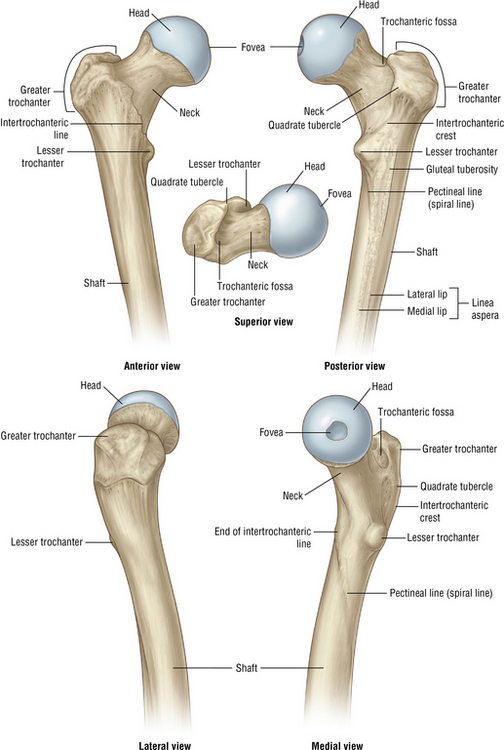
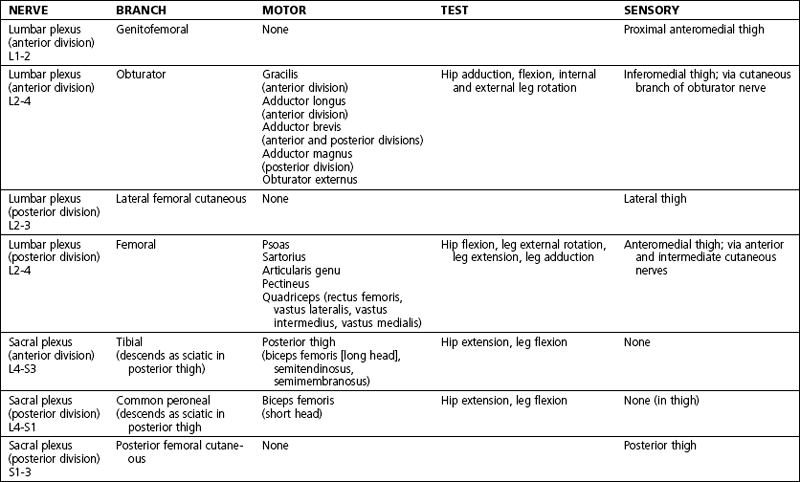
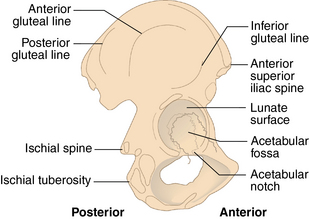
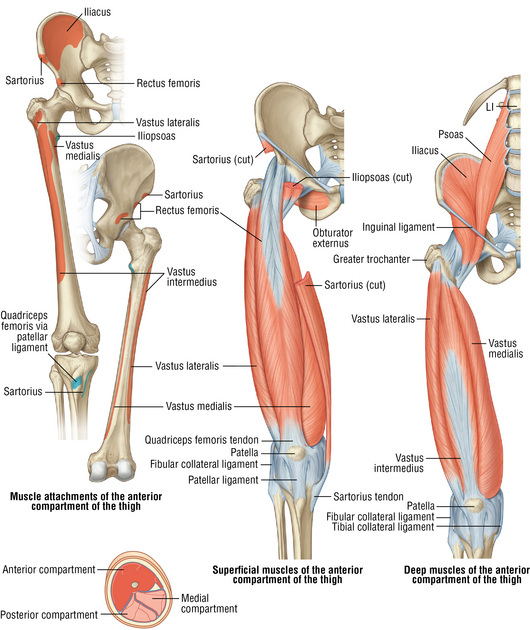
6 Hip and femur Bones: Figures 6-1 and 6-2 Figure 6-1. External surface of the hip bones. (From Bogart BI, Ort VH: Elsevier’s integrated anatomy and embryology, Philadelphia, 2007, Mosby.) Figure 6-4. Anterior compartment muscles of the thigh. (Elsevier illustration from www. elsevierimages.com. Copyright, Elsevier Inc. All rights reserved.) Table 6-2. Normal Range of Motion of the Hip Table 6-4. Differential Diagnosis of Hip and Thigh Pain Eustice C: Osteoarthritis (website). http://osteoarthritis.about.com/od/osteoarthritisdiagnosis/a/range_of_motion.htm. Accessed September 11, 2012. Greene WB: Netter’s orthopaedics, Philadelphia, 2006, Saunders. Hansen JT: Netter’s clinical anatomy, ed 2, Philadelphia, 2010, Saunders. • Femoral acetabular impingement (FAI) • Congenital dysplasia (∼80% female) • Trauma (three times more likely to develop) • Slipped capital femoral epiphysis (SCFE) • Avascular necrosis (AVN) (likely from alcohol or systemic steroid use) • Inflammatory disorders (rheumatoid arthritis, juvenile rheumatoid arthritis, ankylosing spondylitis) • Sepsis (complaint of sharp pain in the groin or anterior hip, worse with weight bearing; night pain in in patients with severe OA) Estimated postoperative course: • Sutures are removed, and a wound check is performed. • PT is begun for hip ROM, strengthening, balance, and gait training. The patient is weight bearing as tolerated. • The patient returns to the clinic for radiographs of the pelvis and the lateral hip. Check for ROM, as well as abductor and quadriceps strength. • Continue to wean the patient off assistive devices (walker, cane) with progressive PT. • The patient may drive, if he or she is not taking narcotics. Stop anticoagulation.
