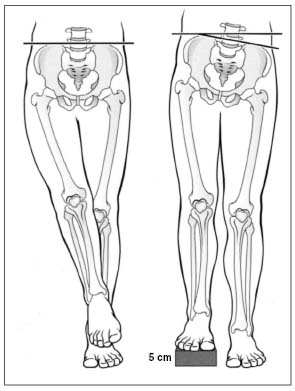
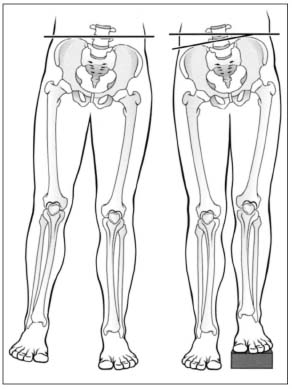
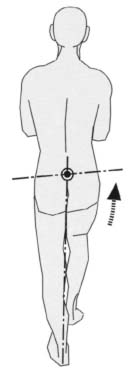
4 Hip In contrast to the other majorjoints of the body, particularly the shoulder and knee, hip disorders are mostly the result of degenerative or inflammatory changes. Isolated injuries to the capsule and ligaments are only rarely encountered and will occur in combination with fractures of the femoral neck or acetabulum as the result of high-energy trauma. Congenital disorders of the acetabulum and femoral epiphysis represent a further large group of hip disorders. Obtaining the patient’s history is the first step of the examination. This will provide significant insight into the nature of disorder. It is particularly important to enquire about the type, location, and time of occurrence of complaints. The clinical examination consists of measuring leg length (see p. 144), observing gait, measuring the circumference of the muscles at standardized measuring points, and assessing the active and’ passive ranges of motion. Functional tests provide further information in certain lines of inquiry. In newborns and infants, provocative tests (Ortolani and Barlow) can be also performed in the presence of suspected hip instability. The dynamic ultrasound examination complements these tests. The patient’s history can provide valuable information about the presence and causes of a hip disorder. The patient’s age is the first clue that the history provides. In newborns and infants, the disorders encountered are most often due to abnormal development such as developmental hip dysplasia. Risk factors for developmental hip dysplasia in newborns may include: – Positive family history – First pregnancy – Breech presentation – Female sex – Other anomalies such as club feet or torticollis – Subsidence of spontaneous kicking toward the end of pregnancy Children and adolescents with a disturbed gait may have Legg-Calvé-Perthes disease or a slipped capital femoral epiphysis. Symptoms of degenerative diseases such as idiopathic chondrolysis or degenerative joint disease are more prevalent in adults and older patients. Questions to ask the patient include: • Location of pain • Onset of pain • Time and duration of pain The differential diagnosis should consider neurogenic claudication (in the presence of stenosis of the spinal canal) and vascular claudication (in the presence of peripheral vascular disease). With neurogenic claudication, the patient feels no pain when beginning exercise, and bending forward in a sitting position lessens the pain. Generally, the pain radiates symmetrically into both the front and back of the thigh. With vascular claudication, the patient reports more rapid onset with exercise, and distal rather than proximal pain. This will be accompanied by alterations in perfusion, and occasionally by murmurs detectable by auscultation over the femoral arteries. Fig. 4.1 Adduction contracture • Pain intensity The patient is observed standing. The following items can provide important information about the cause of the disorder: – Orientation of the pelvis (pelvic obliquity, flexion contracture of the hip) – Deviation of the axis of the legs (genu valgum, genu varum) – Rotation of the legs – Foot deformities – In women, the shape of the Michaelis rhomboid (visible rhomboid-shaped depression over the sacral area) – Structure of the spinal column (scoliosis, tilt) – Muscle contour (asymmetry) – Leg length – Muscle atrophy – Swelling or erythema Fig. 4.2 Abduction contracture Leg length is best evaluated indirectly by observing the position of the pelvis. Sit behind the standing patient so that the patient’s iliac crests are at about the level of your eyes. The patient’s knees are fully extended. While palpating the iliac crests, place shims under the shortened extremity until the pelvis is level. Leg-length differences can be measured quite accurately using this method. This method can produce inaccurate information if: – In the presence of acetabular dysplasia, corresponding deformities of the iliac wing also occur. The pelvis obliquity palpated in such a situation can be misinterpreted as a difference in leg length. – Pelvic obliquity is the result of functional leg shortening due to contracture of the adductors or abductors in the hip (Figs. 4.1 and 4.2). In an adduction contracture of the hip, the affected leg will appear shorter because the patient must raise the pelvis on the affected side when trying to place the foot of the affected side beside that of the nonaffected side. Conversely, an abduction contracture requires the patient to raise the contralateral side to place both feet together parallel to each other. Radiographic techniques are available for more exact measurements and should be considered for more precise measurement. Radiographs with a ruler (the “Scanogram”) or using the CT Scanner with a few cuts at the hips, knees, and ankles yields the most accurate information. After observing the patient standing, inspect his or her gait. Gait irregularities may be due to: – Pain – Muscular weakness (Trendelenburg sign) – Leg shortening (compensatory limp) – Arthrodesis of the hip (compensation for a fused joint) Antalgic gait (Duchenne). The patient attempts to reduce stress on the painful hip with an antalgic gait. There are essentially two mechanisms for achieving this: When the affected leg is in the stance phase, the patient shifts the upper body, and thus the body’s center of gravity, over the affected joint. This shortens the lever arm, with which the body weight acts on the hip, and reduces the tension in the gluteal musculature, relieving the stress on the joint as a whole. The second mechanism is for reducing the duration of stress on the joint, i.e., the stance phase. This leads to a typically truncated gait. Trendelenburg gait due to weakness. In the Trendelenburg gait (Fig. 4.3), weakness of the hip abductors, primarily the gluteal musculature, causes the pelvis to dip toward the unaffected side in the stance phase. Again, the patient attempts to relieve the weakened gluteal musculature by shifting the upper body over the affected side. However, the stance phase is not as sharply truncated as in an antalgic gait, and motion is more uniform. A bilateral Trendelenburg gait produces typical waddling. Testing for the Trendelenburg sign will determine whether such a gait is a true Trendelenburg gait. Compensatory limp with leg shortening. The upper body is shifted slightly over the leg in the stance phase. Otherwise, the gait is relatively smooth. Compensation for hip fusion. Arthrodesis of the hip does not produce a true limp in the sense that the pelvis dips in the stance phase. Rather the increased tilt of the pelvis in the sagittal plane, as it moves from hyperlordosis into lumbar kyphosis, produces femoral anteversion in the swing phase. Since most hip fusions result in some degree of femoral shortening, the post hip fusion gait may demonstrate upper body shift to the affected side in the stance phase as well as femoral anteversion in the swing phase. Fig. 4.3 Trendelenburg limp A number of computerized methods have been developed to supplement clinical examination of gait. These methods, some of which are used in combination with electromyographic studies, may allow the examiner to define the anatomical and functional cause of gait irregularities with far greater precision. To palpate the hip, first locate the origins and insertions of the hip muscles to evaluate tendon disorders involving the muscular insertions (Table 4.1). Muscle pulls in the iliopsoas often occur in athletes (Fig. 4.4). It is almost impossible to palpate the joint capsule in adults. Ultrasound studies should be performed if an effusion is suspected. Further palpation should attempt to exclude disorders such as inguinal and femoral hernias, varicoceles, and lymph node disorders. Palpate the femoral arteries and listen to them through a stethoscope to exclude arterial peripheral vascular disease. In the initial position, the patient is supine with the hip fully extended. The medial aspects of both knees are barely touching, and both feet are parallel. The legs are correctly positioned when the axes of support (the straight lines connecting the midpoints of the hip, knee, and ankle) are parallel. The pelvis is horizontal when the straight line connecting the anterior superior and anterior inferior iliac spine is at an angle of approximately 12° from horizontal. In the neutral position, the pelvis is tilted slightly anteriorly by the lumbar lordosis.
4.1 Introduction
4.2 Clinical Examination
Standard Examination
Patient History
Pain is usually felt in the groin or in a retrotrochanteric location, occasionally radiating to the inner thigh and extending as far as the knee. This means, especially in children, that a hip disorder can masquerade as knee pain. The differential diagnosis should consider pathology in the adductor insertions and involvement of the lumbar spine, particularly the sacroiliacjoints.
Acute pain is indicative of inflammation, infection, or involvement of the femoral head as in an acute slipped capital femoral epiphysis, a subchondral collapse in Legg-Calvé-Perthes disease, or pathologic fractures. Pain that develops slowly suggests a degenerative disorder or tumor.
Transient morning pain that subsides after the patient has taken a few steps, but which reappears with exercise such as walking longer distances or climbing stairs (exercise pain), is typical of degenerative hip disorders.
To help determine the appropriate therapeutic measures, the physician should ask the patient about the intensity of the pain and the resulting impairment of patient well-being. A number of scoring systems have been developed for assessing this impairment (Harris, Hospital for Special Surgery, and Iowa).
Observation
Observation with the Patient Standing
Gait Analysis
Palpation
Assessing the Range of Motion in Adults
| • Iliac spines and sacrum | Origin ofthegluteal musculature and the erector spinae |
| • Anterior superior iliac spine | Origin of the sartorius |
| • Anterior inferior iliac spine | Origin of the rectus femoris |
| • Branches of the pubic bone | Origin of the gracilis and abductors |
| • Ischial tuberosity | Origin of the hamstrings |
| • Lessertrochanter | Insertion of the iliopsoas |
| • Greater trochanter | Insertion of the gluteal musculature |
| • Pes anserinus | Insertion of the sartorius, gracilis, and semitendinosus |
| • Fibularhead | Insertion of the biceps femoris |
| • Lateral tibial epicondyle | Insertion of the iliotibial tract |
Flexion and Extension
Perform the examination with the patient supine on a stable surface. Ensure that the pelvis is in a neutral position by placing your hand under the sacrum. Now flex the contralateral leg at the hip until the lumbar lordosis is neutralized and the sacrum touches your hand. In this position, the patient holds his or her own leg (Thomas grip; Fig. 4.5). Now flex the leg to be examined until the pelvis begins to move. Immobilize the pelvis with your hand on the sacrum. The angle between the thigh and the examining table corresponds to the angle of flexion. Evaluate extension with the patient supine by flexing the contralateral leg past the position in the Thomas grip until the leg being examined is lifted off the table (Fig. 4.6).
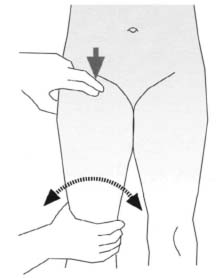
Fig. 4.4 Palpating the lesser trochanter at the insertion of the iliopsoas while rotating the leg.
The difference in the angle between both femurs corresponds to extension.
Hip flexion and extension can also be evaluated in the lateral position. Place the patient on the contralateral side while immobilizing the pelvis in the neutral position of 12° anterior tilt with one hand. To evaluate flexion, flex the leg until the pelvis begins to move. To evaluate extension, place the patient supine, immobilize the contralateral leg with the Thomas grip, and extend the hip until the pelvis begins to move.
Make sure that the knee is flexed when evaluating hip flexion so that the hamstrings are relaxed. The knee should be extended to relax the rectus when extension is evaluated. Contractures in the knee can simulate limited hip motion.
Normal values in adults:
Extension: 10°–15°
Flexion: 130°–140°
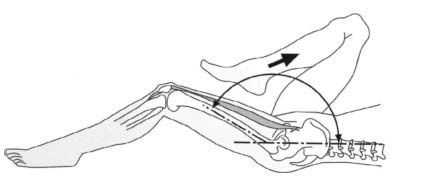
Fig. 4.5 Evaluating flexion using the Thomas grip.

Fig. 4.6 Evaluating hip extension.
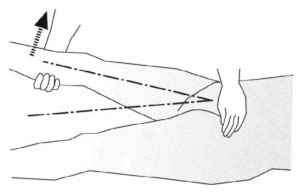
Fig. 4.7 Evaluating abduction in extension (one hand holds the anterior superior iliac spine).
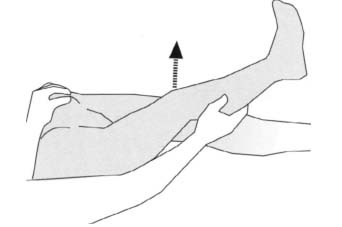
Fig. 4.8 Evaluating adduction in flexion (with slight flexion so that the leg may be lifted over the contralateral leg).
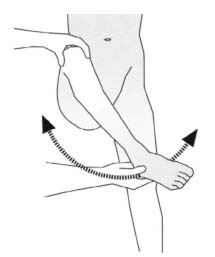
Fig. 4.9 Evaluating rotation in 90° flexion with the patient supine.
Abduction and Adduction
Examination in extension. Immobilize the pelvis with one hand so that your thumb and small finger palpate the anterior superior and inferior iliac spines. With this action, compensatory movement of the pelvis is readily detectable. The extended leg is abducted until passive motion of the pelvis is detected (Fig. 4.7). To test adduction, place the leg being examined in slight flexion and lift it over the contralateral leg. Another option is to immobilize the contralateral leg with the Thomas grip. This makes it possible to adduct the leg even in full extension (Fig. 4.8).
Normal values in adults:
Abduction: 30°–45°
Adduction: 20°–30°
Examination in 90° flexion
This examination can be used in adults in addition to the examination in extension. In newborns, it is the only way to measure abduction and adduction because of physiologic flexion contracture. As in the examination in extension, immobilize the two anterior superior iliac spines with one hand while abducting the flexed leg from the vertical position until the pelvis begins to tilt in the transverse plane. Proceed similarly to evaluate adduction.
Normal values in adults:
Abduction: 60°–70°
Adduction: 20°–30°
Internal Rotation and External Rotation
Hip rotation is usually evaluated in children with the patient prone and the hip extended (Fig. 4.9). In adults, the examination may also be performed with the patient supine and the hip flexed 90°. When performing the examination with the patient supine, make sure that the axis through the two iliac spines is perpendicular to the axis of the body. Move the hip while monitoring the movement of the iliac spines until passive motion of the pelvis is detected. When performing the examination with the patient prone and the knee flexed, place your hand on the sacrum to immobilize the pelvis.

Fig. 4.10 Drehmann test in a child. The thigh moves into compensatory external rotation as flexion increases.
Normal values in adults (in extension):
External rotation: 40°–50°
Internal Rotation: 30°–40°
Normal values in adults (in flexion):
External rotation: 40°–50°
Internal rotation: 40°–45°
Specific Tests for Adolescents and Adults
Drehmann Test
In a slipped capital femoral epiphysis, the thigh will move into compensatory external rotation as hip flexion increases (Fig. 4.10).
Ludloff-Hohmann Test
The knee can be completely extended when the hip is in flexion and adduction because the relative shortening of the thigh relaxes the hamstrings. Positive results are a sign of hip dysplasia.
Fulcrun or Stinchfield Test
In the presence of proximal femur, femor neck, or subcapital pathology such as stress fractures, holding the heel with the hip extended and pressing down on the midfemur will elicit groin pain.
Clinical Examination of Newborns and Infants
When examining the hip in children and newborns, obtaining a precise history is essential (see also Patient History). Inquire about a history of hip dysplasia in the family, whether the child is the first born, about breech presentation, details of delivery, the size of the child, the presence of other position anomalies, and differences in kicking motions. The type of pain can also be a sign because small children especially will present with referred pain into the knee. Even temporary pain with exercise can be an early sign of hip dysplasia. Sometimes “start-up” pain will be present, which children may barely notice. In some cases, the only sign will be gait irregularity. Other causes of such symptoms aside from hip dysplasia include an undiagnosed neurologic disorder, spasticity, or flaccid paralysis. Limps are categorized in various forms as discussed above. The Trendelenburg gait, Duchenne antalgic gait, leg shortening, and a fused joint should be distinguished. Examination of leg length can provide crucial information, particularly in the case of unilateral hip dislocation, where the affected leg appears shortened. Leg length is best evaluated with the child supine and the hips and knees flexed 90°. If this type of apparent leg shortening is present, one could estimate the difference between the legs by the level of the knees. The appearance of the soft tissue would also alter in a fully dislocated hip. Additional skin folds would be present.
Assessing Range of Motion
The differences in technique in the examination of newborns are due primarily to the physiologic flexion contracture in newborns, which precludes evaluation of hip abduction and rotation in extension. The examination is performed with the baby supine with hips and knees in 90° flexion. Make sure that the axis through the two superior iliac spines is horizontal to the examining table and perpendicular to the axis of the baby’s body. Estimate the flexion contracture before performing the examination. It can vary, but will generally be about 20°–35°.
Normal values for abduction and rotation in newborns fluctuate and are difficult to specify. Haas’ studies cite the following ranges of motion:
Normal values in newborns:
Internal rotation: 50°–70°
External Rotation: 75°–105°
Abduction: 65°–90°
According to studies by Harris, the range of abduction decreases in the first 9 months of life to 60°–70°. A range of abduction of less than 50° at birth can be regarded as abnormal. It is important to compare findings with the contralateral side in each case. Tonnis cites a difference between sides of 10°–30° for hip dysplasia and 30°–40° for dislocation. Differences between the sides in the range of abduction can also be the result of a deformity with pelvic obliquity. Symmetric bilateral limited abduction occurs in bilateral hip dysplasia or dislocation.

Fig. 4.11 Congenital hip dysplasia can simulate a shortened leg with asymmetric skin folds.
Range-of-motion testing can include estimation of femoral anteversion.
With the child supine, hold the leg to be examined with the hip and knee flexed 90° in 0° rotation. Palpate the greater trochanter with the other hand. Now internally rotate the leg to maximize lateral displacement of the greater trochanter. Internal rotation now corresponds to anteversion. The angle of anteversion is 30°–40° at birth and decreases to values of 10°-15° in adults.
Specific Examinations for Hip Dysplasia
• Inspection
Two anomalies consistent with hip dysplasia may occasionally be detected by inspection. One of these is the decrease in leg length resulting from subluxation of the femoral head; the other is asymmetry in skin folds. Leg shortening is most readily recognizable when you hold the child supine with the hips and knees flexed 90°. Sit in front of the child so that the child’s knees are at the level of your eyes.
| Associations: |
| — Positive family history |
| — Abnormalities during pregnancy (breech presentation) |
| — Other deformities (clubfeet) |
| — Asymmetric skin folds in the glutei |
| Signs: |
| — Range of abduction less than 50° |
| — Positive snapping phenomenon (Ortolani, Barlow) |
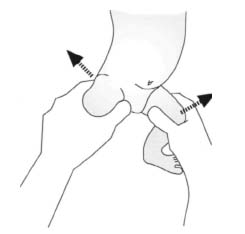
Fig. 4.12 Ortolani test in examination of the hip in new-borns.
Asymmetric skin folds in the adductor and buttocks region are the result of superior protrusion of the femoral head on the affected side; the soft tissue of the thigh is too long for this pathologic anatomical configuration and forms folds (Fig. 4.11). However, this is not a specific sign (Table 4.2) as it can occur in up to 30% of children with normal hips. Asymmetrical folds may also be observed in scoliosis.
• Palpation
There are three situations in developmental dysplasia of the hip. The first is a dislocated hip, the second a dislocatable hip, and the third a subluxatable hip.
• Ortolani Test
A snapping sound in the first few days and weeks of life suggests an unstable hip (Fig. 4.12). Sit in front of the supine newborn. With one hand, grasp the leg to be examined by the flexed knee so that your thumb is touching the medial thigh and your second finger and ring finger are touching the greater trochanter. Bring the contralateral hip into maximum flexion with your other hand by grasping the knee so that the pelvis is immobilized. Now flex and slightly adduct the leg to be examined. In this position, apply slight anteroposterior (AP) pressure to the knee you are holding with your hand. This will cause posterior subluxation of the femoral head. Abduct the hip under slight pressure. Apply slight pressure to the greater trochanter. In a positive test, you will hear a characteristic snapping sound during the abduction motion as the femoral head reduces into the acetabulum.
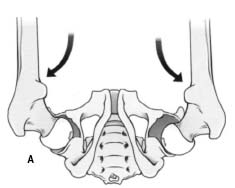
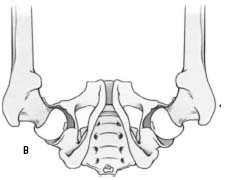
Fig. 4.13 Barlow dislocation test.
• Barlow test
In this examination, the hips are brought into intermediate abduction, and pressure is applied to the greater trochanter to evaluate reduction (Fig. 4.13). Then try to dislocate the hip by applying posterior and lateral pressure to the femoral head.
Neurologic Examination
Examining the Muscles
Not every nerve root has a specific corresponding muscle.
To maximize clinical information, examining the muscles according to their function is recommended. They are then evaluated according to the muscle grading chart.
Flexors
Primary flexor: iliopsoas (femoral nerve, Ll, 2, and 3).
The iliopsoas is the primary flexor. To test it, have the patient sit and let his or her legs dangle over the side of the examining table. Stabilize the pelvis by placing your hand on the iliac crest and having the patient lift the thigh off the table. Press on the distal portion of the thigh with your other hand to determine maximum resistance. Use both hands with strong patients (Fig. 4.14). Repeat the test on the contralateral side for comparison.
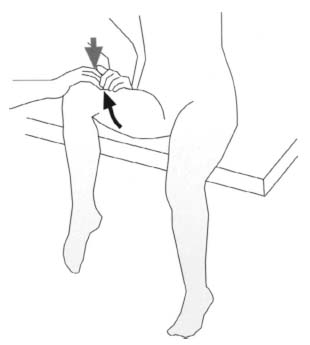
Fig. 4.14 Evaluating the iliopsoas.
Extensors
Primary extensor: gluteus maximus (inferior gluteal nerve, S1).
To test the gluteus maximus in isolation, have the patient lie prone with the knee flexed. Place your arm over the patient’s iliac crest to stabilize the pelvis before instructing the patient to lift the leg. Provide resistance to this motion by pressing against the distal thigh with your other hand. Palpate the muscle tone during this examination. Repeat the test for the contralateral side.
Abductors
Primary abductor: gluteus medius (superior gluteal nerve, L5).
To evaluate abduction, place the patient in a lateral position and stabilize the pelvis at the iliac crest. Have the patient abduct the leg against your resistance. Another option is to examine the patient supine with the leg abducted about 20°. Again, instruct the patient to abduct the leg against your resistance.
Adductors
Primary adductor: adductor longus (obturator nerve, L2, 3, and 4).
To evaluate adduction, have the patient adduct the abducted leg against your resistance (Fig. 4.15). Another option is to examine the patient supine. Again, instruct the patient to adduct the abducted leg against your resistance.
Examining Sensation
Findings on sensation testing are easier to evaluate than muscular findings because the sensory supply is divided into demarcated dermatomes (Fig. 4.16) that are relatively similar among all patients.
Dermatome L1 covers a transverse band along the anterior aspect of the proximal thigh directly distal to the inguinal ligament.
Dermatome L3 extends in an oblique band proximal to the knee.
Dermatome L2 lies precisely between these two. Dermatome L4 includes the area of skin on the medial thigh; dermatome L5 supplies the lateral calf including the dorsum and medial edge of the foot.
Dermatome S2 supplies a long strip along the posterior aspect of the thigh from the fold of the buttocks to the popliteal fossa.
Dermatome S3, often clinically significant because of the lateral femoral cutaneous nerve, is a wide oval area located on the lateral aspect of the thigh.
Dermatomes S3 through S5 are arranged in three concentric rings around the anus, from medial to lateral.
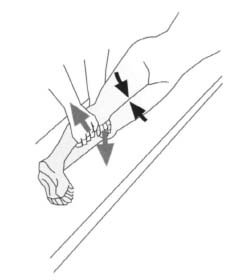
Fig. 4.15 Evaluating the hip adductors.
4.3 Radiology
Standard Views
Standard views of the hip include the AP radiograph of the hip and lateral radiograph of the hip.
The AP radiograph is used to determine the neck-shaft angle and assess possible varus or valgus deformity. It can be used for detecting fractures of the ipsilateral anterior pelvic ring, acetabulum, and femoral head and neck; for confirming dislocations of the hip; and for preoperative evaluation of the vertical origin of the lumbar spine where it exits the sacrum. It may be used in preoperative planning for leg-length operations.
The lateral radiograph demonstrates the anteversion of the femoral neck, the anterior and posterior cortex of the femoral neck, the ischial tuberosity, and rotation and displacement of the femoral head in fractures.
The AP radiograph is prepared with the patient supine with the legs in slight internal rotation to compensate for anteversion of the femoral necks. If the entire pelvis is to be imaged, the ray is centered on the middle of the pelvis; if a hip is to be imaged, it is centered on the respective femoral head.
The lateral radiograph is taken with the patient supine. The affected leg is extended, and the opposite leg is lifted and abducted (Fig. 4.17). The cassette is placed along the side of the affected hip with the ray centered on the groin and inclined 20° cranially from horizontal. This permits calculating the angle of anteversion as described by Dunn, Muller, and Rippstein (see section Hip Dyplasia, p. 153).
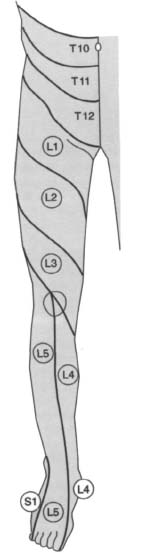
Fig. 4.16 Sensory dermatomes of the lower extremity.
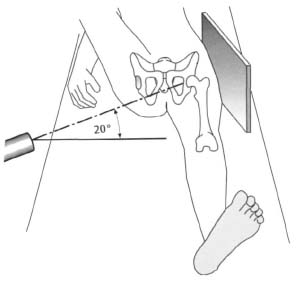
Fig. 4.17 Positioning for the lateral radiograph of the hip.
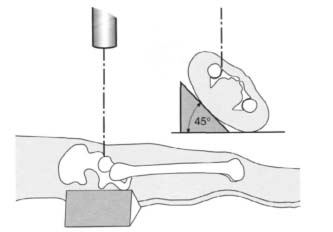
Fig. 4.18 Technique of the anterior oblique radiograph (obturator view).
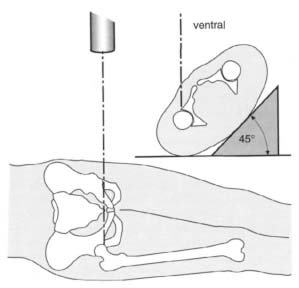
Fig. 4.19 Obtaining the posterior oblique radiograph (iliac wing view).
Special Views
Special views include inlet and outlet views of the pelvis, variations of the lateral radiographs, various oblique views, Lauenstein views, AP radiographs with altered settings, views for preoperative planning, and special views for precise evaluation of the acetabulum and the femoral neck.
In a trauma setting, inlet and outlet views of the pelvis can be helpful in defining a fracture detected in the AP radiograph. The patient is supine with the legs extended for both views. For the inlet view (Fig. 9.37), the central ray is angled 40° caudad and enters the midline at the level of the anterior superior iliac spine. Forthe outlet view (Fig. 9.39), the central ray is angled 40° cephalad and enters at the inferior aspect of the pubic symphysis.
The lateral radiographs mentioned in the previous section can be varied by altering the projection. Epiphyseal dislocation can be documented precisely in a straight lateral projection. A vertical projection, i.e., inclining the projection 20° cranially from horizontal (see above), is especially suitable for documenting anteversion and a slipped epiphysis. A horizontal projection (Sven Johnson) is useful as a second imaging plane if fractures of the femoral neck are to be internally fixed.
The oblique radiographs (Judet views see also p. 434
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








