Pediatric pelvic and acetabular fractures are rare injuries. They are almost always the result of a high-energy injury mechanism. A full trauma protocol should be instituted, having a high index of suspicion for associated life-threatening injuries. In the past, it was recommended that almost all of these injuries be treated nonoperatively. However, pelvic and acetabular fractures do not all remodel well. Prospective studies are needed to establish optimal treatment guidelines. Until then, in the presence of instability or significant displacement, operative fixation by a pelvic and acetabular fracture specialist should be considered to allow the best possible outcome.
Key points
- •
Pediatric pelvic fractures are markers of high-energy injuries and are unlikely to be the cause of death, but are a sign of other associated life-threatening injuries such as head or thoracoabdominal trauma.
- •
Pelvic hemorrhage may go unrecognized in pediatric patients because of a more effective vasoconstriction mechanism and the ability of the immature periosteum to tamponade bleeding.
- •
Operative indications for pediatric pelvic fractures are based on amount of displacement and degree of instability and are indicated to prevent deformity and long-term disability and pain.
- •
Pediatric posterior wall acetabular fractures may be misinterpreted as small fragments when magnetic resonance imaging (MRI) reveals a large osteocartilaginous wall fragment requiring operative fixation. Most pediatric acetabular fractures involving the posterior wall require MRI to better judge the size of the fracture fragment(s).
- •
There is little evidence for the optimal treatment of triradiate acetabular fractures, and outcomes are poor for the most severe crush injuries.
Introduction
Pediatric pelvic and acetabular fractures are rare, with a reported incidence of 1 per 100,000 children per year. Pediatric pelvic fractures caused by high-energy injury mechanisms are a marker of impending death because of associated head and other injuries. Long-term outcome studies of pediatric pelvic fractures are lacking because of their rarity. Treatment can differ significantly between skeletally immature and skeletally mature pelvic fractures. Depending on the injury, the potential exists for long-term disability from residual deformity, growth disturbance, compensatory scoliosis, and pain. Literature specifically on pediatric acetabular fractures is even more scarce than literature on pediatric pelvic fractures. This article presents the anatomy, general considerations, classification systems, and treatment strategies for high-energy pelvic and acetabular fractures in skeletally immature patients based on the best available evidence and our own experience in treating these patients. Pediatric pelvic avulsion fractures, which are usually caused by low-energy mechanisms such as athletic events, are not addressed in this article.
Introduction
Pediatric pelvic and acetabular fractures are rare, with a reported incidence of 1 per 100,000 children per year. Pediatric pelvic fractures caused by high-energy injury mechanisms are a marker of impending death because of associated head and other injuries. Long-term outcome studies of pediatric pelvic fractures are lacking because of their rarity. Treatment can differ significantly between skeletally immature and skeletally mature pelvic fractures. Depending on the injury, the potential exists for long-term disability from residual deformity, growth disturbance, compensatory scoliosis, and pain. Literature specifically on pediatric acetabular fractures is even more scarce than literature on pediatric pelvic fractures. This article presents the anatomy, general considerations, classification systems, and treatment strategies for high-energy pelvic and acetabular fractures in skeletally immature patients based on the best available evidence and our own experience in treating these patients. Pediatric pelvic avulsion fractures, which are usually caused by low-energy mechanisms such as athletic events, are not addressed in this article.
Anatomy
Pelvis
The pelvis begins to form during the first 2 months of embryologic development. The acetabulum, formed by the convergence of the ilium, ischium, and pubis, begins to cavitate and by the eighth week a fully developed hip joint exists. By 9 weeks, endochondral ossification of the ilium begins, with the ischium beginning to ossify at about 16 weeks, and the pubis a few weeks following this. The epiphyseal centers of the pelvis, including the triradiate cartilage, are visible at this time.
The pubic symphysis, composed of thick cartilaginous endplates, has a variable rate of ossification until about age 10 years. The iliac crest and spines remain cartilaginous until adolescence, at which time secondary ossification centers develop along the anterolateral iliac crest at 13 to 15 years of age. As ossification of the wing advances posteriorly toward the posterior superior iliac spine, fusion to the rest of the ilium occurs from 15 to 17 years, with complete fusion often not occurring until age 25 years. The ilium is thought to develop normally based partly on the pull of the gluteal muscles on its outer wing.
Acetabulum
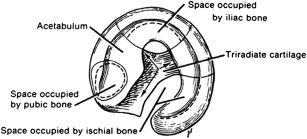
The first ossification center of the acetabulum begins in infancy as woven bone at the level of the acetabular fossa. The triradiate cartilage is composed of 3 secondary ossification centers at the periphery of the acetabulum, with the pubis, the ilium, and ischium each contributing to an arm of growth ( Fig. 1 ). These 3 secondary ossification centers begin to develop within the acetabular cartilage in the prepubescent period. The os acetabuli, part of the pubis, appears at 8 years of age, and develops into the anterior acetabular wall, with fusion normally by age 15 years. The acetabular epiphysis, the secondary ossification center of the ilium, appears between 8 and 9 years, and contributes to most of the roof of the acetabulum, and fully fuses by 18 years. The ischial epiphysis appears between 9 and 10 years with the secondary ossification center in the ischium continuing to develop through adolescence. Before the visualization of secondary ossification centers during adolescence, injuries to this region can be missed with radiographs.
The triradiate cartilage and other ossification centers contribute to the widening of both the pelvic ring and the acetabulum. Interstitial growth in the triradiate cartilage contributes to the height and width of the acetabulum, but much of the growth as well as its depth are stimulated by mechanical stimuli. The acetabulum cavitates as a result of the pressure of the femoral head and also symbiotically contributes to the normal development of the femoral head. As the triradiate cartilage grows and develops into the acetabulum it also grows outward, contributing to the length of the pelvic bones.
Pattern of traumatic acetabular dysplasia
Dysplasia caused by injury is distinct from developmental dysplasia of the hip (DDH). In DDH, the femoral neck is typically anteverted and the femoral head subluxes laterally and anteriorly while the pelvic ring remains symmetric and relatively unaffected. The acetabulum has a decreased lateral and anterior center edge angle. In posttraumatic hip dysplasia, proximal femoral anatomy is normal, but the true pelvis deforms and appears lengthened on the side of the injured acetabulum. The teardrop and inner wall of the acetabulum appear increased in size and the femoral head lateralizes. Patients usually have symmetric leg lengths but the leg can appear shortened because of the upward migration of the femoral head into the growth-arrested acetabulum. A positive Trendelenburg sign toward the uninjured side may be present because of an increased lever arm of the abductor muscle tendon-tendon unit on the injured side.
Cause of traumatic acetabular dysplasia
The exact cause of premature closure of the triradiate cartilage has yet to be elucidated. Rodrigues suggested that the hematoma that forms after injury ossifies creating a bony bridge that halts growth of the physis. Trousdale and Ganz suggested a combination of direct injury to the growth plate chondroblasts during the trauma and subsequent scarring as likely contributing to growth arrest. Bucholz and colleagues suggested that the hypoxia caused by traumatic disruption of precarious microcirculation to the chondroblasts causes growth arrest.
Animal studies have contributed to the knowledge on traumatic acetabular dysplasia. Delgado and colleagues found in a rat model that selective injuries to different flanges of the triradiate cartilage resulted in different patterns of growth arrest and deformity of the acetabulum. Gepstein and colleagues showed in a study of selective fusion of rabbit triradiate cartilage that injury to the ilioischial flange has the greatest negative effect on growth and development with 100% of rabbit acetabuli having dysplasia and 66% of hips dislocated by 9 weeks after iatrogenic injury.
General considerations
The Unique Characteristics of the Skeletally Immature Pelvis
Elasticity
The distinction between adult and pediatric pelvic fractures is not only related to anatomy and development but also to injury mechanism, associated injuries, and mortality. Depending on the age of the child, much of the pelvis is composed of cartilage, and the bone has thicker periosteum. These factors make the pediatric pelvis more elastic than the adult pelvis. Pediatric sacroiliac and pubic symphyseal joints are wider and thicker in children than in adults, and they are capable of absorbing a greater amount of force without frank rupture. These anatomic considerations may account for the lower incidence of pelvic fractures in children than in adults. Because the immature pelvis is more resistant to sustaining a fracture, when a fracture does occur, unless it is an avulsion fracture, it should be assumed that it is caused by a high-energy mechanism. When a pelvic fracture occurs in a child, there should be a high suspicion for associated head injury, thoracic injuries, and abdominal injuries.
Lower mortality
Even though pelvic fractures in children are harbingers of other associated life-threatening bodily injuries, children who sustain pelvic fractures have an overall lower mortality from pelvic fractures than adults. Over a 6 year period at a level I trauma center, of 57 children diagnosed with a pelvic fracture, only 1 patient had significant hemorrhage directly related to a pelvic fracture, and the 3 mortalities were caused by other injuries. Another retrospective study found similarly low mortalities in pediatric pelvic fractures.
Better hemorrhagic control
Skeletally immature pelvic fractures are associated with less blood loss than in adults. Because the thicker periosteum is more resistant to fracture, incomplete greenstick pelvic fractures can occur. The unruptured periosteum contains and tamponades bleeding fracture hematoma. Furthermore, children have vasculature that is more vasoreactive and bleeding vessels in the pelvis are more likely to effectively constrict, limiting hemorrhage. Although this is protective for the child, it also can mask earlier stages of hemorrhagic shock. When a child with a high-energy pelvic fracture is hemodynamically unstable and is bleeding into the pelvis, the trauma team should immediately stabilize the pelvis provisionally and aggressively resuscitate the child with blood and blood products, because the child is likely in late stages of hemorrhagic shock. However, mortality in a child with a pelvic fracture is usually not from the pelvic fracture but approximately 75% of time from an associated head injury.
Injury mechanism
The mechanism of injury is another distinction between adult and pediatric pelvic fractures, and may also be a factor in why mortalities in children are lower. Pediatric pelvic fractures are more likely to be the result of a pedestrian being struck by a motor vehicle than from a head-on motor vehicle accident, which is a common injury mechanism in adult pelvic fractures. Pedestrians are most likely to be struck on the side of the body, which is likely to cause a lateral compression injury. Lateral compression injuries are also associated with head and thoracic injuries, whereas head-on motor vehicle collisions are more likely to cause an anterior-posterior compression or open-book pelvic fracture, more commonly associated with life-threatening hemorrhage and death than lateral compression fractures.
Status of the triradiate cartilage
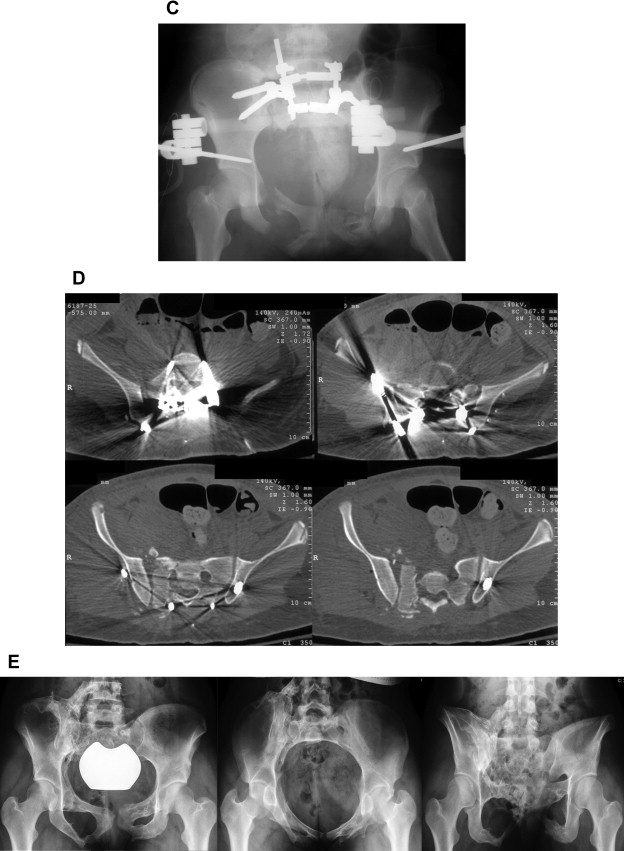
Deciding when to treat a child as skeletally immature or as an adult should largely be based on the status of the triradiate cartilage. Silber and Flynn performed a retrospective review of 166 pediatric pelvic fractures and evaluated several different radiographic parameters for gauging skeletal maturity, including the Risser stage, closure of the triradiate cartilage, closure of the ischial physis, closure of the proximal femur physis, and closure of the greater trochanter apophysis. They concluded that, in the context of pelvic fractures, the most reliable method of deciding on skeletal maturity was the status of the triradiate cartilage. Before triradiate closure, the pelvis is considered skeletally immature and can show injury patterns unique to this age group. Silber and Flynn found single, isolated pelvic ring injuries such as iliac wing fractures or isolated rami fractures 29% of the time in skeletally immature patients, which is an extremely rare pattern in adult patients. These isolated injury patterns are likely caused by the greater elasticity of the immature cartilaginous pelvis and thicker periosteum. After triradiate closure, injury patterns are identical to those of adults and can be treated as such ( Fig. 2 ). Therefore, one of the guiding principles of treating pediatric pelvic and acetabular fractures is the status of the triradiate cartilage. On average, the triradiate cartilage closes at 14 years in boys and at 12 years in girls.
Evaluation and initial treatment
The trauma evaluation begins following advanced pediatric life support (APLS) protocol, beginning with airway, breathing, circulation, and exposure followed by a full musculoskeletal examination evaluating the spine, pelvis, and extremities. The hips should be tested for range of motion to help determine whether there is a hip dislocation or acetabular fracture. A Morel-Lavallée lesion (internal deglovement) is uncommon in children but can be seen in overweight adolescents.
The pelvis should be palpated for tenderness and crepitus over the pubic rami, laterally over the iliac wings, and posteriorly over the sacrum. Pelvic stability should be evaluated with anteroposterior (AP) and lateral compression forces to the iliac wings. In an unstable pelvic fracture, this should only be performed once in order not to disrupt any clot that may have previously formed.
When a displaced pelvic fracture is diagnosed in a hemodynamically unstable patient, a pelvic binder or sheet should be placed during the trauma evaluation to decrease intrapelvic volume and potentially tamponade off any bleeding from vessels and bone. Vertically unstable pelvic fractures and hip dislocations after reduction should be treated with skeletal traction. If the patient does not respond to initial resuscitative measures and pelvic binder application, bleeding secondary to fracture is most often caused by bleeding veins or bone and is not arterial. Computed tomography (CT) scan with contrast shows a characteristic extravasating contrast blush, which is sensitive for arterial bleeding 80% to 84% of the time. More studies are needed to definitively determine the best treatment protocol; however, angiography is still the next step in the treatment algorithm at most trauma centers.
Open pelvic fractures can easily be missed and therefore suspicion should always be high in the setting of high-energy trauma. A thorough examination for blood around the urethral meatus, the vagina, the scrotum, and the rectum should be performed. A retrograde urethrogram should be performed by a urologic specialist to evaluate the urogenital pathway before placement of a Foley catheter if any suspicion exists for a urologic injury. If a bladder injury has occurred and a suprapubic catheter is placed, and if anterior fixation of the associated pelvic fracture is planned, the orthopedic surgery team should be present when the catheter is placed to ensure that it does not compromise future incisions. During the digital rectal examination, bony fragments in the rectal vault indicate an open pelvic fracture and high-riding prostate signifies urologic injury. Open pelvic fractures communicating with the colon or rectum usually require a temporary diverting colostomy to help prevent infection and osteomyelitis. The site of colostomy should be planned in conjunction with the orthopedic team in order to prevent interference with and contamination of future surgical approaches to the pelvis. An open pelvic fracture requires intravenous antibiotics and urgent irrigation and debridement and external fixation.
Pelvic fractures
Classification
Several classification systems exist for pediatric pelvic fractures. Quinby classified pediatric pelvic fractures into 3 groups based on a series of 20 patients less than 14 years of age. The classification was most useful for general trauma surgeons and was based on the severity of injury to multiple organ systems and who required laparotomy: Group I were mild or stable fractures not requiring laparotomy; group II were fractures with internal organ injury that require surgical exploration; group III were fractures associated with massive hemorrhage and multiple fractures. Watts later classified pelvic fractures in children as follows: simple avulsion fracture; fracture of the pelvic ring, either stable or unstable; acetabular fracture.
The Torode and Zieg classification is most widely used today ( Fig. 3 ). Type I fractures are avulsion fractures of bony insertions of muscles attaching to the pelvis, commonly occurring during a sporting event. Type II injuries are iliac wing fractures, usually caused by a direct force on the lateral side, such as in a pedestrian who is struck. Type III fractures are simple ring fractures involving the pubic rami or a pubic symphysis disruption. Type IV pelvic injuries are ring fractures or joint disruptions, resulting in instability of at least part of the pelvic ring. Type IV fractures include straddle injuries in which the bilateral superior and inferior pubic rami are fractured, combined fractures, or dislocations of both the anterior and posterior ring, as well as combined pelvic ring injury and acetabular fractures. Type IV fractures are more serious injuries associated with life-threatening internal injuries, and are more often associated with progressive growth disturbance and deformity. More recently, this classification was modified by using CT findings in addition to plain radiographs. The original classification was changed into type I, II, III-A, III-B, and IV. The difference between type III-A and III-B is that, in addition to an anterior ring injury, there is also a posterior ring fracture in type III-B.
Pediatric patients with closed triradiate cartilage are considered to be skeletally mature and therefore pelvic fractures in this group should be classified using the same system used in adult injuries, the Tile and Pennal classification system, later adopted by the Arbeitsgemeinschaft für Osteosynthesefragen/Orthopaedic Trauma Association (AO/OTA) classification system for pelvic fractures. Young and Burgess later modified this classification system to add subclassifications based on increasing amounts of force with resultant increased disruption of the pelvic ring. They also added a combined injury mechanism as a fourth class of pelvic ring disruption. This classification is important because the subgroups have different associated injury patterns, blood transfusion requirements, and mortalities. Furthermore, it helps guides treatment. Although this classification system does not specifically differentiate adults from children, it is applicable to skeletally mature adolescents, and in a skeletally mature adolescent the Tile and Pennal/AO/OTA system or the Young and Burgess system is more commonly used.
Diagnostic Imaging
Standard trauma films include an AP radiograph of the pelvis in addition to the lateral cervical spine and chest radiographs. Some trauma centers have stopped obtaining initial radiographs and use standard full-body screening CT scan instead. The normal pubic symphysis in very young children is 10-mm to 12-mm wide, whereas in adult patients the width of the symphysis is 2 to 4 mm.
Some clinicians have questioned the utility of regularly obtaining a CT scan in pediatric pelvic fractures, given the risks of radiation in pediatric patients and the question of whether or not CT scans result in a change of management. The addition of CT scans to standard AP pelvis radiographs in 62 patients who sustained pelvic fractures at a level I pediatric trauma center changed the classification in 9 patients (15%) and definitive management in 2 patients (3%). Given that most patients with trauma require CT scans to rule out associated head, thoracic, abdominal and pelvic visceral, and spinal injuries, CT scans should be obtained for any pediatric patient with suspected instability or significant anterior disruption, or when posterior ring disruption is suspected based on plain films. Acetabular fractures merit a CT scan to fully evaluate the articular surface. In addition, standard inlet and outlet views or Judet radiographic views are performed in pelvic and acetabular fractures respectively. CT scans are typically not necessary for apophyseal avulsion fractures that occur from low-energy mechanisms.
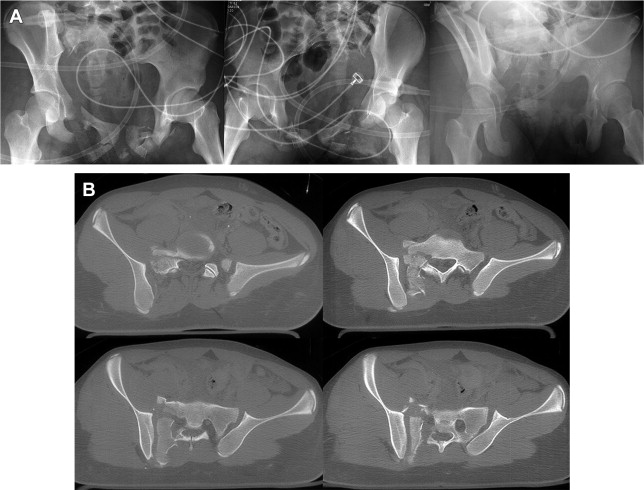
In young children, in whom much of the pelvis is not ossified, and if there is a high index of suspicion but no fracture is clearly seen on radiographs, the more advanced imaging of choice is magnetic resonance imaging (MRI), which is most sensitive at showing the degree of soft tissue disruption and displacement, including nonossified portions of the acetabulum ( Fig. 4 ).






