CHAPTER 5 HIP
A ARTICULAR TESTS
FAIR test
Technique
Clinical context
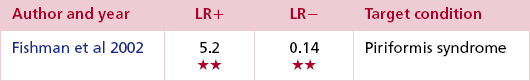
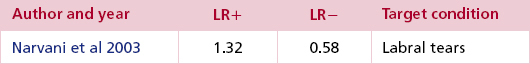
The FAIR test gets its name from the acronym generated by the principal elements of this test (Flexion, Adduction and Internal Rotation). The list of possible structures that can be incriminated by a positive FAIR test naturally results in a test with low specificity. There is some evidence, however, that demonstrates its sensitivity in the diagnosis of labral pathology/impingement and piriformis syndrome (Burnett et al 2006, Fishman et al 2002, Fitzgerald 1995, Hase & Ueo 1999, Jaberi & Parvizi 2007, Lewis & Sahrmann 2006, Mitchell et al 2003, Narvani et al 2003).
Most of the research comprises of small case series or larger retrospective studies of patients with known acetabular pathology or femoro-acetabular impingement (FAI). While the precise prevalence and cause of labral pathology is unknown, the population most likely to present is the younger patient with groin or hip pain (see McCarthy test, p. 156; McCarthy & Busconi 1995, Narvani et al 2003). A typical presentation would be a female patient in her mid-thirties with groin pain which is provoked by flexion activities such as driving or squatting and where certain movements are accompanied by a click. Some patients may also report lumbar or buttock pain provoked by activity, impact or load-bearing. There is a general lack of consensus concerning the significance of other findings such as a history of trauma, congenital or developmental hip abnormalities, movement impairment and radiological changes (Burnett et al 2006, Fitzgerald 1995, Hase & Ueo 1999, Jaberi & Parvizi 2007, Lewis & Sahrmann 2006, Mitchell et al 2003, Narvani et al 2003). Impingement, scour/quadrant (see Variations) and FABER tests (see p. 160) are all additional tests used to help the clinician determine the necessity of further investigation such as magnetic resonance arthrography (MRA) and arthroscopy.
The absence of an agreed ‘gold standard’ diagnostic tool for labral injury introduces uncertainty when attempting to measure the sensitivity of the test, as the significance of a positive finding on examination cannot always be confirmed definitively by means other than surgery, with investigations such as MRI and MRA being of limited value (Standaert et al 2008). In a retrospective study of 66 patients, the FAIR test was positive in 95% of patients with an arthroscopically confirmed labral tear compared to only 79% detected by MRA (Burnett et al 2006). These findings were confirmed in two separate case series (Hase & Ueo 1999, Ito et al 2004). The lack of false negatives in these current studies prevents specificity being calculated. Although the FAIR test is part of the suggested examination for FAI there are several variations (see p. 155).
The use of the test for piriformis syndrome has been evaluated in a large cohort trial of 918 patients which found that a positive FAIR test was a valid predictor of the response to physiotherapy, injection or surgical treatment for this condition (Fishman et al 2002). A study of 15 cases of surgically proven piriformis/sciatic nerve compression following blunt trauma concluded that the combination of a positive FAIR test along with a history of trauma, buttock pain and/or radicular pain, intolerance to sitting and tenderness over the sciatic notch were highly indicative of piriformis adhesions and should guide the need for referral for EMG (Benson & Schutzer 1999).
Clinical tip
Placing the hip in flexion, adduction and internal rotation will cause either compression or stretch of many hip structures including the ischiofemoral ligament of the hip, iliopsoas tendon and bursa, pectineus, adductor longus, sartorius, tensor fascia lata, piriformis and the glutei. Inevitably the hip joint itself is tested and the findings may help to isolate the first signs of joint pathology, such as Perthes’ disease in children for example (Woods & Macnicol 2001). The FAIR test is not capable of distinguishing between specific structures or pathology and the clinician is reliant on other information gleaned from the patient including the history, other physical findings and the results of pertinent investigations.
| EXPERT OPINION | COMMENTS |
|---|---|
 | FAIR test |
| Useful as a non-specific test for a range of hip pathology. A diagnosis of femoro-acetabular impingement is likely if the patient’s symptoms are typical, the test is positive and they have a ‘C’ sign (when asked to indicate the area of pain, they grasp the area of the greater trochanter with their thumb and index finger). |
Variations
The scour/quadrant/flexion adduction test is a modification where the hip is passively flexed to 90° and adducted. The clinician’s hands are interlocked and placed over the patient’s flexed knee. Leaning over the knee so that the examiner’s body weight can be used to good effect, a compressive force is applied through the longitudinal axis of the femur. Small passive movements are made into flexion and extension in order to ‘scour’ the joint (Fig. 5.2). A positive test is indicated by reproduction of the patient’s symptoms.
McCarthy test
Technique
Clinician position
The affected hip is taken into full passive flexion, with one hand supporting the flexed knee and the other supporting the foot (see Fig. 5.3).
Action
External rotation is then added as the affected hip is gradually taken down towards extension (see Fig. 5.4). If this does not elicit a positive response, the manoeuvre is repeated with the addition of internal rotation instead.
Clinical context
The role of the labrum in the symptomatic hip and the diagnosis of femoro-acetabular impingement (FAI) are comparatively new areas of study and the evidence concerning the clinical diagnosis and the most appropriate investigations and treatment is uncertain. The labrum does have a propensity to degenerate with age and this was demonstrated in a cadaver study where degenerative tears were identified in 90% of specimens (McCarthy et al 2003). Interestingly, it is not the ageing population that report labral problems as the accompanying joint disease inevitably takes precedence. The younger patient with groin or hip pain is most likely to present and 22–55% of patients with this profile were found to have labral tears (Narvani et al 2003). A typical presentation would be a female patient in her mid-thirties with groin pain which is provoked by flexion activities such as driving or squatting and where certain movements are accompanied by a click. Some patients may also report lumbar or buttock pain provoked by activity, impact or load-bearing.
Apart from surgical confirmation, there is no agreed ‘gold standard’ diagnostic tool, with neither MR arthrography nor MRI showing sufficient sensitivity or specificity to confirm FAI (Standaert et al 2008). The detection of FAI, labral tears or chondral lesions at the hip therefore largely relies on a combination of the history, signs and symptoms, the outcome of physical tests and imaging studies to guide both diagnosis and management. There has been shown to be some correlation, however, between acetabular tears and pre-operative reports of clicking and giving way (McCarthy & Busconi 1995, Narvani et al 2003).
Clinical tip
Acetabular tears may present in young, athletic patients where the predominant symptoms are groin pain, often accompanied by clicking, a catching sensation and/or giving way. A traumatic history involving hip flexion, abduction and knee extension is common (DeAngelis & Busconi 2003), although not essential, as a significant proportion of patients in one study reported an insidious onset (Burnett et al 2006).
| EXPERT OPINION | COMMENTS |
|---|---|
 | McCarthy test |
| Useful as a non-specific test for hip joint pathology. A positive test is not sensitive or specific for labral lesions. However, patients who report reproduction of their click and pain on this test seem to get better outcomes post surgery. |
Variations
The snapping hip test (sometimes known as the clicking hip test or the extension test) is an active version of the McCarthy test and used to distinguish extra-articular snapping of the iliopsoas tendon as it passes over the femoral head or the iliopectineal eminence anteriorly. Iliopsoas syndrome is a source of groin pain and clicking and is most commonly encountered in young, athletic patients. It may also be associated with inflammatory or degenerative arthritis in the hip, or present post hip arthroplasty. The patient lies supine and actively brings the affected hip into a flexed, adducted and internally rotated position. The clinician places one hand over the anterior aspect of the hip joint to palpate for snapping. The other hand is then free to guide the movement of the patient’s leg downwards. The patient actively extends, abducts and externally rotates the hip from the starting position. A positive test is indicated by pain and reproduction of the patient’s familiar snapping sensation (Magee 2008). Alternative causes of extra-articular snapping are the tensor fascia lata/gluteus maximus slipping over the greater trochanter and the iliofemoral ligament movement over the anterior joint capsule.
Related tests
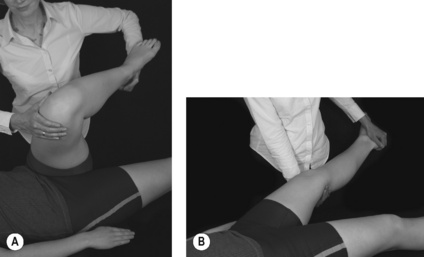
Other labral tests have attempted to identify the location of the tear (Fitzgerald 1995). For the posterior labral tear test (Fig. 5.5) the hip is taken into in a flexed, adducted and internally rotated position (Fig. 5.5A) and then passively moved into the reverse pattern of extension, abduction and external rotation (Fig. 5.5B). The opposite manoeuvre is used for the anterior labral tear test. The hip starts in full flexion, external rotation and abduction and is then moved passively into extension, internal rotation and adduction. Pain and/or clicking reproduced with either of these manoeuvres would be suggestive of a labral tear. Fitzgerald’s (1995) study prospectively examined patients with surgically verified labral pathology and although 54 of 55 patients reported a positive finding (pain and/or a click) on one of these tests, it was not possible to specifically isolate the exact site of the lesion.
| EXPERT OPINION | COMMENTS |
|---|---|
 | Posterior labral tear test |
| The posterior labral tear test can be adapted so that the hip is taken into extension over the edge of the couch. |
The log roll test can also be used to detect pathology of the acetabular labrum or identify hip joint laxity. The patient lies supine with the lower limbs relaxed in a neutral position. Standing on the affected side, the hands are positioned over the anterior aspect of the patient’s thigh, just above the knee. The thigh is then passively rolled into full internal rotation and then full external rotation. The test may elicit a click in the presence of a labral tear. An increase in the range of movement of the affected hip can indicate laxity (Austin et al 2008; see torque test, p. 163).
| EXPERT OPINION | COMMENTS |
|---|---|
 | Log roll test |
| The log roll test can be useful as a general assessment for hip pathology. As the patient lies supine, excess external rotation caused by hip instability/laxity is indicated by the foot of the affected leg rolling outwards. |