Anatomy
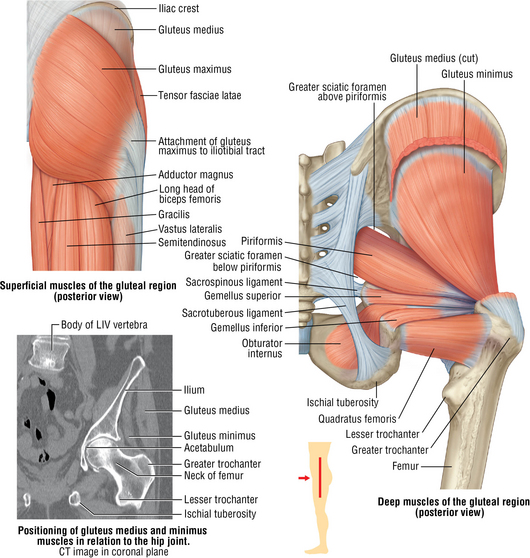
Muscles and tendons: Figures 6-4 and 6-5
Physical examination
Normal range of motion (ROM): Table 6-2
Extension
115 degrees
Flexion
125 degrees
External rotation
45 degrees
Internal rotation
45 degrees
Abduction
45 degrees
Adduction
45 degrees
Special tests
 FABERE test: This maneuver tests for hip osteoarthritis (OA). The patient lies supine while the examiner flexes hip and knee and places the lateral malleolus across the contralateral knee. The examiner then extends the hip by pushing the flexed knee toward the table. A positive test result is when this maneuver elicits severe pain or restriction. The name of this test is an acronym for flexion abduction external rotation and extension.
FABERE test: This maneuver tests for hip osteoarthritis (OA). The patient lies supine while the examiner flexes hip and knee and places the lateral malleolus across the contralateral knee. The examiner then extends the hip by pushing the flexed knee toward the table. A positive test result is when this maneuver elicits severe pain or restriction. The name of this test is an acronym for flexion abduction external rotation and extension.
Differential diagnosis: Table 6-4
Buttock pain
Ischial bursitis
Sciatica
Hamstring strain
Piriformis syndrome
Gluteal tear
Sacroiliac dysfunction
Groin pain
Hip arthritis
Avascular necrosis
Femoral acetabular impingement
Adductor strain
Femoral neck fracture
Sacroiliac dysfunction
Osteitis pubis
Lateral hip pain
Trochanteric bursitis
Posterior thigh pain
Sciatica
Anterior thigh pain
Iliopsoas tendinitis/bursitis
Hip arthritis
Hamstring strain
Femoral shaft fracture
Suggested readings
Hip osteoarthritis
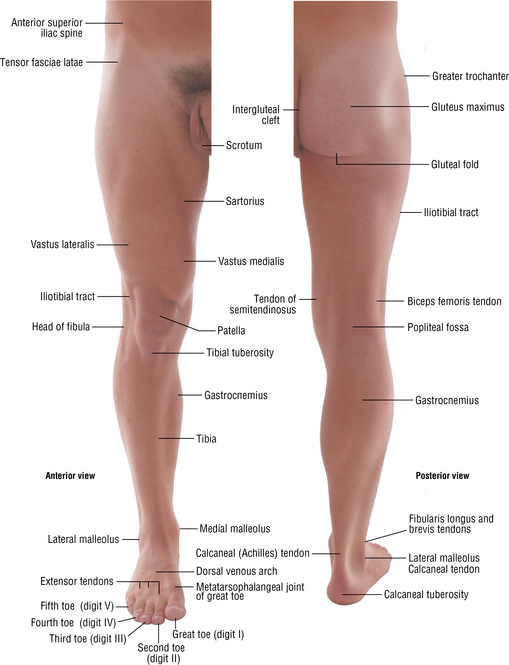
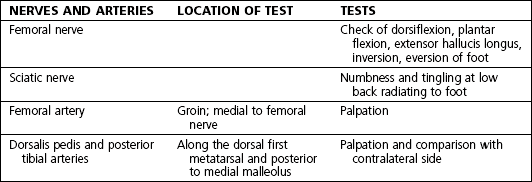
Physical examination
 Antalgic gait; posture and use of assistive devices
Antalgic gait; posture and use of assistive devices
 Positive Trendelenburg test result: difficulty standing on one leg on the affected side because of abductor weakness
Positive Trendelenburg test result: difficulty standing on one leg on the affected side because of abductor weakness
 Pain with active and passive ROM especially with hip flexion and internal rotation
Pain with active and passive ROM especially with hip flexion and internal rotation
 Check of distal pulses (dorsalis pedis and posterior tibial)
Check of distal pulses (dorsalis pedis and posterior tibial)
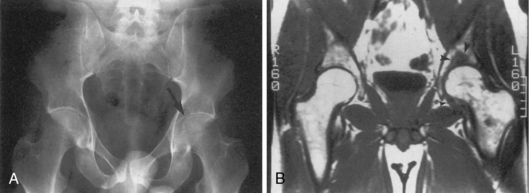
Imaging: Figure 6-9
 Order radiographs: pelvis and OR lateral of hip. OR lateral requires the patient to rotate the hip internally approximately 10 to 15 degrees to provide a true lateral view because of the natural anteversion of the femoral head in the acetabular cup. Consider a frog leg view to assess for FAI.
Order radiographs: pelvis and OR lateral of hip. OR lateral requires the patient to rotate the hip internally approximately 10 to 15 degrees to provide a true lateral view because of the natural anteversion of the femoral head in the acetabular cup. Consider a frog leg view to assess for FAI.
 FAI: Order magnetic resonance imaging (MRI) without contrast to assess for soft tissue and labral damage. If labral damage is present, the patient will need total hip arthroplasty (THA); if not, consider surgical débridement of the femoral head.
FAI: Order magnetic resonance imaging (MRI) without contrast to assess for soft tissue and labral damage. If labral damage is present, the patient will need total hip arthroplasty (THA); if not, consider surgical débridement of the femoral head.
 AVN: Order MRI with and without contrast to assess the extent of necrosis. If the femoral head has collapsed, the patient will need THA; if not, consider core decompression and bone graft to restore the blood supply.
AVN: Order MRI with and without contrast to assess the extent of necrosis. If the femoral head has collapsed, the patient will need THA; if not, consider core decompression and bone graft to restore the blood supply.
 Order a computed tomography (CT) scan for complex cases to assess the acetabular cup.
Order a computed tomography (CT) scan for complex cases to assess the acetabular cup.
Treatment options
Operative management
Informed consent and counseling
 Risks include bleeding, infection, blood clots, and LLD.
Risks include bleeding, infection, blood clots, and LLD.
 The patient will need medical clearance.
The patient will need medical clearance.
 The average hospital stay lasts 3 days.
The average hospital stay lasts 3 days.
 Patients require 2 to 6 weeks of anticoagulation treatment.
Patients require 2 to 6 weeks of anticoagulation treatment.
 Expect 6 weeks of healing, PT, and strict hip precautions to prevent dislocation (no flexion >90 degrees or adduction) if the posterolateral approach is used; if the anterolateral approach is chosen, no hip precautions are necessary.
Expect 6 weeks of healing, PT, and strict hip precautions to prevent dislocation (no flexion >90 degrees or adduction) if the posterolateral approach is used; if the anterolateral approach is chosen, no hip precautions are necessary.
 Expect to wait about 3 months before returning to work. Work restrictions include no prolonged sitting or standing and a 40-lb lifting limit.
Expect to wait about 3 months before returning to work. Work restrictions include no prolonged sitting or standing and a 40-lb lifting limit.
Surgical procedures
 Hardware consists of an acetabular cup, femoral head, femoral stem, polyethylene liner, and acetabular screws. Femoral and acetabular components may be made of titanium, stainless steel, or cobalt chrome (metal-on-polyethylene THA). Ceramic-on-ceramic components may also be used.
Hardware consists of an acetabular cup, femoral head, femoral stem, polyethylene liner, and acetabular screws. Femoral and acetabular components may be made of titanium, stainless steel, or cobalt chrome (metal-on-polyethylene THA). Ceramic-on-ceramic components may also be used.
