Guided Growth to Correct Limb Deformity
Ryan D. Muchow
Kenneth J. Noonan
DEFINITION
The anatomic axis is the mid-diaphyseal line of a bone. The anatomic angle of the lower extremity consists of the angle between the anatomic axis of the femur and tibia (normal = 5 to 9 degrees valgus).
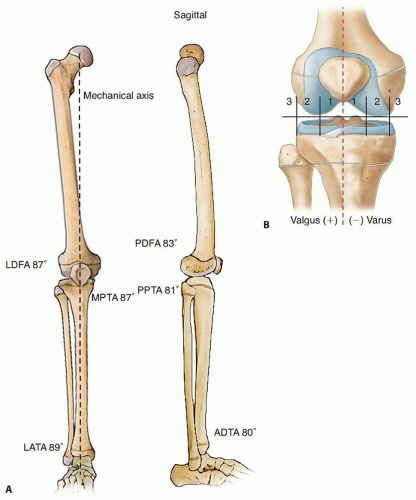
The mechanical axis represents the weight-bearing alignment of a bone or an extremity in either the coronal or sagittal plane. It is a straight line connecting the proximal and distal extent of the bone regardless of its anatomic alignment. For example, the normal mechanical axis of the lower extremity in the coronal plane is a straight line from the center of the femoral head to center of the distal tibia and passes through the middle of the knee (FIG 1).14
The mechanical axis is used to assess coronal and sagittal plane deformity and guide surgical correction to restore a normal weight-bearing alignment. Sagittal plane deformity can also be manipulated to improve the amount of extension at the knee or dorsiflexion at the ankle.
Symmetric physiologic varus is expected between birth and 18 to 24 months, which transitions to a physiologic valgus deformity that is maximal at 3 to 4 years and should correct by 6 to 8 years of age.18
The physis is located at the junction of the epiphysis and metaphysis of long bones and is responsible for longitudinal growth. Consisting of chondrocytes in an extracellular matrix, the cells are oriented longitudinally in four distinct zones: the resting zone, the proliferative zone, the zone of hypertrophy, and the zone of provisional calcification.
The zone of Ranvier is located at the periphery of the physis and contributes to circumferential growth of the physis.
The perichondrial ring of LaCroix is an extension of the diaphyseal bone and periosteum and stabilizes the physis to the periosteum of the bone enhancing the shear strength of the growth plate.1
The Heuter-Volkmann principle states that compression of the growth plate results in slowing the rate of bone growth. Delpech law is related in that tension across the growth plate increases the rate of bone growth.
Guided growth or growth modulation techniques use the Heuter-Volkmann principle to affect the rate of growth at one part of the physis relative to another to gain correction of deformity in the coronal or sagittal plane. Common lower limb deformities that are treated with guided growth include pathologic:
ANATOMY
Hip
Neck-shaft angle (NSA) = 130 degrees
Knee
Lateral distal femoral angle (LDFA) = 87 degrees
Medial proximal tibia angle (MPTA) = 87 degrees
Posterior distal femoral angle (PDFA) = 83 degrees
Posterior proximal tibia angle (PPTA) = 81 degrees
Ankle
Lateral distal tibia angle (LDTA) = 89 degrees
Anterior distal tibia angle (ADTA) = 80 degrees
Center of rotation of angulation (CORA) is the location of deformity in a long bone. If a single point of deformity exists, the point of intersection between the proximal mechanical axis and the distal mechanical axis is the CORA and it should correspond to anatomic deformity. If a constructed CORA does not correspond with obvious anatomic deformity, another deformity must exist. Therefore, deformity correction should occur at the CORA to restore the mechanical axis.14
Assessment of the physis should occur to ensure adequate growth is available for guided growth. This would include checking for physeal bars and to identify whether the physis is normal or pathologic secondary to an underlying etiology.
Secondary problems
Limb length discrepancy
Rotational problems
Osteochondritis dissecans
Angular problems resulting in subluxation
Hip—coxa valga
Patella—genu valgum
PATHOGENESIS
Physiologic
Idiopathic genu valgum
Heuter-Volkmann principle
Infantile and adolescent tibia vara
Acquired (insult to the physis)—trauma, infection, radiation, iatrogenic, juvenile inflammatory arthritis, osteochondroma
Congenital (condition affecting the health/growth of the physis)—skeletal dysplasia, focal fibrocartilaginous dysplasia, osteogenesis imperfecta, multiple hereditary exostosis, Ollier disease, Maffucci syndrome
Metabolic bone disease (the physis is susceptible to the Heuter-Volkmann principle at the age of physiologic angulation, for example, onset before 2 years of age will lead to progressive varus, after 4 or 5 years of age will lead to progressive valgus)—rickets, renal osteodystrophy
Adaptive response to a long bone deformity
NATURAL HISTORY
Physiologic = spontaneous resolution
Progressive angular deformity can cause gait disturbance, limitations in function, and pain.
There is no consistent evidence demonstrating what degree of malalignment could lead to osteoarthritis and at what age. Various biomechanical and gait studies describe increased force through the medial and lateral compartments with genu varum and valgum, respectively, but this has not been shown to cause osteoarthritis.4, 9, 12, 24
PATIENT HISTORY AND PHYSICAL FINDINGS
History is important to identify underlying pathology and determine growth potential.
Current symptoms
Pain, functional limitations, cosmetic concerns
Observe gait
Thrust, instability, crouch, equinus
Assess for limb length discrepancy and rotational profile.
Joint examination
Range of motion of affected and adjacent joints
Joint instability and pain
Foot deformities
IMAGING AND OTHER DIAGNOSTIC STUDIES
Plain radiographs (as indicated)
Bone age
Lower extremity
Standing, full-length anteroposterior (AP) alignment radiograph
Lateral views of the lower extremities and joints involved
Consider comparison views
Consider scanogram
Standing lateral foot film to assess foot height
Computed tomography (CT)—most accurate assessment of rotational profile and best method to assess individual bone lengths in children with sagittal plane joint contractures
CT or magnetic resonance imaging (MRI)—identifies a physeal bar
DIFFERENTIAL DIAGNOSIS
Physiologic
Idiopathic genu valgum
Infantile and adolescent tibia vara
Acquired: trauma, infection, radiation, iatrogenic, juvenile inflammatory arthritis, osteochondroma, adaptive response to a long bone deformity
Congenital: skeletal dysplasia, focal fibrocartilaginous dysplasia, osteogenesis imperfecta, multiple hereditary exostosis, Ollier disease, Maffucci syndrome
Metabolic bone disease: rickets, renal osteodystrophy
NONOPERATIVE MANAGEMENT
Pathologic conditions by definition are progressive and therefore not commonly amenable to observation or bracing.
Metabolic disorder—treat and optimize underlying condition first, then if progressive deformity remains, guided growth is indicated.
SURGICAL MANAGEMENT
Progressive angular deformity resulting in pain or functional limitation
Must have a physis with sufficient growth remaining (variable based on location of physis, patient, and pathology). It is important to remember that in some syndromes, the radiographic presence of an open growth plate does not ensure that the physis is growing sufficiently to correct deformity via guided growth.
Surgical options
Temporary hemiepiphysiodesis
Rigid stapling
Percutaneous screw (Metaizeau)
Tension band plate and screws
Stainless steel or titanium
Cannulated or solid screws
One or two plates
Permanent hemiepiphysiodesis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree