Hemiarthroplasty for Management of Complex Proximal Humerus Fractures: Preoperative Planning and Surgical Solution
Ariane Gerber
Jon J. P. Warner
A. Gerber: Department for Orthopaedic Surgery, Department for Trauma and Reconstructive Surgery, Medical School-Charité, Berlin, Germany.
J. J. P. Warner: Partner’s Department of Orthopaedic Surgery, Massachusetts General and Brigham and Women’s Hospitals, Harvard Medical School, Boston, Massachusetts.
INTRODUCTION: THE PROBLEM
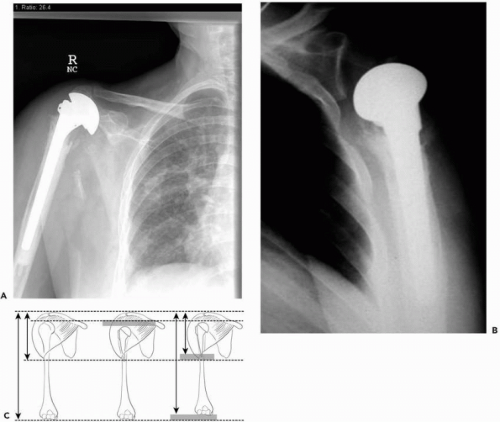
Proximal humerus fractures that require surgical treatment account for only 20% of fractures in this region because most are satisfactorily managed with nonoperative methods. A small percentage of the fractures involve severe comminution or occur in the setting of poor quality bone, which precludes stable fixation and thus requires endoprosthetic treatment. These cases can be very technically challenging, owing to loss of available anatomic landmarks. Indeed, many poor outcomes can be directly attributed to surgical errors in placement of the prosthesis. Typically, the humeral head placed is either too large or too small, and the prosthetic height is either too short or too long. Excessive retroversion is not uncommon as a factor seen in failed treatments1, 2, 3 and 4,6,7 (Fig. 15-1).
In these cases, there is loss of anatomic reference points due to distortion of the proximal humeral anatomy. Together, with the anatomic fact that there is a wide range of proximal humeral anatomy, it is not surprising that placement of a humeral component in a manner which restores normal articular position may be a difficult feat.5,14,19 Factors to consider include variable humeral head diameter, neck-shaft inclination, retroversion, and offset of the humeral head center relative to the shaft axis. Thus, the goal
of reconstruction is to restore the anatomic relationships between the humeral head component and the tuberosities. This should affect forces across the joint, which will allow not only for tuberosity healing and proper soft-tissue tensioning, but also for less wear and tear on the glenoid. Indeed, misplacement of the humeral component has been associated with accelerated glenoid wear.18
of reconstruction is to restore the anatomic relationships between the humeral head component and the tuberosities. This should affect forces across the joint, which will allow not only for tuberosity healing and proper soft-tissue tensioning, but also for less wear and tear on the glenoid. Indeed, misplacement of the humeral component has been associated with accelerated glenoid wear.18
Another critical technical problem is secure tuberosity fixation and healing, and loss of tuberosity fixation and poor function are, unfortunately, not uncommon (Fig. 15-2).
Other factors that can contribute to a poor outcome include advanced patient age and poor bone quality, patient comorbid factors, such as poor general health, poor social supports for postoperative care, and supervised therapy program.
Even in the best surgical hands the expected clinical outcome is largely limited to pain relief but not restoration of function. Although Neer16 reported reliable restoration of shoulder motion, the best contemporary studies13,20,21 show that less than 50% of patients can expect to be able to raise their arms over their heads after hemiarthroplasty for acute fracture. Indeed, recent studies11,12,20,21 have demonstrated that surgeon experience and hospital volume closely correlate to expected outcome, with lower volume centers having a poorer outcome and higher complication rate. It therefore would seem that many of the variables affecting patient outcome after this surgery are directly controlled by the surgeon.
The purpose of this chapter is to review our current approach to preoperative patient selection, planning, surgical
technique, and postoperative care for a successful outcome using hemiarthroplasty to manage acute proximal humerus fractures that cannot be surgically reconstructed by fixation methods. Few publications consider all steps critically important, and most usually concentrate on the surgical techniques. We believe that patient selection followed by accurate preoperative planning prepares the surgeon to achieve a predictable and consistently good outcome.
technique, and postoperative care for a successful outcome using hemiarthroplasty to manage acute proximal humerus fractures that cannot be surgically reconstructed by fixation methods. Few publications consider all steps critically important, and most usually concentrate on the surgical techniques. We believe that patient selection followed by accurate preoperative planning prepares the surgeon to achieve a predictable and consistently good outcome.
Indications for Hemiarthroplasty
Patient Selection
In many cases of complex proximal humerus fracture osteosynthesis, either by closed means or through formal open reduction, internal fixation may be the best choice, especially in young patients with good quality bone. The goal is to maintain anatomic relationships between the humeral head and tuberosities. Even in the case of avascular necrosis, the prognosis may remain quite good, and subsequent arthroplasty reconstruction, if necessary, can be more easily performed than if a malunion were the problem.9 Our indications for immediate hemiarthroplasty for proximal humeral fracture include severe comminution of the articular segment, impression fracture greater than 40% of the articular surface, four-part fracture in an older individual, two- or three-part fracture with poor bone quality in some older individuals.10,16
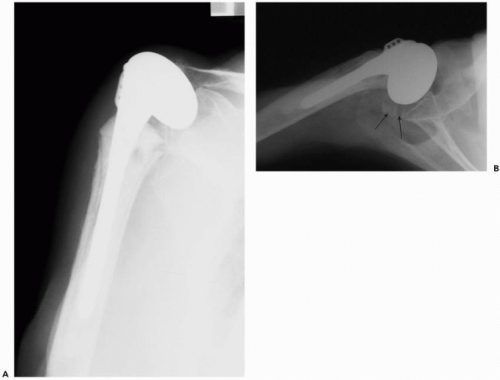 Figure 15-2 (A) AP view demonstrates no observable greater tuberosity. (B) Axillary x-ray shows remnant of greater tuberosity in a posterior displaced position (arrows). |
Prior to performing surgery, it is very important to establish that the patient has good social support for postoperative recovery and understands the immediate postoperative commitment to physical therapy following surgery.
Preoperative Planning: Anatomical Basis
Patient Assessment
First, a thorough preoperative history and clinical examination should be performed to evaluate the patient’s overall
health status and identify any medical comorbidities. Their ability to perform a strict postoperative rehabilitation program should also be assessed. Furthermore, associated injuries, like neurovascular injuries of the injured arm, should be documented prior to surgery.
health status and identify any medical comorbidities. Their ability to perform a strict postoperative rehabilitation program should also be assessed. Furthermore, associated injuries, like neurovascular injuries of the injured arm, should be documented prior to surgery.
Radiographic Assessment
Conventional radiographic evaluation with orthogonal views must include an anteroposterior radiograph and axillary radiograph. This is essential to accurately classify the fracture configuration and document humeral head and tuberosity positions. The anteroposterior view gives information about the amount of displacement of the greater tuberosity and the extent of metaphyseal comminution of the fracture. The axillary view is essential to evaluate the presence of an associated glenohumeral dislocation and to appreciate the amount of displacement of the lesser tuberosity. In selected cases, a CT scan may add information about fragment displacement and associate injury to the glenoid.
Little is written about preoperative planning for surgical reconstruction with hemiarthroplasty. Although many arthroplasty designs are available and some utilize a variety of jigs for placement, the emphasis of many techniques is based on intraoperative decision making and visual approximation of anatomy. We believe that this is one reason why many surgical results reflect nonanatomic reconstruction, which may be the inevitable cause of failure of the procedure.
The objectives of prosthetic replacement of the humeral head for fractures are to determine the proper size and position of the prosthetic head, despite loss of anatomic references, and to perform a stable osteosynthesis of the tuberosities. Indeed, accurate placement of the prosthesis in terms of reestablishing proper head height, retroversion, and tuberosity offset strongly correlates with tuberosity healing and ultimate functional outcome.1,2,13
Anatomic studies have shown that there is a large variability of proximal humeral anatomy among individuals and between both shoulders in the same individuals.1, 2 and 3 The data obtained in those cadaveric studies create the basis for design of most modern third-generation implants. However, in the setting of a complex proximal humerus fracture, arthroplasty reconstruction is based on mean values of inclination, retroversion, medial, and lateral offsets and is therefore always an approximation of normal individual anatomy. Whereas head size and head height can reliably be determined with preoperative planning, definition of retroversion remains an unsolved problem.14 Most authors recommend a hemiarthroplasty implant for the fracture at a mean retroversion of 20 degrees to 30 degrees. Considering that individual retroversion can range from 10 degrees to 60 degrees, an error in rotation can theoretically be up to 30 degrees to 40 degrees.5, 6 and 7 This is of great importance, because malrotation of the implant seems to be a significant factor for early failure of fixation of the tuberosities.6,7
If arthroplasty is indicated, we always obtain bilateral long arm radiographs in the anteroposterior plane so that the humeral length can be determined. A magnification marker is utilized so that comparison views of the contralateral shoulder can act as an accurate reference for length. The size of the contralateral humeral head can be templated to determine the proper size of the humeral head. This will ensure that proper tuberosity offset can be obtained because the humeral head size is accurate. The proper length of the prosthesis is determined by measuring the length of the contralateral normal side and then subtracting the length of the fractured humerus. This will give the length required to place the humeral component at the proper height (Figs. 15-3 and 15-4): The distance a (distance between the proximal end of the shaft and the top of the prosthesis) determined in the drawing can then be measured
intraoperatively (Fig. 15-5) and is required for reconstruction of humeral length h (Fig. 15-6). In addition, the surgeon can anticipate if bone loss will require an associated bone graft to restore tuberosities to the proper position. Allograft can then be available or the patient’s iliac crest can be sterilely prepared, if necessary. This method has been used by Boileau et al., though they utilized an intraoperative jig for the reconstruction and demonstrated an accuracy to within 1 cm of the contralateral side.3
intraoperatively (Fig. 15-5) and is required for reconstruction of humeral length h (Fig. 15-6). In addition, the surgeon can anticipate if bone loss will require an associated bone graft to restore tuberosities to the proper position. Allograft can then be available or the patient’s iliac crest can be sterilely prepared, if necessary. This method has been used by Boileau et al., though they utilized an intraoperative jig for the reconstruction and demonstrated an accuracy to within 1 cm of the contralateral side.3
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree