Hip Arthroscopy: The Basics
Marc Safran
Michael Kalisvaart
Matthew A. Stanich
DEFINITION
The hip is increasingly recognized as a source of pain owing to heightened awareness of pathologies, recent research, enhanced imaging techniques, and greater popularity of hip arthroscopy as a diagnostic and therapeutic tool.
Hip arthroscopy first was performed on a cadaver in the 1930s by Burman, but it was not performed regularly until the 1980s, serving mostly as a tool for diagnosis and simple treatments, such as loose body removal, synovial biopsy, and partial labrectomy.
With improvements in instrumentation, indications for hip arthroscopy have expanded because surgeons now are able to do more in the hip with decreased risk of iatrogenic injury. Furthermore, enhanced imaging techniques have allowed noninvasive diagnosis, and research has led to increased understanding of hip pathologies, furthering interest in this procedure.
Hip arthroscopy can be performed in the central compartment (femoroacetabular joint) and peripheral compartment (along the femoral neck), which also has expanded the indications and success of hip arthroscopy, propagating the popularity of this procedure.
ANATOMY
The hip joint is a multiaxial ball-and-socket type of synovial joint in which the head of the femur (ball) articulates with the acetabulum (socket) of the hip.
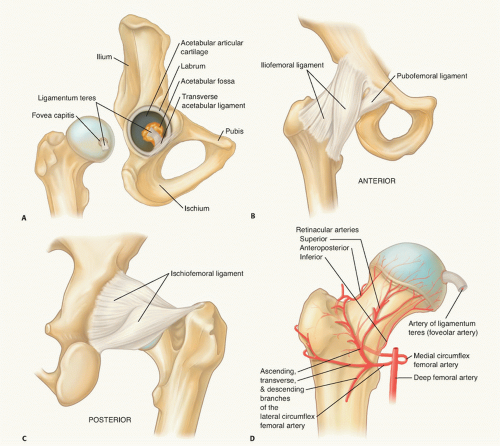
Articular cartilage covers the head of the femur and acetabulum but is not present at the fovea or cotyloid fossa.
The articular cartilage of the femoral head and acetabulum is relatively thin compared with that of the knee (FIG 1A).
The acetabular labrum is a triangular fibrocartilage that attaches to the rim of the acetabulum at the articular cartilage edge, except at the inferior most region of the acetabulum, where the transverse acetabular ligament extends the acetabular rim.
The hip joint is enclosed by a capsule that is formed by an external fibrous layer and internal synovial membrane and attaches directly to the bony acetabular rim.
The fibrous layer consists of the iliofemoral, pubofemoral, and ischiofemoral ligaments, which anchor the head of the femur into the acetabulum (FIG 1B,C).
The ligamentum teres is extracapsular and travels from the central acetabulum to the foveal portion of the femoral head (FIG 1A).
The major arteries supplying the hip joint include the medial and lateral circumflex femoral arteries, which branch to provide the retinacular arteries that supply the head and neck of the femur (FIG 1D).
The artery to the head of the femur also supplies blood and transverses the ligament of the head of the femur (ie, the ligamentum teres).
The labrum has a relatively low healing potential because vessels penetrate only the outermost layer of the capsular surface.
Pertinent extra-articular neurovascular structures near the hip joint include the lateral femoral cutaneous nerve, femoral nerve, superior gluteal nerve, sciatic nerve, and the ascending branch of the lateral circumflex femoral artery.
The lateral femoral cutaneous nerve, formed from the posterior divisions of L2 and L3 nerve roots, supplies the skin sensation of the lateral thigh. It travels from the pelvis just distal and medial to the anterior superior iliac spine (ASIS) and divides into more than three branches distal to the ASIS.
The femoral nerve and artery run together with the femoral vein. They pass under the inguinal ligament midway between the ASIS and the pubic symphysis, with the nerve being most lateral and the vein most medial but being mostly superficial at the level of the hip.
The femoral nerve is 3.2 cm from the anterior hip portal but slightly closer at the level of the capsule.
The superior gluteal nerve, formed from the posterior divisions of L4, L5, and S1, passes posterior and lateral to the obturator internus and piriformis muscles, then between the gluteus medius and minimus muscles approximately 4 cm proximal to the hip joint.
The sciatic nerve, formed when nerves from L4 to S3 come together, passes anterior and inferior to the piriformis and posterior to the deep hip external rotators to supply the hamstrings and lower leg, foot, and ankle.
The sciatic nerve is 2.9 cm from the posterior hip arthroscopy portal but is closest at the level of the capsule.
Internally rotating or flexing the hip prior to making the posterior portal brings the nerve dangerously close to the arthroscope.
The lateral femoral circumflex artery is a branch of the femoral artery that, along with the medial circumflex artery, forms a vascular ring about the neck of the femur, providing arteriole branches to supply the femoral head (FIG 1D).
The lateral femoral circumflex artery is 3.7 cm inferior to the anterior arthroscopy portal; it is much closer at the level of the capsular entry of the arthroscope.
PATHOGENESIS
Loose bodies can be ossified or nonossified and can either appear after traumatic hip injury or be associated with conditions such as osteochondritis dissecans and synovial chondromatosis.8
Labral tear often results from hyperextension or external rotation of the hip and is more likely with hip dysplasia.
Chondral (articular cartilage) damage can result from dislocation or subluxation of the hip or direct impact onto the hip and is associated with labral tears in more than half the cases.9
Femoroacetabular impingement is a major cause of labral tears and chondral damage.
It usually occurs when there is loss of femoral head-neck offset (cam impingement), excessive acetabular coverage (eg, osteophytes, retroversion, overcorrection with pelvic osteotomy, protrusio acetabuli, or otto pelvis) (pincer impingement), or both.
The femoral head-neck junction abuts the acetabulum and labrum, resulting in tearing of the labrum, delamination of the articular cartilage, synovitis, and, eventually, arthritis.
Ligamentum teres pathology may be due to ligament hypertrophy or partial or complete tearing and may be the result of trauma or degenerative joint disease (DJD).
Ligamentum hypertrophy or tearing may result in pain as a result of catching of a thickened or torn edge between the joint surfaces.
DJD may be associated with loose bodies, labrum tears, chondral damage, ligamentum teres pathology, and synovitis.
Avascular necrosis of the femoral head is primarily idiopathic but can be associated with corticosteroid use, alcohol consumption, fracture, and deep sea diving (caisson disease), among others.
Synovial diseases such as pigmented villonodular synovitis, synovial chondromatosis, inflammatory arthritis, and osteochondromatosis can be sources of hip pain and joint damage.
Hip instability, either traumatic or atraumatic, may be a cause of labral tears and chondral damage.
Hip instability may be traumatic (eg, acetabular posterior wall fractures) or atraumatic (eg, developmental dysplasia of the hip, connective tissue disorders, benign hypermobility) or as a result of microtrauma (repetitive external rotation).
Pathology exists as a spectrum from hip dislocation to subluxation to microinstability.
NATURAL HISTORY
The natural history of most pathologies about the hip has not been studied; much of the purported natural history is therefore conjecture.
Removal of loose bodies alleviates mechanical symptoms and reduces articular cartilage damage.
Labral tears and chondral lesions that are débrided may result in degenerative arthritis.
Untreated femoroacetabular impingement may result in degenerative arthritis.
It has been proposed, but not proved, that labral repair or surgery for femoroacetabular impingement may lower the risk of developing DJD or slow the rate of degeneration.
PATIENT HISTORY AND PHYSICAL FINDINGS
The patient history should include an investigation of the quality and location of pain, timing and precipitating cause of symptoms, and any referred pain.
Patients with intra-articular pathology may have difficulty with torsional or twisting activities, discomfort with prolonged hip flexion (eg, sitting), pain or catching from flexion to extension (eg, rising from a seated position), and greater difficulty on inclines than on level surfaces.2
Intra-articular pathology may be associated with groin pain extending to the knee and mechanical symptoms such as popping, locking, or restricted range of motion (ROM).3
The source of intra-articular pathology should be investigated in patients with continuous hip pain for longer than 4 weeks.
Physical examination methods are summarized later.
It is important to follow a systemic approach to examination that includes inspection, palpation, ROM, strength, and special tests.11
Intra-articular pathologies do not have palpable areas of tenderness, although compensation for long-standing intraarticular problems may result in tenderness of muscles or bursae.
Motor strength and neurovascular examinations must be performed for the entire lower extremity.
It is important to rule out other causes of pain referred to the hip.
Spinal pain usually is localized at the posterior buttock and sacroiliac region and may radiate to the lower extremity.
Injuries to the sacrum and sacroiliac joint are recognized by a positive gapping or transverse anterior stress test.
Abdominal injuries are recognized by basic inspection and palpation of the abdomen for a mass or fascial hernia, which can be evaluated by isometric contraction of the rectus abdominis and obliques.
Abdominal muscle injury is recognized by pain during contraction of the rectus abdominis and obliques.
Herniography may be used to rule out hernias.
Particularly difficult to diagnose is the sports hernia (Gilmore groin), which is not a true hernia.
Genitourinary tract
Injuries to the pelvic area, such as pubic symphysis and intrapelvic problems, are recognized by the gapping/transverse anterior stress test.
Specific tests for the hip include the following:
McCarthy test: distinction of internal hip pathology such as torn acetabular labrum or lateral rim impingement
Stinchfield and Fulcrum test: diagnosis of internal derangements, primarily of the anterior portion of the acetabulum
Scour test: associated with microinstability or combined anterior anteversion, acetabular anteversion summation, hyperlaxity, or strain of the iliofemoral ligament
Thomas test: tests for flexion contracture. Extension to 0 degrees (in line with the body) without low back motion is normal. Less than full extension without rotating the pelvis or lifting the lower back is consistent with a flexion contracture.
Ober test: used to evaluate iliotibial band tightness. The test is positive when the upper knee remains in the abducted position after the hip is passively extended and abducted, then adducted, with the knee flexed. If, when the hip and knee are allowed to adduct while the hip is held in neutral rotation, the knee adducts past midline, the hip abductors are not tight; whereas if the knee does not reach to midline, then the hip abductors are tight.
Ely test: if on flexion of the knee the ipsilateral hip also flexes, then the rectus femoris is tight.
Trendelenburg test: indicative of hip abductor weakness and may indicate labrum pathology that affects neuroproprioceptive function. If the pelvis (iliac crest or posterior superior iliac spine) of the ipsilateral hip of the leg that is lifted elevates from the neutral standing position, this is normal. If the pelvis drops below the contralateral pelvis or from the starting position (ie, iliac crest/posterior superior iliac spine), this is considered a positive Trendelenburg sign and indicative of hip abductor weakness of the muscles on the extremity standing on the ground. If the pelvis stays level, then this is indicative of mild weakness and recorded as level.
Patrick test (FABER test): indicative of sacroiliac abnormalities or iliopsoas spasm. Pain may be felt with downward stress on the flexed knee. Pain in the posterior pelvis may be considered a positive finding that indicates the pain is coming from the sacroiliac joint.
Labral stress test: indicative of labral tear. The patient will note groin pain or a click in a consistent position as the hip is being rotated.
Piriformis test: Pain in the lateral hip or buttock reproduced by this maneuver is consistent with pain from the piriformis.
Impingement test: Pain in the groin is a positive test and is consistent with intra-articular hip pain, not just femoroacetabular impingement.
Hip extension and external rotation test: indicative of hip microinstability. The patient will note discomfort or apprehension in the anterior aspect of the hip.
IMAGING AND OTHER DIAGNOSTIC STUDIES
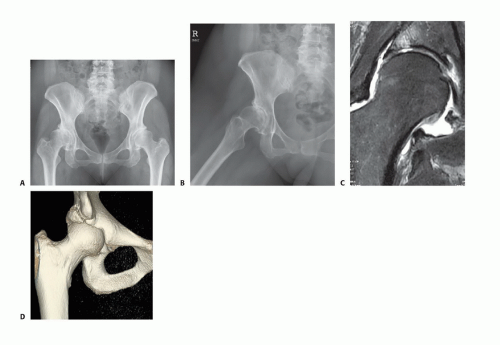
Routine anteroposterior (AP) and lateral (usually cross-table lateral or Dunn view) radiographs should be obtained in all patients with hip pain to evaluate variations in bony architecture and visualization of areas that may present with hip pain such as the pubic symphysis, sacrum, sacroiliac joints, ilium, and ischium.
Radiographs help exclude degenerative joint changes, osteonecrosis, loose bodies, stress fractures, or other osseous pathology, and help assess for acetabular dysplasia and femoral neck abnormalities (bump or cam lesion) and femoroacetabular impingement (FIG 2A,B).
Bone scan or radionuclide imaging is sensitive in detecting fractures, arthritis, neoplasm, infections, and vascular abnormalities but has low specificity and poor anatomic resolution.
Magnetic resonance imaging (MRI) is used to detect stress fractures of the femoral neck and to identify sources of hip pain such as osteonecrosis, pigmented villonodular synovitis, synovial chondromatosis, osteochondromas, and other intra-articular pathology.
MRI arthrography can increase the ability to diagnose and describe labral pathology and articular cartilage loss (FIG 2C).
MRI combined with the use of intra-articular local anesthetic with gadolinium is used to assess pain relief and provide evidence that intra-articular pathology may be causing pain.
Recent studies have demonstrated a very high prevalence of asymptomatic labral tears in young, active people.
Computed tomography (CT), MRI, and occasionally radioisotope imaging typically are required to help diagnose labral tears, hip instability, iliopsoas tendinitis, inflammatory arthritis, early avascular necrosis, occult fractures, psoas abscess, tumor, upper lumbar radiculopathy, or vascular abnormalities.
CT scan can be useful to measure ante- and retroversion of the femoral neck and acetabulum, to show the size and shape of the acetabulum and femoral head and neck, to elucidate bony architecture, to confirm concentric reduction after hip dislocation, and to rule out loose bodies.
CT scan has also been shown to be helpful in assessing the morphology of the AIIS (anterior inferior iliac spine), which has been implicated in subspinous impingement.
Ultrasound is a nonirradiating way of evaluating intraarticular effusions and soft tissue swelling.
Iliopsoas bursography is the choice imaging modality to detect iliopsoas bursitis and internal snapping hip.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree