a difference in long-term outcomes. Beware of possible ipsilateral knee injuries. There is a high incidence of meniscal and ligaments injury to the knee, and MRI are warranted if there is clinical suspicion.16
b. Rehabilitation. Isometric exercises for the hip musculature are instituted as soon as pain subsides sufficiently. Continuous passive motion (CPM) may be useful to maintain joint motion, but is not essential. There is no consensus in the literature as to the length of time the patient should be restricted from weight bearing. The authors favor bed rest until the patient is pain free and has established near-normal abduction and extension muscle power. The patient is then allowed to move around using crutches for protective weight bearing until it is determined that he or she can ambulate without pain or an antalgic limp; this generally takes 3 to 6 weeks. At that time, full weight bearing is permitted.
c. Prognosis and complications
- Sciatic nerve injuries are discussed in IV.2.c and e.
- AVN of the femoral head is the most feared delayed complication from a simple posterior dislocation of the hip. It occurs late, but various authors have noted an average time of 17 to 24 months from injury to the time of diagnosis. Rates of approximately 6% to 27% are reported, and figures show an incidence of 15.5% for early closed reductions, increasing to 48% if reduction is delayed. There are no good results if the reduction was delayed more than 48 hours. In Epstein’s classic study of 426 cases, better results were obtained with open reduction and internal fixation in patients who had associated fractures (see Selected Historical Readings). The overall rate of AVN was 13.4% with a higher rate of 18% in patients with associated fractures. For fracture–dislocations

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








