Fig. 3.1
(a) AP X-ray. (b) Lateral X-ray. Preoperative X-rays of typical Valenti candidate
3.3 Author’s Preferred Technique: The Valenti Arthroplasty
A linear incision is made approximately 5 cm over the first metatarsophalangeal joint (Fig. 3.2). It is deepened and great care is taken to dissect the capsule off the proximal phalanx first in the medial aspect. Next was coming up in the “student” hole and dissecting the capsule off the medial aspect of the first metatarsal (Fig. 3.3). Then, the periosteum is gently removed underneath the extensor hallucis longus tendon along with capsule to expose the entire head of the joint and base of the proximal phalanx (Fig. 3.4).



Fig. 3.2
Incisional approach

Fig. 3.3
Dissection medially through “student hole”
Fig. 3.4
(a) Medial view. (b) Dorsal view. Dissection exposes the entire dorsal first
Great care is taken not to resect the flexor hallucis brevis tendon plantarly nor the extensor hallucis longus dorsally. Next, our attention is focused on the degenerative bone around the first metatarsal. First we use a power saw to resect the medial hypertrophic bone and cartilage (Fig. 3.5). We then resect the hypertrophic bone laterally. The dorsal resection is via a cut at an oblique angle from the inferior aspect of the typical central chondral defect (Fig. 3.6), usually midline in the central aspect of the defect, terminating at the proximal aspect of the metatarsal neck dorsally on a very oblique angle (Fig. 3.7) avoiding invading the medullary canal of the first metatarsal. After this is removed, we then use a rongeur to resect the hypertrophic bone off the base of the proximal phalanx leaving the standard normal contour of the base of the proximal phalanx and taking what is hypertrophic dorsally, medially, and laterally (the latter which is known as the “Valenti spur”) (Fig. 3.8). Great care is taken to leave the plantar aspect of the joint totally intact (Fig. 3.9). The next focus is on determining the amount of dorsiflexion present. At this point, if the toe is able to be dorsiflexed passively without much pressure to get to 90° of dorsiflexion, everything is left alone. If one is not able to get 90° of dorsiflexion, we then gently free up the tibial and fibular sesamoids from within the joint with a #15 blade eccentrically (from the center medially and from the center laterally). Great care is taken not to disrupt the arterial supply between the sesamoids or below the sesamoids. We just separate the adhesed tissue from the tibial sesamoid medially and the fibular sesamoid laterally, staying between the sesamoids and periosteum as well as bone. After this is performed, we close by hour-glassing the medial and lateral capsule to each other with absorbable suture (2-0 Vicryl™), draped dorsally but not directly interposed between the distal portions of the joint. Hypertrophic synovium that will impede dorsiflexion is resected.
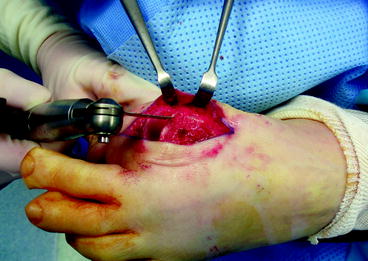

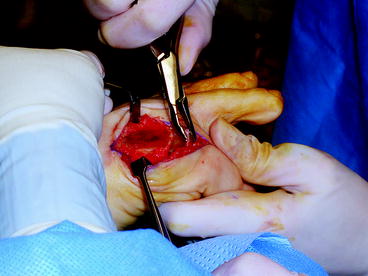
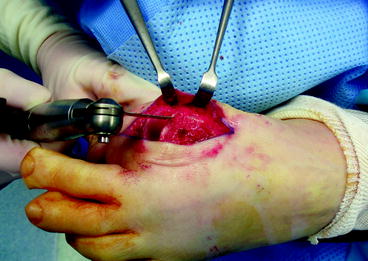
Fig. 3.5
Medial exostosis resection
Fig. 3.6
Dorsal resection of dorsal hyperostosis (a). Note: resection is below the osteochondral defect but is angled to avoid invading the medullary canal (b)

Fig. 3.7
Dorsal resection completed
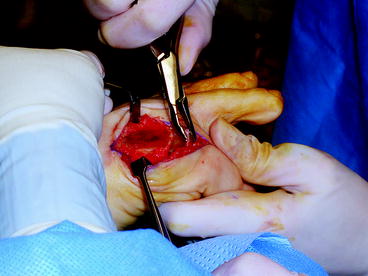
Fig. 3.8
Lateral spur from base of proximal phalanx resected with a rongeur
Fig. 3.9
Diagram showing appropriate resection on both sides of the first MPTJ
Next, attention is focused on closure, and we leave the toe in dorsiflexion when we close (usually about 60° of dorsiflexion) the periosteum and superficial tissue still using 2-0 Vicryl. This is done so that remodeled scar will favor dorsiflexion of the joint. It should be noted that passive dorsiflexion is ideally in the 60–90° range at this point, even after closure (Fig. 3.10). Plantarflexion should also be more than 10° for normal function. Deep closure is performed often with 3-0 Vicryl™ subcutaneous sutures. Skin is closed with a subcuticular suture of 4-0 Monocryl™ or nylon. Postoperative bandaging can consist of steri-strips, Adaptic or Xeroform™, 4 × 4 gauze sponges, and Webril™. Postoperatively, these arthroplasties sometimes swell significantly, especially if the medullary canal was entered with the dorsal resection of bone. If that is the case, swelling will be intolerable if a restrictive, nonelastic dressing is used. The patient will have resultant stiffness from excessive scarring and possible hematoma. To avoid this, we cover the wound with 4 × 4s and Webril® only. Elevation and icing is extremely important in the initial postoperative period (see Chap. 18).