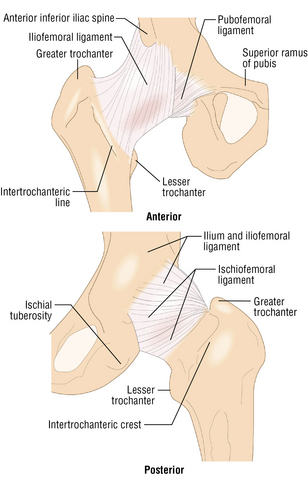
 Posterolateral approach: An 8- to 10-cm incision is made along the posterior border of the greater trochanter to the vastus tubercle. Deep dissection is performed using a Cobb elevator through the gluteus maximus over the posterior border of the greater trochanter, and thus the posterior capsule is entered.
Posterolateral approach: An 8- to 10-cm incision is made along the posterior border of the greater trochanter to the vastus tubercle. Deep dissection is performed using a Cobb elevator through the gluteus maximus over the posterior border of the greater trochanter, and thus the posterior capsule is entered.
 The hip is then dislocated, and the femoral neck is exposed and débrided. A transverse cut is made at the preoperative templated level on the femoral neck with an oscillating saw, and the femoral head is removed. The femur is then reamed, and trial components are placed.
The hip is then dislocated, and the femoral neck is exposed and débrided. A transverse cut is made at the preoperative templated level on the femoral neck with an oscillating saw, and the femoral head is removed. The femur is then reamed, and trial components are placed.
 The acetabulum is then exposed using long Hohmann retractors. The acetabular cup is reamed to create appropriate anteversion (ideally approximately 40 degrees, but no more than 45 degrees) while preserving appropriate bone coverage to ensure that the hip does not impinge, which may increase risk of dislocation. Osteophytes are removed using a rongeur, and soft tissue is débrided. Trial components are placed in the acetabulum.
The acetabulum is then exposed using long Hohmann retractors. The acetabular cup is reamed to create appropriate anteversion (ideally approximately 40 degrees, but no more than 45 degrees) while preserving appropriate bone coverage to ensure that the hip does not impinge, which may increase risk of dislocation. Osteophytes are removed using a rongeur, and soft tissue is débrided. Trial components are placed in the acetabulum.
 The hip is then reduced with trial components and checked to ensure that there is no impingement, LLD, or dislocation at the extremes of flexion or extension.
The hip is then reduced with trial components and checked to ensure that there is no impingement, LLD, or dislocation at the extremes of flexion or extension.
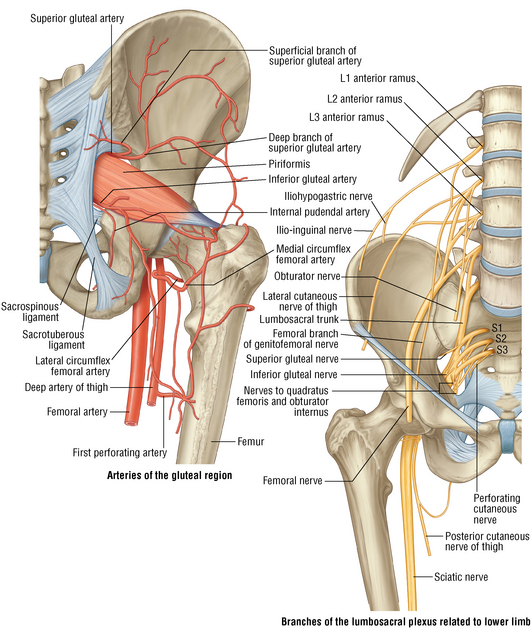
 When trials are satisfactory, the actual components are placed. The capsule is then closed by using Tycron suture to secure the piriformis to the capsule, while avoiding injury to the sciatic nerve that runs directly posterolateral to the piriformis. A drain is placed in deep layer, and local anesthetic is injected. Deep layers are closed with Vicryl suture, and either nylon horizontal mattress or Monocryl subcutaneous sutures close the superficial layers. Use petrolatum gauze (Xeroform) and 4 × 4 gauze pads or Steri-Strips for a bandage, and affix a hip abduction pillow before extubation.
When trials are satisfactory, the actual components are placed. The capsule is then closed by using Tycron suture to secure the piriformis to the capsule, while avoiding injury to the sciatic nerve that runs directly posterolateral to the piriformis. A drain is placed in deep layer, and local anesthetic is injected. Deep layers are closed with Vicryl suture, and either nylon horizontal mattress or Monocryl subcutaneous sutures close the superficial layers. Use petrolatum gauze (Xeroform) and 4 × 4 gauze pads or Steri-Strips for a bandage, and affix a hip abduction pillow before extubation.
 Postoperative 3 months, 6 months, and 1 year
Postoperative 3 months, 6 months, and 1 year
Muscle strains and injuries (adductors, hamstring, quadriceps)
Treatment options
Hip and femur