Hemivertebrae Excision: Posterior-Only Approach
Michael P. Glotzbecker
John B. Emans
Although a challenging operation, hemivertebra excision can result in significant deformity correction while involving only a short section of spine. Treatments available for an isolated hemivertebra include in situ fusion, convex hemiepiphysiodesis, or hemivertebra excision. In situ fusion remains the safest surgical treatment choice for an isolated hemivertebra, but to be successful, fusion must extend somewhat above and below the hemivertebra into normal spine and little or no correction is usually achieved. Convex hemiepiphysiodesis is easily accomplished and relatively safe, but the results with regard to curve correction are less predictable. Hemivertebra excision involves a short section of spine and potentially allows for complete deformity correction but remains a demanding operation with potential for neurologic complications and extensive blood loss.
The excision of an isolated hemivertebra may be performed as a staged or simultaneous anterior-posterior procedure or as a posterior-only procedure. The advantages of a simultaneous anterior-posterior approach to hemivertebra excision are complete exposure and control of the anterior operative site (1, 2). For the surgical team unfamiliar with anterior column surgery from a posterior approach, for very fragile patients where sudden blood loss entails risk, or for very lordotic deformities (or when doubt exists about manipulating the dura and its contents), simultaneous or staged anterior and posterior procedures may be preferable.
Posterior-only approaches are advantageous in that they avoid anterior surgery, allow for similar correction of the deformity, and may be performed with a low complication rate. A posterior-only approach is easiest in a kyphotic deformity, particularly in the thoracolumbar or lumbar spine. The disadvantages of posterior-only surgery include the technically demanding nature of the procedure; the potential for sudden significant blood loss, which may impair visualization and inhibit deformity correction; and the need for manipulation of the dural sac and its contents.
Ruf and Harms (3, 4) demonstrated that a posterior wedge resection with segmental pedicle screw placement could be used as a viable option for hemivertebrae resection. We and most other centers currently perform hemivertebrae resection via an all-posterior approach, and this seems to be associated with less overall morbidity and shorter hospitalization (5). When first described, it was determined that pedicle screw placement in this young population is possible and safe and has no long-term consequences with regard to canal stenosis (6, 7). However, early reports of this posterior-only technique demonstrated a high revision rate for implant failure (3, 4). Use of the three-rod technique described here has been demonstrated with a low rate of implant-related complications (5).
INDICATIONS/CONTRAINDICATIONS
Excision of a hemivertebra may be indicated when there is a hemivertebra causing progressive imbalance or curve progression in a growing child. The natural history of hemivertebra-induced curve progression is dependent on the anatomy of the congenital anomaly (8). A hemivertebra can be fully segmented with discs present above and below the abnormal vertebral body, partially segmented, or incarcerated (unsegmented). Because of the two convex growth plates present in a fully segmented hemivertebra, a fully segmented hemivertebra can progress approximately 2 degrees per year. This is compared to a partially segmented hemivertebra, which may progress by less than 1 degree per year (8). A fully incarcerated or semisegmented hemivertebra may not cause progressive deformity and may be better observed or treated differently. In general, we perform this operation from ages 3 to 8. Below age 3, the bones are often so weak that it is difficult to have sufficient anchor purchase, and above age 8, the spine and surrounding structures become stiffer and the cord seems a little less amenable to radical change without loss of signals. Observation during these years to see if there is progression and if surgery is needed or not is reasonable. Posterior element anomalies may differ from the vertebral bodies and may influence deformity behavior (9). Balanced deformities (hemimetameric shift) that result from hemivertebrae at different levels but opposite sides of the spine may not progress as the growth potential is similar on both sides of the curve. Hemivertebrae in the thoracolumbar, lumbar, and lumbosacral regions of the spine commonly cause progressive deformity above and below and are often an indication for early surgical treatment.
In general, hemivertebra resection should completely correct the patient’s local deformity in the coronal and sagittal plane. If the deformity involves a long section of the spine in a very young child, consideration should be given to growth-oriented treatments, such as a vertical expandable prosthetic titanium rib (VEPTR) or growing rods or Shilla. Patients between the ages of 3 and 5 years may be the best age for posterior-only hemivertebra excision. At this ideal age, vertebral size and strength are well enough developed to provide meaningful pedicle screw fixation and there is enough bony surface available to obtain reliable fusion. These children also represent minimal anesthetic risk. Consider earlier intervention in larger children or if the deformity is worsening rapidly or later if the child is small. The procedure can be performed on younger children, but spinal anchor fixation will be less secure and more postoperative external immobilization such as a body cast or brace will be needed. The procedure can be performed in older children easily, but the secondary deformities above and below may correct less well. Manipulation of the dura and contents is less well tolerated with advancing age, and the risk of neurologic injury may be greater above age 5 (10). Concern has been expressed about early circumferential fusion and the creation of iatrogenic canal stenosis; operating after the age of 18 months probably makes stenosis unlikely. If supplemental fixation in the form of a body cast is needed, children of this age can tolerate periods of immobilization and can still be carried fairly easily by parents.
PREOPERATIVE PLANNING
Congenital scoliosis is frequently associated with other organ system abnormalities, especially the genitourinary, auditory, musculoskeletal, and cardiac systems. A thorough examination of the patient is warranted, as is a screening ultrasound of the genitourinary system and screening echocardiogram of the cardiac system. Because more than 30% of patients with congenital scoliosis will have associated spinal dysraphism, a thorough neurologic exam is required. Other signs that may indicate the presence of a spinal dysraphism include cavus feet or presence of cutaneous manifestations over the spine such as hairy patches, dimples, or hemangiomas. A screening magnetic resonance imaging (MRI) of the spinal cord and brain stem, to assess the spinal axis, should be obtained in all of these patients (11). Major anomalies such as a coexistent diastematomyelia or major tethering may be a relative contraindication to simultaneous hemivertebra excision. Associated minor anomalies such as fatty filum with tethering are often operated on at the same anesthetic. A key part of preoperative planning is to inform the parents that there is a very significant chance that even if the hemiverte-brectomy is 100% successful in correcting the scoliosis at the time of surgery, a more global scoliosis may gradually develop over time that may require a much longer spinal fusion years in the future.
Upright preoperative posteroanterior (PA) and lateral x-rays of the spine help assess balance, while preoperative bending, supine, or push-prone radiographs assess the anatomy and flexibility of the adjacent curvatures. A computed tomography (CT) scan of the spine with three-dimensional reconstructions is indispensable in preoperative assessment and surgical planning (9). Plain radiographs often do not reveal posterior laminar fusions or bifid lamina that may be present at surgery and that can cause confusion when trying to identify levels in the operating room (Fig. 40-1). Pedicles immediately above and below the hemivertebra should be identified on the CT. Posterior-only excision assumes adequate pedicles in the body above and below the hemivertebra. If pedicles
are not present (not a rare circumstance in congenital anomalies), hemiexcision as described here will not be feasible, and some other option such as laminar hooks, rib hooks, and postoperative cast fixation or temporary implants above or below the vertebrae to be fused can be considered. We have been happy with the three-rod technique in which the initial correction is obtained via laminar hooks and a third rod, which requires adequate hemilaminae above and below (5).
are not present (not a rare circumstance in congenital anomalies), hemiexcision as described here will not be feasible, and some other option such as laminar hooks, rib hooks, and postoperative cast fixation or temporary implants above or below the vertebrae to be fused can be considered. We have been happy with the three-rod technique in which the initial correction is obtained via laminar hooks and a third rod, which requires adequate hemilaminae above and below (5).
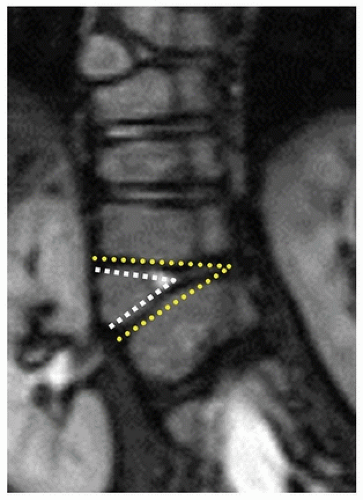
Preoperative planning most often includes the goal of complete correction of the deformity at that level, which may best be thought of as a wedge resection in the coronal plane (Fig. 40-2). If the deformity is kyphotic, more posterior column must be resected; if lordotic, more anterior column will need to be resected. The hemivertebra body must be resected, but equally important, any disc
and endplate cartilage above and below must also be resected back to the endplate. The resection optimally continues well past the midline over to the concave annulus, but leaving the concave annulus intact as a stabilizing hinge. Without such a resection across midline, complete correction in the coronal plane will be quite difficult and inadvertent lordosis may be produced. Excising the bony vertebral body in children is relatively easy, but resecting the rubbery, resistant endplate and disc material is much more difficult.
and endplate cartilage above and below must also be resected back to the endplate. The resection optimally continues well past the midline over to the concave annulus, but leaving the concave annulus intact as a stabilizing hinge. Without such a resection across midline, complete correction in the coronal plane will be quite difficult and inadvertent lordosis may be produced. Excising the bony vertebral body in children is relatively easy, but resecting the rubbery, resistant endplate and disc material is much more difficult.
The surgical team should be conversant with surgery on the anterior column, placement of pedicle screws and laminar hooks in small children, and control of epidural and vertebral body bleeding. A second set of experienced hands can be critical if epidural bleeding is difficult to control or visualization is difficult due to rapid bleeding from the vertebral body. The anesthetic team should be comfortable with anesthetic technique for intraoperative neurologic monitoring, and although patients only rarely require transfusion, there can be sudden massive bleeding from the vertebral body or sustained heavy bleeding from epidurals, and the anesthetic team should be appropriately prepared with a large-bore peripheral IV in order to adequately resuscitate the patient or administer a transfusion if necessary.
SURGICAL PROCEDURE
Appropriate anesthesia, arterial monitoring, Foley catheter placement, and motor-evoked potential (MEP) and somatosensory-evoked potential (SSEP) monitoring can be performed prior to or after surgical positioning depending on surgeon preference and risk assessment. The patient is positioned prone on a radiolucent table. Support is placed under the chest and the pelvis, leaving the abdomen free. If size permits, this can be done with a specialized table with pads specific for the prone positioning. However, in smaller children, a combination of rolled blankets or gel rolls under the chest and pelvis will provide adequate support while leaving the abdomen free. Airplaning the table slightly with the convex side up may improve visibility when resecting the anterior portion of the vertebral body and retracting the dura (Fig. 40-3). A headlight assists in this portion of the procedure. A radiopaque marker can be placed over the skin and examined with fluoroscopy prior to incision, to ensure that the incision is made at the appropriate level.
Exposure should not enter the facet joints above or below the intended segments of fusion. Inadvertent subperiosteal exposure of adjacent vertebrae or facets will likely result in inadvertent fusion above or below, negating some of the benefit of a localized hemivertebra excision. One may perform a standard midline incision or an incision a couple of centimeters lateral to midline over the pedicle of the hemivertebrae, while planning for the possibility of a longer fusion in
the future. Subperiosteal dissection is carried out over the vertebrae of intended instrumentation and fusion, leaving the interspinous ligaments and facet joints above and below these vertebrae intact. Awareness of any laminar defects or widely bifid areas helps avoid inadvertent dural injury (Fig. 40-1



the future. Subperiosteal dissection is carried out over the vertebrae of intended instrumentation and fusion, leaving the interspinous ligaments and facet joints above and below these vertebrae intact. Awareness of any laminar defects or widely bifid areas helps avoid inadvertent dural injury (Fig. 40-1
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree