Fig. 4.1
Preoperative photograph of a pinpoint wound on the volar aspect of the distal phalanx of the index finger on the nondominant hand secondary to high-pressure injection of paint (From: Rosenwasser and Wei [41], with permission from Wolters Kluwer Health. Courtesy Robert Strauch, MD, New York, NY)
The Evidence
Epidemiology
The incidence of reported high-pressure injection injuries in the medical literature coincides with the development of more complex machinery in the last half of the twentieth century, when increasingly higher-pressure guns were used to inject paint, grease, concrete, plastic, and fuel [2]. Some authors noted that paint gun injuries usually occurred in painters who were accustomed to low-pressure guns and switched to high-pressure airless guns [3]. On average, 1 of 600 hand traumas are due to high-pressure injection injuries, and 1–4 cases present to large surgical hand centers annually [4]. The patient is most commonly a young male laborer involved in industrial cleaning, painting, lubricating, or fueling, and injuries are sustained when the operator attempts to clean the nozzle with a finger or a cloth. The nondominant hand is most commonly injured with more than 50 % of these injuries sustained in the index finger [5, 6]. The thumb is the second most commonly injured digit, followed by the palm, but high-pressure injection injuries may occur anywhere along the upper extremity [7].
Pathophysiology
The injury process from high-pressure injections may be divided into four main components: (1) initial injury, (2) chemical irritation, (3) inflammation, and (4) secondary infection.
Initial Injury
High-pressure injection injury begins with the initial force delivered to the tissues. A pressure of 100 psi (7 bar) is sufficient for skin penetration, while high-injection pressures can range from 3000 to 12,000 psi depending on the specific application of the apparatus with velocities up to 400 mph [7–9]. Examples of systems that operate around 3000 psi include airless high-pressure spray guns first developed in the 1950s that use hydraulic pumps to deliver paint, as well as reinforced hydraulic pipes used in many industries such as coal mining, agriculture, and construction, that contain pressurized oils [10]. The higher end of pressurized systems includes diesel engines that compress fuel up to 12,000 psi before releasing its contents through a nozzle to the combustion chamber. In the event of nozzle malfunction or blockage, these pressures may even be higher [11]. The kinetic injury of a grease gun injury to the finger is calculated to be equivalent to a 1000-kg (2205-lb) weight falling from a height of 25 cm (9.8 in.) [12]. Injuries are less severe when a small distance separates the injection source from the skin. Nevertheless, high-pressure jets can penetrate and infiltrate the subcutaneous tissues even without direct bodily contact [13, 14].
The force of the injection dissects along planes of least resistance that tend to follow neurovascular bundles in the digits. When the fibrous sheaths of the stouter annular pulleys are encountered, the force of the injected substance usually deflects and passes around the tendon sheath and underlying bone [15]. However, if the force penetrates the tendon sheath over the thinner, membranous cruciate pulleys that overlie the joints of the hand, the injected material may distend and disrupt the tendon sheath itself. Mid-palmar injections are usually limited to material superficial to the palmar aponeurosis, with occasional deposition in the deep palmar space injuring bones, muscles, and vessels, and through and through penetration entering the dorsum of the hand [11].
Following the forceful entry of the injected substance, compression, decreased perfusion pressure, venous hypertension, and capillary leaking initiate a cycle of swelling, edema, and further compression much like a typical compartment syndrome. Caustic chemical reaction, secondary to the injected material, initiates a second hit with a violent inflammatory response magnifying the injury. This then cycles back as increased tissue pressures further compromise blood flow, triggering vasospasm, thrombosis, and ultimately ischemia.
Local Chemical Irritation
Paint, grease, hydraulic fluid, diesel fuel fluid, paint thinner, mud, toluene, molding plastic, paraffin, and cement are the most commonly injected substances. Many of these chemicals are intrinsically cytotoxic, causing necrosis and inciting inflammatory responses. In particular, paint and turpentine have been shown to be particularly harmful agents, and the severe toxicity of paint has led some authors to recommend primary amputation as the initial treatment [16].
The chemical composition of paint can consist of up to 40 raw materials, but they may be divided into three main parts: a solvent that evaporates shortly after it is applied, a pigment that provides color, and a transport vehicle or binder that acts as an adherent [10]. Each of these constituents can damage tissue directly. The vehicle or binder may be an unsaturated or drying oil, or it may be a synthetic polymer such as an alkyd resin.
Water-based latex paints were introduced in the late 1940s, and they differ in solvent and vehicle compared with oil-based paints, with substantially lower rates of amputation following latex paint injection than following oil paint injection (6 and 58 %, respectively) [10]. This difference is thought to be due to the reduced inflammatory potential of acrylic latex vehicles compared with the alkyd resins of oil-based paints. Turpentine and other paint thinners are a mixture of alkylated aromatic hydrocarbons designed to dissolve fats, and they cause lipid dissolution without a high-pressure etiology [17, 18]. The powerful detrimental nature of turpentine is demonstrated through its effects even when not injected into the body. The fumes can cause irritation of exposed mucous membranes and bronchial inflammation, predisposing individuals with chronic exposure to pneumonia, chronic nephritis, and dermatitis [14].
In contrast, the chemical contents of grease are less inflammatory than both paint and paint solvents. Grease contains 88 % mineral oil, along with graphite and detergent, and produces chronic granulomas rather than direct chemical irritation [19]. Water, air, and small quantities of veterinary vaccine have been reported to produce minimal damage and good outcomes even with nonsurgical management, further emphasizing the impact of direct chemical irritation on treatment and outcomes [7, 20, 21].
Systemic Inflammatory Response
Experimental injection of oils, waxes, diesel oil, and turpentine into human and animal tissues have been shown to cause acute and chronic inflammation with granulomatous changes [11, 14, 22]. Soya alkyd, a polymeric resin vehicle for paint, produces greater inflammatory responses and is more caustic than mineral spirits, turpentine, xylol, and acrylic latex [10]. Postinjection sectioning of resected tissue shows substitution of normal connective tissue and fat, with whorls of proliferative granulation tissue and fibroblasts. Macrophages containing vacuoles of the injected material, as well as polymorphonuclear leukocytes, lymphocytes, and plasma cells are present [17].
Secondary Infection
The ischemic conditions and tissue necrosis that occur following the initial injury creates an environment for bacteria to thrive [10, 23]. However, some authors have found wound infection to be rare, due to the injected material being an organic chemical that does not support bacterial growth [8]. Although wound cultures have not been consistently obtained for injection injuries, infection rates have ranged widely from 1.6 to 60 % [6, 11, 24, 25]. In the literature review performed by Hogan and Ruland, wound cultures were reported for 126 out of 435 patients, of which 53 were positive (42 %) [20]. Most of the infections were polymicrobial. Infection is fostered by necrotic tissue and the reluctance to aggressively debride these injection injuries early may allow infection to take hold.
Clinical Presentation and Indications
Initially, small punctate lesions may be the only visible sign of injury on the skin, with minimal or no pain. Some patients have seen as many as seven doctors before the significance of their injury was recognized. Such innocuous presentation of a painless wound often delays patients from seeking medical evaluation. The average time to physician evaluation averages nearly 9 h. However, as swelling develops, pain and paresthesias occur with loss of perfusion, and the urgency of the clinical presentation becomes obvious as the finger becomes bloated, edematous, tense, pale, and cold [7].
Appropriate initial management of this injury mandates a high index of suspicion by the physician who first encounters the patient. In the presence of radiopaque materials, radiographs can be effective and helpful in determining the spread of injected material; however, some material may be radiolucent, or lucent areas may represent air [26, 27] (Fig. 4.2a, b). If laboratory evaluation occurs within a few hours after injury, it may reveal an elevated white blood cell count and be accompanied by lymphadenitis and lymphangitis [16].
Fig. 4.2
The injected material is radiolucent and therefore cannot be seen on the preoperative AP (a) and lateral (b), radiographs of the index finger. c Intraoperative photograph of the markings for a planned Bruner incision for debridement. d Photograph of the incision of the volar aspect of the finger showing the appearance of the injected material in the subcutaneous space. e Post-debridement photograph following the removal of foreign injected material with careful preservation of neurovascular structures (From: Rosenwasser and Wei [41], with permission from Wolters Kluwer Health. Courtesy Robert Strauch, MD, New York, NY)
Initial management should include elevation of the limb, tetanus prophylaxis, systemic prophylactic antibiotics, and analgesia. Digital blocks should be avoided because they may add to swelling and vasospasm in a digit that is already at risk. Wounds should be left open, with no attempt to obtain primary closure in the emergency department setting, and ice is discouraged due to the need to optimize perfusion of the injected hand [4].
Management
Surgical Debridement
The benefits of early and aggressive surgical debridement have been known since the initial reports of injection injuries [1]. Ensuring the entire zone of injury is debrided, decompressing compartments, exploring and incising tendon sheaths, removing injected material, and using ample saline irrigation are all critical steps in the management of high-pressure injection injuries to the hand (Figs. 4.2c–e and 4.3a–k). Surgical removal of foreign material to avoid ischemic gangrene and to reduce fibrosis and scarring are also important steps [16]. Delayed surgery has been associated with increased morbidity and higher amputation rates [2, 16, 27].

Fig. 4.3
a through c: Photographs of the left index finger of a patient who was transferred from another institution after having had only catheter irrigation of a paint injection injury without formal debridement. d Intraoperative photograph during thorough surgical debridement. e through g: Photographs showing that the wounds were left open to heal by secondary intention. h through k: Follow-up clinical photographs of the healed wound. The patient had excellent motion (From: Rosenwasser and Wei [41], with permission from Wolters Kluwer Health. Courtesy Robert Strauch, MD, New York, NY)
Some authors have recommended amputation as the primary treatment for high-pressure injection injuries to the hand [31]. However, Pinto et al. reported an 84 % salvage rate with open wound packing, repeat debridement, and delayed closure with only four amputations in 25 patients [6]. They utilized a wide exposure with Bruner palmar digital incisions and thoroughly debrided all devitalized tissue in the zone of injury, while removing injected material and preserving the neurovascular structures. Repeat debridement was performed at 24–72 h later as necessary. Alternative incisions may be used such as a midaxial incision to achieve full exposure and in some cases may be preferred over palmar flaps that might be compromised from the injury itself (Fig. 4.4). Following debridement and excision of injected material, irrigation with normal saline or lactated Ringer injection may be used, whereas organic solvents should be avoided, as they lead to further inflammation and tissue damage.
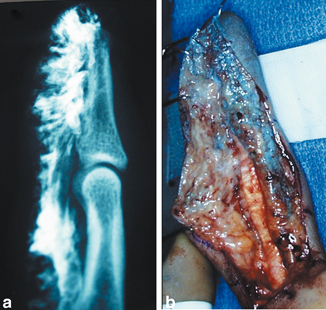
Fig. 4.4
A lateral radiograph (a) and clinical photograph (b) of an index finger demonstrating the appearance of radiopaque paint in a patient who sustained a high-pressure injection injury. An extensile midaxial incision was used to ensure adequate exposure of the zone of injury (From: Rosenwasser and Wei [41], with permission from Wolters Kluwer Health. Courtesy Robert Strauch, MD, New York, NY)
Steroids and Anti-Inflammatory Agents
Treatment of high-pressure injection injuries with systemic steroids was reported as early as 1962, when Bottoms advocated the use of dexamethasone, reporting the effectiveness of its anti-inflammatory properties [32]. However, more recent evidence challenges the utility of steroid use in the setting of high-pressure injection injuries. Some authors advocate the routine use of steroids in all patients, while others voice concerns that steroid suppression of the leukocyte response will increase the risk of superinfections [14, 33, 34].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








