1 Hand and Wrist Injuries
Flexor Tendon Injuries
Important points for rehabilitation after flexor tendon laceration and repair
Rehabilitation rationale and basic principles of treatment after flexor tendon repair
Timing
Before tendons can be secondarily repaired, these requirements must be met:
Table 1-1 Boyes’ Preoperative Classification
| Grade | Preoperative Condition |
|---|---|
| 1 | Good: minimal scar with mobile joints and no trophic changes |
| 2 | Cicatrix: heavy skin scarring from injury or previous surgery; deep scarring from failed primary repair or infection |
| 3 | Joint damage: injury to the joint with restricted range of motion |
| 4 | Nerve damage: injury to the digital nerves resulting in trophic changes in the finger |
| 5 | Multiple damage: involvement of multiple fingers with a combination of the above problems |
Anatomy
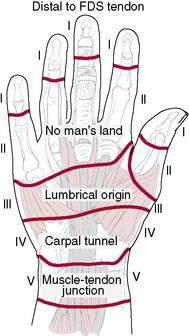
The anatomic zone of injury of the flexor tendons influences the outcome and rehabilitation of these injuries. The hand is divided into five distinct flexor zones (Fig. 1-3):
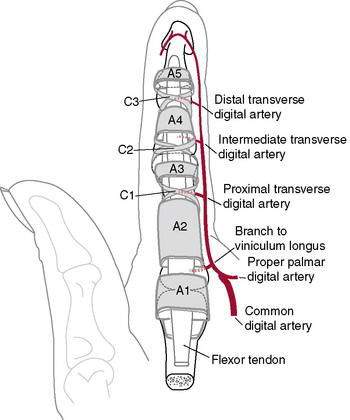
It is essential that the A2 and A4 pulleys (Fig. 1-4) be preserved to prevent bowstringing. In the thumb, the A1 and oblique pulleys are the most important. The thumb lacks vincula for blood supply.
Tendon Healing
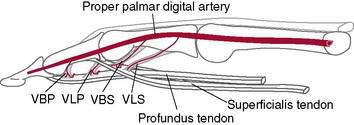
Flexor tendons in the distal sheath have a dual source of nutrition via the vincular system and synovial diffusion. Diffusion appears to be more important than perfusion in the digital sheath (Green 1993).
Several factors have been reported to affect tendon healing:
Through experimental and clinical observation, Duran and Houser (1975) determined that tendon glide of 3 to 5 mm is sufficient to prevent motion-limiting tendon adhesions. Exercises are thus designed to achieve this motion.
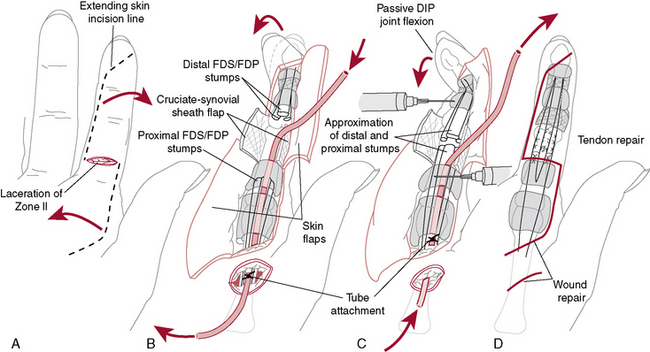
Treatment of Flexor Tendon Lacerations
Teno-Fix Repair
A stainless-steel tendon repair device (Teno Fix, Ortheon Medical, Columbus, OH) was reported to result in lower flexor tendon rupture rates after repair and similar functional outcomes when compared with conventional repair in a randomized, multicenter study, particularly in patients who were noncompliant with the rehabilitation protocol (Su et al. 2005, 2006). Active flexion was allowed at 4 weeks postoperatively. Solomon et al. (unpublished research) developed an “accelerated active” rehabilitation program to be used after Teno Fix repairs: Active digital flexion and extension maximum-attainable to the palm are started on the first day with the goal of full flexion at 2 weeks postoperatively. The anticipated risks with this protocol are forced passive extension, especially of the wrist and finger (e.g., fall on outstretched hand), and resisted flexion, potentially causing gapping or rupture of the repair.
FDP lacerations can be repaired directly or advanced and reinserted into the distal phalanx with a pull-out wire, but they should not be advanced more than 1 cm to avoid the quadregia effect (a complication of a single digit with limited motion causing limitation of excursion and, thus, the motion of the uninvolved digits). Citing complications in 15 of 23 patients with pull-out wire (button-over-nail) repairs, 10 of which were directly related to the technique, Kang et al. (2008) questioned its continued use. Complications of the pull-out wire technique included nail deformities, fixed flexion deformities of the distal interphalangeal (DIP) joint, infection, and prolonged hypersensitivity.
A more recent technique for FDP lacerations is the use of braided polyester/monofilament polyethylene composite (FiberWire, Arthrex, Naples, FL) and suture anchors rather than pull-out wires (Matsuzaki et al. 2008, McCallister et al. 2006). Reports of outcomes currently are too few to determine if this technique will allow earlier active motion than standard techniques.
Rehabilitation after flexor tendon repair
The rehabilitation protocol chosen (Rehabilitation Protocols 1-1 and 1-2) depends on the timing of the repair (delayed primary or secondary), the location of the injury (zones 1 through 5), and the compliance of the patient (early mobilization for patients who are compliant and delayed mobilization for patients who are noncompliant and children younger than 7 years of age). A survey of 80 patients with flexor and extensor tendon repairs determined that two thirds were nonadherent to their splinting regimen, removing their splints for bathing and dressing (Sandford et al. 2008).
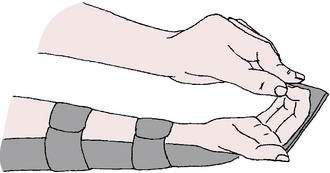
REHABILITATION PROTOCOL 1-1 Rehabilitation Protocol after Immediate or Delayed Primary Repair of Flexor Tendon Injury: Modified Duran Protocol
Postoperative Day 1 to Week 4.5
Passive flexion and extension exercises of the proximal interphalangeal (PIP) joint in a dorsal blocking splint (DBS).
4.5 Weeks
REHABILITATION PROTOCOL 1-2 Indianapolis Protocol (“Active Hold Program”)
(From Neumeister M, Wilhelmi BJ, Bueno Jr, RA: Flexor tendon lacerations: Treatment. http://emedicine.medscape.com/orthopedic_surgery)
In a comparison of early active mobilization and standard Kleinert splintage,Yen et al. (2008)found at an average 4-month follow-up (3 to 7 months) that those in the early active mobilization group had 90% of normal grip strength, pinch, and range of motion compared to 50%, 40%, and 40%, respectively, in those with Kleinert splinting.
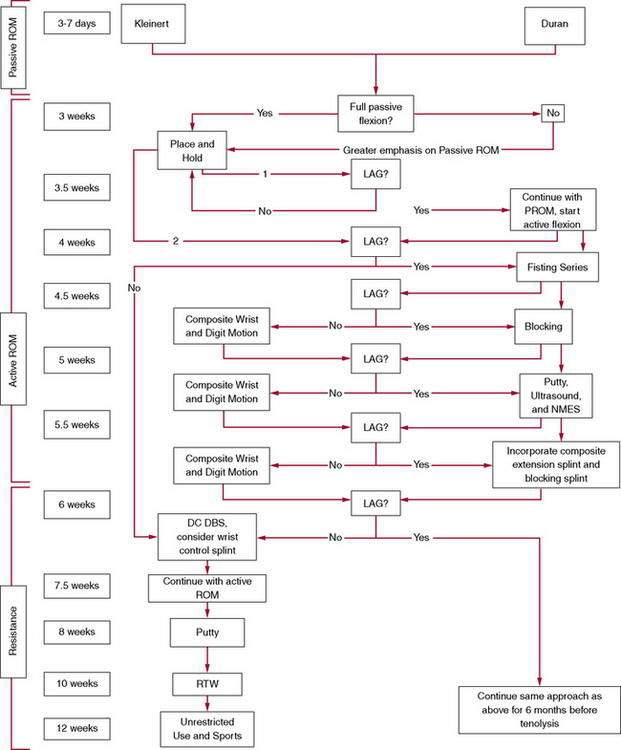
Sueoka and LaStayo (2008) devised an algorithm for zone 2 flexor tendon rehabilitation that uses a single clinical sign—the lag sign—to determine the progression of therapy and the need to modify existing protocols for individual patients. They defined “lag” as PROM—AROM (active ROM) ≥15 degrees and consider it a sign of tendon adherence and impairment of gliding. Rehabilitation begins with an established passive ROM Protocol (Duran), which is followed for 3.5 weeks before the presence or absence of a lag is evaluated. The presence or absence of lag is then evaluated at the patient’s weekly or twice-weekly visits, and progression of therapy is modified if a lag sign is present (Rehabilitation Protocol 1-3).
Trigger Finger (Stenosing Flexor Tenosynovitis)
S. Brent Brotzman, MD, and Theresa M. Kidd, BA
Treatment
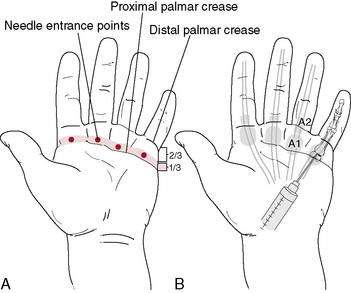
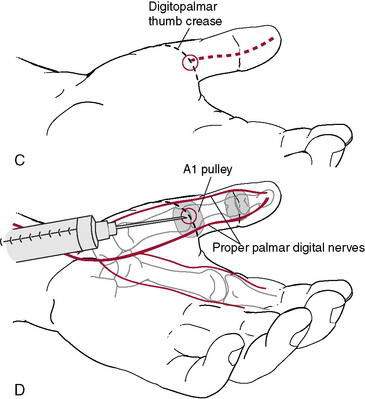
Currently, nonoperative treatment involves injection of corticosteroids with local anesthetic into the flexor sheath. A meta-analysis of the literature found convincing evidence that combining lidocaine with the corticosteroid obtains results superior to those with corticosteroid alone(Chambers 2009). In a cost-minimization analysis, the use of two steroid injections before resorting to surgery was found to be the least costly treatment strategy compared to one or three injections before surgery and open or percutaneous release(Kerrigan and Stanwix 2009).
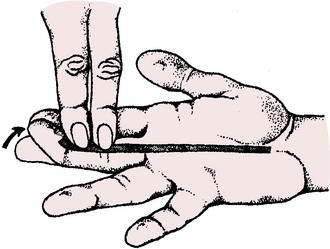
Our preference is 0.5 ml lidocaine, 0.5 ml bupivicaine, and 0.5 ml methylprednisolone acetate (Depo-Medrol) (Fig. 1-5). A single injection can be expected to relieve triggering in about 66% of patients. Multiple injections have been reported to relieve triggering in 75% to 85% of patients. Current reports indicate a success rate of 47% to 87% with this type of treatment. Systematic review of levels I and II studies in the Journal of the American Academy of Orthopedic Surgeons (Fleisch et al. 2007) indicates a success rate of 57%. Prognostic indicators of recurrence of trigger digits after corticosteroid injection include younger age, insulin-dependent diabetes mellitus, involvement of multiple digits, and a history of other tendinopathies of the upper extremity (Rozental et al. 2008).
The risk of cortisone injection here is of inadvertent injection into the flexor tendon with possible tendon weakening or rupture. Ultrasound guidance has been reported to help avoid this complication and improve results (Bodor and Flossman 2009).
Surgery to “release” a trigger finger is a relatively simple outpatient procedure done with the patient under local anesthesia. The surgery involves a 1- to 2-cm incision in the palm overlying the A1 pulley to identify and completely divide the A1 pulley. Gentle active motion is initiated early, and return to unrestricted activities usually is possible at about 3 weeks (Rehabilitation Protocol 1-4).
REHABILITATION PROTOCOL 1-4 Rehabilitation Protocol After Trigger Finger Cortisone Injection or Release
After Trigger Release Surgery
| 0–4 days | Gentle active MCP/PIP/DIP joint ROM (avoid gapping of wound). |
| 4 days | Remove bulky dressing and cover wound with bandage. |
| 4–8 days | Continue ROM exercises. Remove sutures at 7–9 days. |
| 8 days–3 weeks | Active/active-assisted ROM/PROM MCP/PIP/DIP joints. |
| 3 weeks + | Aggressive ROM and strengthening. Return to unrestricted activities. |
Pediatric trigger thumb
Pediatric trigger thumb is a congenital condition in which stenosis of the A1 pulley of the thumb in infants causes locking in flexion (inability to extend) of the IP joint. It often is bilateral. Usually no pain or clicking occurs because the thumb remains locked. A recent report by Baek et al. (2008) indicates spontaneous resolution in 63% of cases. The rest require surgical intervention when the patient is around 2 to 3 years old to release the tight A1 pulley and prevent permanent joint flexion contracture.
Flexor Digitorum Profundus Avulsion (“Jersey Finger”)
Background
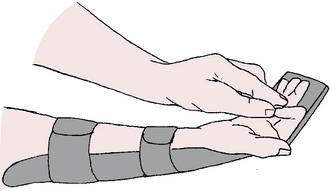
The resultant lack of active flexion of the DIP joint (FDP function loss) must be specifically checked to make the diagnosis (Fig. 1-6). Often the swollen finger assumes a position of extension relative to the other, more flexed fingers. The level of retraction of the FDP tendon back into the palm generally denotes the force of the avulsion.
Leddy and Packer (1977) described three types of FDP avulsions based on where the avulsed tendon retracts: type I, retraction of the FDP to the palm; type II, retraction to the proximal interphalangeal (PIP) joint; and type III, bony fragment distal to the A4 pulley. Subsequently, a type IV injury was described in which a type III lesion is associated with a simultaneous avulsion of the FDP from the fracture fragment. Treatment is based on the anatomy of the injury.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree