Hallux Metatarsophalangeal Arthrodesis with and without Intercalated Bone Graft
Bertil W. Smith
The first metatarsophalangeal (MTP) joint is comprised of the round, cartilage-covered first metatarsal head that articulates with the smaller, concave base of the proximal phalanx. The two sesamoids articulate on the plantar surface of the first metatarsal head and are contained within the flexor hallucis brevis tendon. The intersesamoid ligament connects the two sesamoid bones. The tendon of the flexor hallucis longus is protected beneath them. The extensor hallux longus tendon is anchored medially and laterally by the dorsal capsule and MTP joint hood ligaments. The abductor and adductor hallucis tendons pass on the plantar medial and lateral aspect of the first MTP joint. A first MTP arthrodesis maintains first ray length, relieves pain, and permanently corrects deformities of the hallux, allowing for normal shoe wear.
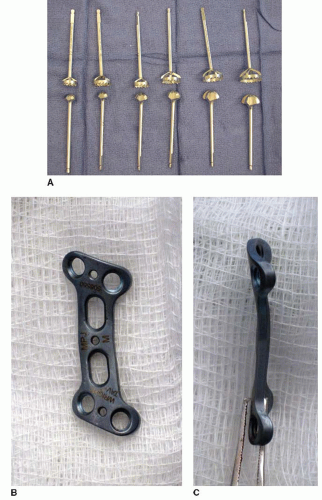
Arthrodesis of the first MTP joint can be used to treat a variety of pathology and conditions. Numerous surgical techniques have been described for the first MTP fusion. These include various approaches, techniques of joint preparation, and methods of internal fixation. The use of flat surfaces for the first MTP fusion is well described and popular with many surgeons. However, this technique requires exact precision to obtain the desired alignment. Additionally, greater shortening of the first ray is required to achieve bony apposition at the fusion site. The author’s preferred technique with a power reaming system coupled with internal fixation using a dorsal precontoured plate provides a strong construct that “brings the bones to the plate,” helping insure correct alignment (Fig. 6.1). This technique has proven to be reliable with an excellent union rate and patient satisfaction. Particular attention to the operative technique will help avoid complications, leading to reproducible results.
INDICATIONS AND CONTRAINDICATIONS
Indications
Advanced hallux rigidus, grade IIIB and grade IV
Severe hallux valgus deformity
Recurrent hallux valgus deformity
Hallux varus deformity
Inflammatory arthropathy
Posttraumatic arthritis
Failed implant arthroplasty, requires a distraction first MTP arthrodesis
Avascular necrosis of the first metatarsal head, requires a distraction first MTP arthrodesis
Contraindications
Impaired vascularity
Active infection
Smoking
Hallux interphalangeal joint arthritis/arthrodesis (relative contraindication)
PREOPERATIVE PLANNING
A complete history and physical examination, including a pulse and sensory exam, should be performed. It is important to evaluate for associated forefoot pathology, including the following:
Crossover toe: The lesser toes should be inspected for either medial or lateral deviation. A drawer test of the lesser MTP joints should be performed. Crossover toe deformities usually affect the second and third toes.
Intractable plantar keratosis: The plantar aspect of the forefoot should be inspected for callosities.
Interdigital neuroma: The interspaces should be palpated for tenderness, and a Mulder test should be performed. Interdigital neuromas most commonly affect the second and third interspaces.
Hammer/mallet toe: The patient should be examined while standing to evaluate for these lesser toe deformities.
Gastrocnemius contracture: A Silferskiöld test should be performed.
First MTP motion is assessed. The presence of midrange pain with a diagnosis of hallux rigidus argues against joint preservation in favor of an arthrodesis. Tenderness to palpation beneath the sesamoids, particularly the tibial sesamoid, should be noted. If there is pain, a callosity, or atrophy of the plantar fat pad, the sesamoid should be excised at the time of the arthrodesis.
Standing radiographs should be obtained as part of the routine preoperative evaluation. It is important that the images be weight bearing for an accurate assessment of the deformity. With a diagnosis of hallux rigidus, the lateral radiograph may be used to evaluate for the presence of an elevated first metatarsal. Up to 5 mm of elevation is normal.
SURGICAL TECHNIQUE
Technique 1: First Metatarsophalangeal Arthrodesis
Positioning
The patient is placed supine on the operating table with a bump under the ipsilateral hip. This allows the foot to rest in a neutral position (Fig. 6.2A).
A regional block or general anesthesia may be used for the procedure.
A sequential compression device is placed on the nonoperative lower extremity.
An Esmarch bandage is used to exsanguinate the foot and is used as an ankle tourniquet wrapped just above the malleoli with a thin layer of padding beneath the bandage (Fig. 6.2B).
Joint Exposure
A dorsal, longitudinal incision is made centered over the first MTP joint (Fig. 6.3A). The incision lies in the internervous plane between the medial and lateral common digital nerves to the hallux.
The incision is extended from a point 3 to 4 cm proximal to the first MTP joint to a point just proximal to the interphalangeal joint of the hallux.

FIGURE 6.3 A: A dorsal incision is made over the first MTP joint. B: The EHL tendon is identified and retracted laterally. C: The first MTP joint is inspected.
Care is taken to identify and protect the tendon of the extensor hallucis longus (EHL) (Fig. 6.3B). The dissection is deepened medial to the EHL tendon, with a dorsal capsulotomy made.
A thorough synovectomy is performed, and the MTP joint is inspected for osteophytes and loose bodies (Fig. 6.3C).
A thin wafer of bone is removed from the articular surface of the first metatarsal head using a sagittal saw (Fig. 6.4A). This helps to “break” the subchondral bony plate and minimize the risk of fragmentation during power reaming.
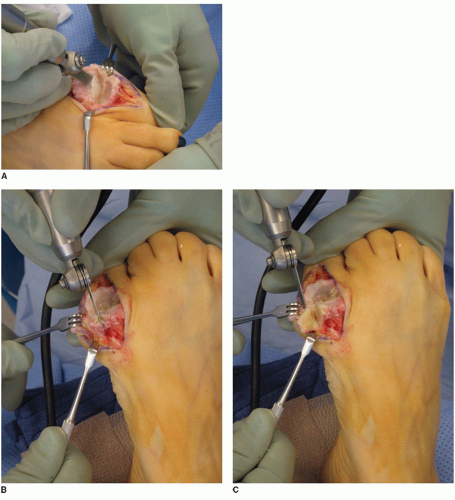
FIGURE 6.4 A: A thin wafer of bone is resected for the first metatarsal head. B,C: The medial eminence is resected when treating a hallux valgus deformity.

FIGURE 6.5 A 0.062-inch Kirschner wire is placed in the center metatarsal head and advanced into the intramedullary canal.
If further shortening of the first ray is needed, a larger bony resection may be made from the first metatarsal head.
The medial eminence is also resected with a sagittal saw if the fusion is performed for a hallux valgus deformity (Fig. 6.4B and C).
Metatarsal Head Preparation
A 0.062-inch Kirschner wire, centered in the metatarsal head, is driven retrograde into the medullary canal of the first metatarsal (Fig. 6.5).
The appropriate size concave reamer is then selected by comparing the diaphyseal metatarsal width with the inner size of the reamer.
The cannulated power reamer is then passed over the Kirschner wire, shaving the metatarsal head subchondral plate to achieve a cancellous, convex bony surface (Fig. 6.6).
Any debris or osteophytes are removed circumferentially around the periphery of the metatarsal head with a rongeur (Fig. 6.7).
Proximal Phalangeal Preparation
A 0.062-inch Kirschner wire, centered at the base of the proximal phalanx, is then driven into the proximal phalangeal medullary canal (Fig. 6.8A).
The smallest of the cannulated, convex reamers is then passed over the Kirschner wire (Fig. 6.8B). Successively larger reamers are used to enlarge the phalangeal surface until it matches that of the prepared metatarsal head.
Final Joint Preparation
Cancellous bony shavings are collected throughout the joint preparation process. These are saved as a bone slurry to use as autograft.
The joint surfaces and incision are copiously irrigated to remove any debris prior to the final step in the joint preparation process.
The 0.062-inch Kirschner wire is then used to perforate the prepared metatarsal and phalangeal joint surfaces in multiple places to increase the surface area for arthrodesis (Fig. 6.9A and B).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree