Hallux Metatarsophalangeal Interposition Arthroplasty (Modified Keller Procedure)
Stuart D. Miller
Hallux rigidus or arthritis of the first metatarsophalangeal (MTP) joint is a very common problem, particularly with the aging of a more athletic population. While a cheilectomy, or resection of the bony osteophytes on the first metatarsal head and proximal phalanx, is a very successful procedure, there is often further damage to the cartilage surface that may cause further pain in the joint and a less than optimal result. The exact amount of damaged cartilage that would require a more extensive procedure rather than a cheilectomy has not been determined. Less favorable results of cheilectomy have been reported with Grades III and IV cartilage damage (1). The treatment for more extensive degenerative disease of the first MTP joint has traditionally been a fusion of the joint. While this procedure has excellent outcomes, many patients prefer to avoid fusion because of limitation of footwear (˜1-inch variation in heel height) and time required to be non-weight bearing for healing.
A number of procedures have been developed for preservation of first MTP joint motion in the face of extensive arthrosis. Barca (2) proposed a round ball of tendon interposition arthroplasty into a joint prepared with convex surfaces, proximal and distal. Hamilton et al. (3) proposed a hallux MTP interposition arthroplasty (modified Keller) procedure with resection of the base of the proximal phalanx and attachment of the short flexor to the short extensor over the metatarsal head. This interposition arthroplasty procedure was associated with problems with toe strength, and long-term results were less favorable than with cheilectomy (4). Inspired by Dr. William Hamilton, my colleagues and I began preserving the base of the proximal phalanx—where the short flexor is attached—and using the joint capsule for interposition (5). This procedure has increased in popularity over the past 14 years. Clinical efficacy of the procedure in severe arthrosis of the first MTP joint has also been reported (6,7).
INDICATIONS AND CONTRAINDICATIONS
Indications
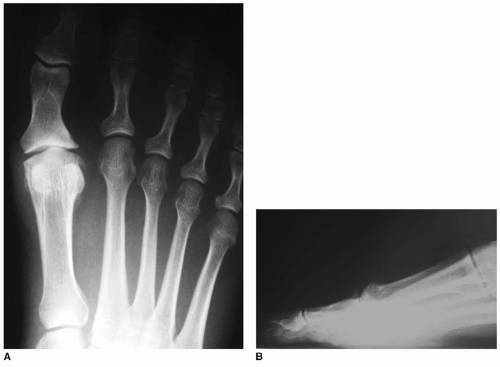
Arthritis in the first MTP joint not responsive to conservative treatment measures (Fig. 5.1)
Grades III and IV damage to articular surfaces of first metatarsal head and/or base of proximal phalanx
Contraindications
Obvious infection
Sesamoid pain
The issue of sesamoid pain deserves special mention. If the patient has significant sesamoid pain, either in the tibial or the fibular sesamoid, and the joint requires better motion, the sesamoid pain may indeed worsen. This serves as a relative contraindication for the procedure, and patients with sesamoid pain must be warned of possibly worsened problems after the procedure. For these patients, a first MTP joint fusion or an alternative interposition arthroplasty procedure with allograft completely encircling the metatarsal head and in between the head and the sesamoids is recommended (8).
PREOPERATIVE PLANNING
Most patients prefer local anesthesia with intravenous sedation. Preoperative planning involves discerning any sesamoiditis, second or third metatarsalgia, or other structural abnormalities that might affect the first MTP joint function. Patients with prior infection may benefit from consultation with an infectious disease specialist. Protocols vary depending on the organism and may involve skin cleansing and nasal antibiotics to decrease the colonization.
SURGICAL TECHNIQUE
The patient is placed in the supine position, with radiographs available for interpretation.
An Esmarch tourniquet about the ankle is adequate. Intravenous antibiotics are given preoperatively.
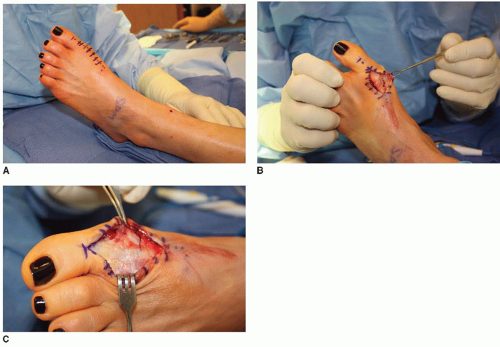
A dorsal approach slightly medial to the extensor hallucis longus (EHL) tendon is undertaken (Fig. 5.2A).
The subcutaneous tissues are examined for the dorsal medial cutaneous nerve, which must be protected; Stevens dissecting scissors work well (Fig. 5.2B).
The first MTP capsule (Fig. 5.2C) can be incised along the medial aspect of the dorsum of the joint. This approach allows visualization of the joint and progression to a simple cheilectomy if possible. A medial dorsal incision is used rather than a more central incision because the capsule will serve as an interposition flap, and transecting it down the middle would severely limit the tissue available for interposition.
The capsular incision is carried onto the proximal phalanx. The incision must be large enough to see the first MTP joint and may require more extensive proximal incision to get over the large dorsal osteophyte on the metatarsal head.
Sharp dissection is used to bring the MTP joint capsule elevation subperiosteal to the lateral aspect of the joint.
Hohmann retractors are used to visualize the lateral aspect of the joint.
In most cases, the medial and lateral collateral ligaments are released from the MTP joint to allow some subluxation of the joint and a better visualization of the plantar joint surfaces. This also allows visualization of the sesamoid and articular cartilage.
If cartilage damage is mild, a simple cheilectomy may be performed and closure can begin. Note that this approach allows closure of the capsule without interfering with the EHL tendon sheath, which has allowed for faster recovery in the author’s experience.
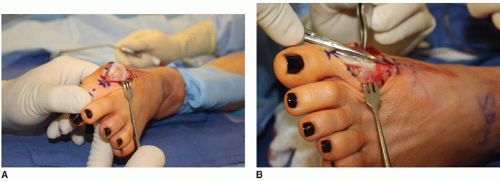
If damage is found to be more extensive and the sesamoid cartilage looks viable, the modified Keller procedure could proceed (Fig. 5.3A).
The incision is carried distally to allow for better visualization of the proximal phalanx and of the joint. This will be carried over at least to the midportion of the proximal phalanx.
The EHL tendon must be visualized and mobilized. A tenolysis of the tendon is done, and the tendon is retracted laterally throughout the case (Fig. 5.3B).
The capsule is incised transversely across the middle of the proximal phalanx (Fig. 5.4).
A corresponding lateral incision in the capsule is brought along the lateral border of the MTP joint dorsally to the metatarsal neck region. This is elevated completely off the proximal phalanx, and the metatarsal head has a free interposition flap with a proximal base (Fig. 5.4C).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree