Fig. 1.1

Fig. 1.2
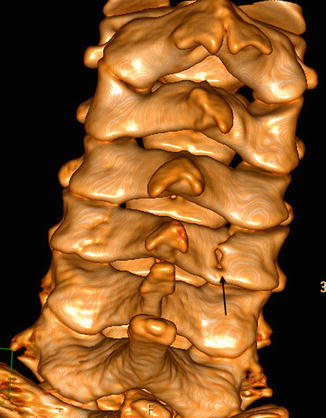
Fig. 1.3

Fig. 1.4
A 16-year-old male sustains an impact with a hyperflexion cervical injury while performing a somersault during a physical education class. He presents with severe pain and power loss in both lower extremities. The paraplegia is obvious in the emergency room: muscle weakness, loss of sensation, deep tendon hyperreflexia, and autonomic function alteration, all compatible with a spinal cord lesion.
Comments
In young children, due to their biomechanical setup leading to greater flexibility (skeletal immaturity plus increased laxity in paravertebral ligaments and muscles), cervical trauma tends to occur at higher levels, from the base of the cranium to C3. The greater spine flexibility relative to the cord explains the tendency for cord damage without bony lesions. In older children and teenagers, cord injuries are more frequently seen at C5–C6 level, just like in adults.
Specific facts to be considered in pediatric cervical trauma:
C2–C3 subluxation is physiological.
The atlantoaxoid distance is greater than in adults.
Odontoid fractures tend to affect the basal synchondrosis.
In a pediatric sporting activity context, cervical spine fractures with associated cord damage are typical in diving during water sports, to the point of, according to some series, being the most frequent cause for cord injury in this age group. Diving into shallow waters is particularly dangerous. In gymnastics, the mechanism of injury tends to be extreme hyperflexion with or without associated trauma.
Cervical spine radiographs, including lateral views up to C7/T1, are usually the initial diagnostic tool. However, the false negative rate with a single lateral study can reach between 21 and 26 %, so taking the clinical findings into consideration; CT should be considered to complete the exam.
CT with multiplane reformatting plays a fundamental role in cervical trauma diagnosis: it adequately shows fracture trajectories and extension in a better way than MRI.
MRI is useful in spinal cord evaluation, detecting cord lesion (with or without associated bony fracture) and possible cord compression. It is also valuable to assess the extradural space and spinal ligaments.
Radiological Findings
The plain lateral view (Fig.1.1) shows a vertebral body fracture in C5 (arrow). Given the clinical and radiological findings and the incomplete study (no views of the lower spine), a CT was performed.
A cervicothoracic CT with multiplanar reformatting in the sagittal plane (Fig. 1.2) shows C5 with an anteroposterior fracture line in the upper cortex following a right inferolateral trajectory in the anterior region of the lower cortex. The fracture line reaches the posterior wall.
The volumetric 3D reconstruction (Fig. 1.3), posterior view, shows fracture lines in both C5 laminae, with greater displacement on the right (arrow) but without interapophyseal joint disruption.
The MRI study (sagittal plane, STIR) (Fig. 1.4) shows an increased cord signal from C4 to C6 consistent with contusion. There are signal changes in C5 and C6 vertebral bodies compatible with bony edema. There is extensive soft tissue signal alteration consistent with acute posttraumatic edema.
Case 1.2: Lumbar Spondylolysis

Fig. 1.5
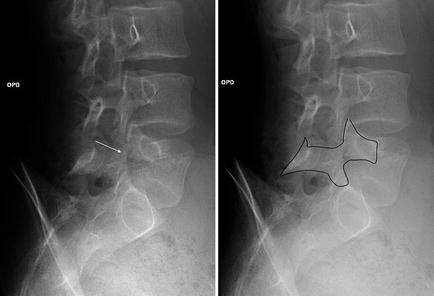
Fig. 1.6
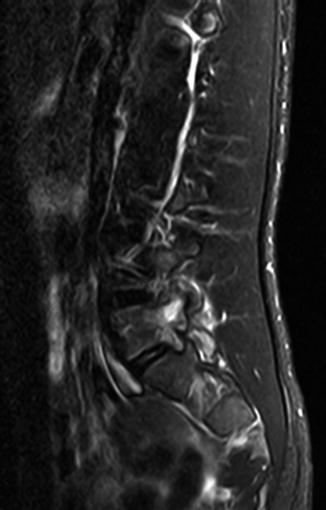
Fig. 1.7
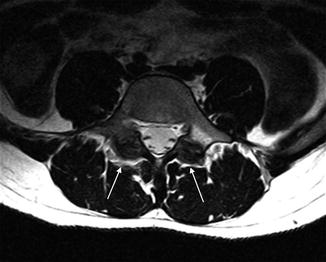
Fig. 1.8
A 15-year-old male presented with lumbar pain for the previous 2 months, partially resolved with nonsteroidal anti-inflammatory drugs. He was a keen skate-park boarder and referred multiple trauma events although he did not recall any of them as precipitant to the presenting complaint.
Comments
Spondylolysis is fairly frequent in sporting children and teenagers. It occurs in almost half the cases consulting for lumbar pain. It can happen both with repetitive and acute trauma, mostly when subjected to flexion and hyperextension forces. It is typical in soccer players, gymnasts, swimmers, and pool divers.
It originates on a pars articularis defect on the vertebral posterior elements.
Although it can affect any level, it tends to involve L5 85–95 % of the times (the rest is mostly L4). It can be uni- or bilateral. When unilateral, a compensatory contralateral sclerosis can be seen; it should not be mistaken for other pathologies such as osteoid osteoma.
Plain lumbar spine radiographs in four views (anteroposterior, lateral, and both obliques) are required. Oblique views are needed since up to 20 % of cases are only seen in them. Interruption of LaChapelle’s or Scotty dog’s neck is the classical sign. A lateral radiograph may show an associated spondylolisthesis.
Given the high incidence in young sportswomen and men, if the plain radiographs are normal but the suspicion index is high, other diagnostic tools (bone scan, CT, or MRI) that could additionally detect other pathologies such as infection or osteoid sarcoma should be used.
MRI is able to determine early edema before a complete defect occurs (allowing a better response to conservative treatment). The lack of ionizing radiation for MRI makes the technique of choice to evaluate spondylolysis.
Case 1.3: Isolated Spinous Process Fracture

Fig. 1.9
Fig. 1.10
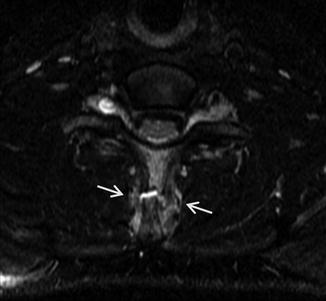
Fig. 1.11

Fig. 1.12
A 16-year-old soccer player got injured after forcibly hyperextending his neck trying to head the ball towards another player. He presented with pain and decreased range of cervical flexion–extension. There was pain on palpation of the lower cervical spinous processes.
Comment
Isolated spinous process fractures (Clay-shoveler fracture) are fairly infrequent, and they are generally considered stable. However, they can also be associated to more significant lesions depending on the forces involved.
They were first described in Western Australia among strenuous physical laborers. They have been reported in American football, volleyball, power lifting, golf, cycling, diving, skiing, ice hockey, wrestling, and gymnastics and, anecdotally, among Nintendo Wii players and indoor rock climbers.
They usually occur at lower cervical/ upper thoracic levels. Mechanisms of injury include hyperflexion, hyperextension, rotation, or repetitive stress. In these cases the para- and supraspinous musculature and ligaments can avulse the spinous process. When caused by a direct blow, they may be associated to other more serious injuries or extend into the laminar regions. In high-risk incidents, exquisite care should be taken to rule out unstable injuries capable of spinal cord or nerve root damage.
Plain radiography (AP, lateral, and odontoid views) constitutes the initial investigation of choice. A ghost sign, where a double spinous process is seen on the AP view, results from displacement of the fracture.
Patients with associated injuries or presenting after a high-risk mechanism of injury or those showing radiological abnormalities on initial studies require CT investigation with coronal and sagittal reformatted views.
MRI is useful in investigating suspected muscular, ligamentous, and spinal cord injuries. CT and/or MR angiogram are required to discard vascular injuries.
Isolated spinous process fractures are almost always managed conservatively with rest, analgesia, and immobilization during the painful period followed in due course by physical therapy. They may become chronically symptomatic in particular if nonunion is present.
Our player’s management included soft collar immobilization for 10 days. Jogging was introduced on day 15 post injury and more complex football drills on his own at day 40. He was discharged back to full training at day 72.
Radiological Findings
The axial (Fig. 1.9) and sagittal reconstruction CT (Fig. 1.10) show the C7 spinous process fracture.
The axial fat-suppressed FSE T2-weighted MR image (Fig. 1.11) shows the fracture and surrounding edema (arrows).
The sagittal fat-suppressed FSE T2-weighted MR image (Fig. 1.12) shows the fracture with no other acute injury related.
Case 1.4: Cranial Fracture with Intraparenchymal Contusion/Hematoma
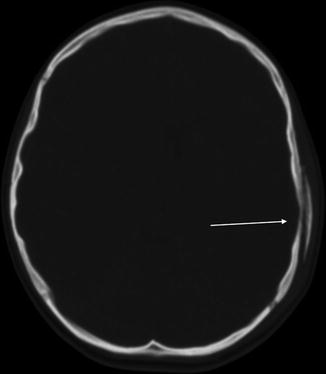
Fig. 1.13
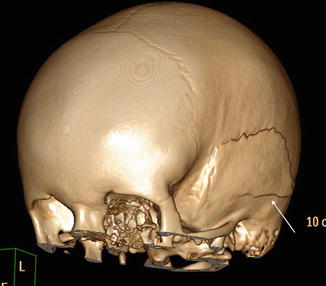
Fig. 1.14

Fig. 1.15
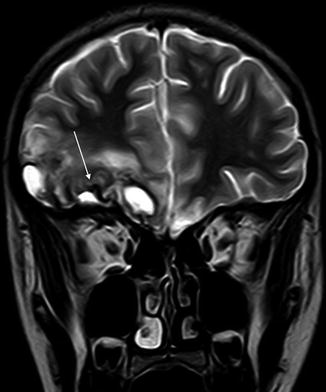
Fig. 1.16
A 13-year-old male suffered a head injury after a cycling accident. He was brought to the emergency room with temporary loss of consciousness and severe headache. On examination, there was an obvious cranial nerve VI lesion on the right side.
Comment
Cycling accidents are the most common cause of head injury in older children and teenagers. While most of them are mild, detecting intracranial lesions requiring extended management is paramount. The choice of diagnostic imaging techniques is dictated by clinical findings and evaluation including a Glasgow Coma Scale.
Contrary to adults, in smaller children, due to the head’s larger relative volume and the skull’s increased flexibility and fragility, a lower energy impact can lead to skull fractures. Plain radiography can detect most of them (seen as radiolucent linear images). A fracture increases the chances of intracranial lesions, but its absence does not exclude significant parenchymal damage, so plain radiography is not useful as a screening tool. Over 50 % cases combine intracranial lesions with normal plain radiographs, and about half detected skull fractures are associated to intraparenchymal injury.
CT’s speed and ability to detect acute traumatic lesions make it the investigation of choice to diagnose and follow up pediatric head injuries. If the fracture is parallel to axial cuts, multiplane 3D reconstructions or MIP (Maximum Intensity Projection) may be required.
Intra-axial lesions are mostly constituted by contusions, intraparenchymal hematomas, and shearing lesions.
In children, the greater cranial flexibility increases the risk for intraparenchymal damage. This can be caused by either direct trauma or secondary to acceleration–deceleration mechanisms. Their main locations are as follows: temporal lobe (temporal pole, inferior temporal region and adjacent to the Sylvian fisure), frontal lobe, frontal lobe (inferior frontal region), and parasagittal areas.
Contusions are seen in CT as poorly defined, low-density areas. Hyperdense foci can be noted in superficial gray matter if hemorrhage is present.
MRI has a greater sensitivity in detecting nonhemorrhagic contusions: FLAIR sequence on MRI shows cortical edema, while T2 echo-gradient sequence detects chronic hemorrhage and hemosiderin deposits.
Radiological Findings
Helicoidal CT without contrast shows a left temporal fracture (arrow) with overlapping on the bony window (Fig. 1.13). A volumetric 3D reconstruction is performed to better appreciate the whole fracture (arrow) (Fig. 1.14). The parenchymal window (Fig. 1.15) shows hemorrhagic contusions (highly attenuated foci) in right basal frontal (arrow) and anterior temporal regions with perilesional vasogenic edema.
MRI: a cortex/subcortex fuzzy lesion, mostly hyperintense, with decreased signal in relation to hemosiderin (arrow) in the right anterior frontal and temporal regions compatible with evolving trauma is noted on the T2-weighted coronal plane (Fig. 1.16).
Case 1.5: Cranial Fracture with Epidural Hematoma

Fig. 1.17
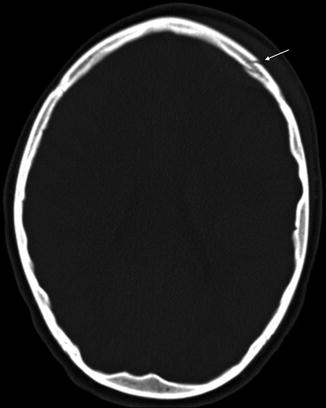
Fig. 1.18
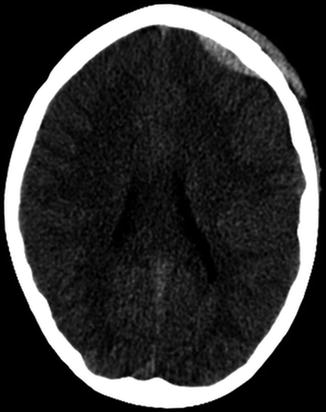
Fig. 1.19
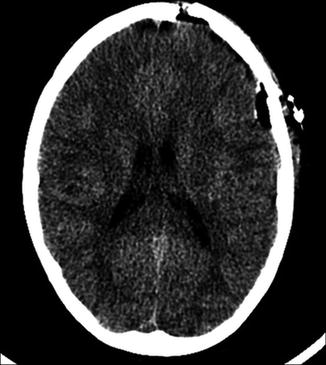
Fig. 1.20
A 9-year-old boy suffered a frontal head trauma following a goal frame falling on him. After a lucid interval he presented with headache and deteriorating conscious level.
Comments
Head trauma during soccer practice is more common among the 10–14 age group. The main mechanism of injury tends to involve a direct collision with another player, specifically, head to head. In the 5–9-year-old age group, there is a high proportion of head trauma caused by goal post-impact.
In addition to intraparenchymal damage, cranial trauma can be associated to extra-axial blood collection, both epidural and/or subdural.
A posttraumatic epidural hematoma is a blood collection between the dura mater and the internal skull table. It is most usually located in the temporoparietal region. It occurs in 1–3 % of moderate to severe head trauma in children.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








