Growth, Growth Hormone, and Pituitary Disorders
Leslie P. Plotnick
Ryan S. Miller
Problems related to growth are commonly observed in pediatric practice. Short stature can be defined as height more than two standard deviations (SDs) below the mean and tall stature as height more than two SDs above the mean. By definition, 3% of children have short stature and 3% have tall stature. On the other hand, growth is dynamic, and growth velocity is defined as the increase in length or height over time.
Measurement of growth velocity over a period of time in addition to determination of stature at any given point in time both are essential in deciding whether a child may have a
problem with growth. A child may have normal height and weight but a subnormal rate of growth, indicating the need for an evaluation. The growth of an individual can be assessed adequately only through obtaining regular height and weight measurements and accurately plotting these measurements on growth curves to detect deviations from normal velocities (see Chapter 5, Pediatric History and Physical Examination, for height and weight curves for girls and boys, birth to 36 months and 2 to 18 years).
problem with growth. A child may have normal height and weight but a subnormal rate of growth, indicating the need for an evaluation. The growth of an individual can be assessed adequately only through obtaining regular height and weight measurements and accurately plotting these measurements on growth curves to detect deviations from normal velocities (see Chapter 5, Pediatric History and Physical Examination, for height and weight curves for girls and boys, birth to 36 months and 2 to 18 years).
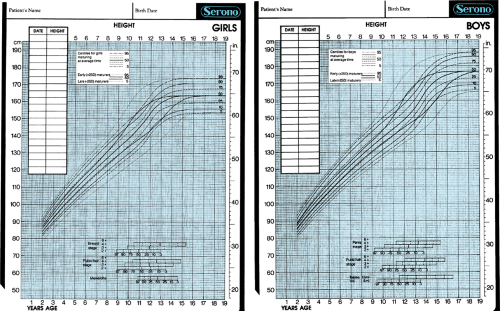
Because the timing of puberty affects growth rate, Tanner has modified the growth curves to include curves for early and late developers. These curves are especially useful in evaluating adolescents with early-normal and late-normal onset of puberty and should be used to assess the normality of growth in these children (Fig. 375.1).
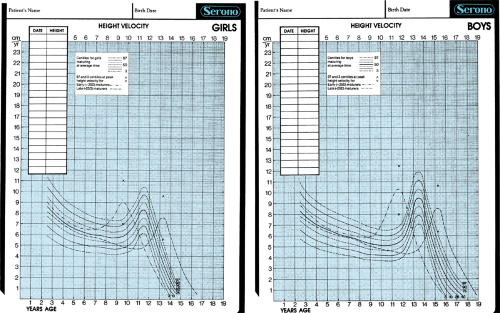
Growth velocity curves are important to use when evaluating children for disorders of growth. These curves are shown in Fig. 375.2. Velocities for children with early-normal and late-normal puberty are superimposed on the curves.
Bone age also is important in evaluating a child for a growth problem. A child with normal bone age is unlikely to have a systemic chronic disease or a hormonal abnormality as the cause of the growth problem. Significantly delayed or advanced bone ages (i.e., greater than two SDs from the mean) may indicate pathology and require evaluation.
SHORT STATURE OR POOR LINEAR GROWTH
A child with a height below the third percentile or whose growth curve has been crossing percentiles downward should be examined carefully for a pathologic cause of poor growth (Box 375.1). However, for children who are born smaller or larger than their genetic growth potential to gradually shift percentiles, up or down, for height and weight is not unusual. For example, a child who at birth is in the 90th percentile for length and weight but whose parents are in the tenth percentile for height may decelerate gradually to the tenth percentile over the course of the first 2 years of life. Sometimes differentiating this pattern from pathologic growth is difficult. The key points are a gradual deceleration of height and weight proportionally, deceleration not below the genetically anticipated percentile, and once the percentile is reached, velocities normalizing and height and weight remaining at that percentile. If the deceleration is abrupt and falls to less than the third percentile or to a percentile below the parents’ percentile, further evaluation is needed.
A large percentage of children with poor growth have major organ system disease that is responsible for their growth failure. Most patients in this category have a disorder that is not subtle, and the history and physical examination disclose the problem without extensive laboratory testing. However, some disorders may not be evident from history and physical examination and, therefore, require laboratory studies for diagnosis.
Renal disorders, particularly renal tubular acidosis, require evaluation by electrolytes, chemistries, and urinalysis. Particularly difficult to define are patients with gastrointestinal (GI) abnormalities. Patients with inflammatory bowel disease, especially Crohn disease, may have growth failure for several years before GI symptoms become evident. A complete blood cell count with an erythrocyte sedimentation rate and/or C-reactive protein may be helpful, but GI contrast studies and endoscopy are required to make the diagnosis. Patients with celiac disease may not have the classic history of malabsorption and hyperphagia. These children may have poor appetites or may have no symptoms other than poor growth. Laboratory tests (tissue transglutaminase and antiendomysial antibodies) may help with this diagnosis, but the definitive diagnostic test is a small-bowel biopsy. The decision as to when to do more extensive GI studies (e.g., radiologic, endoscopic) rests on the persistence of a poor growth rate over time, with other laboratory tests remaining normal and no other diagnosis being made, especially if the child’s weight is affected more than is height. Malnutrition of any cause, including malabsorption or inadequate caloric intake, is associated with poor growth.
Poor growth also may be due to inborn metabolic errors, chromosomal abnormalities, and a variety of dysmorphic syndromes including Turner syndrome, Prader-Willi syndrome (PWS), Russell-Silver syndrome, and Noonan syndrome. Turner syndrome and its variants (i.e., absence or structural abnormalities of one X chromosome or a mosaic pattern) may manifest with classic phenotypic features or may have only minor clinical features. Girls with non-45X karyotypes (i.e., mosaics, rings, isochromes, or partial X deletions) are more likely to lack the classic phenotypic features. All short girls with subnormal growth rates should have banded karyotyping as part of the laboratory evaluation. Turner syndrome may be as common as growth hormone (GH) deficiency and should be considered in all short girls. Growth curves for girls with Turner syndrome are available.
Children born small for gestational age (SGA), which is defined as weight or length greater than or equal to two SDs below the mean for gestational age, may have poor postnatal growth and resultant short stature. These children may have dysmorphic features, indicating a specific syndrome associated with intrauterine growth retardation. They may be nondysmorphic but thin, especially with very thin extremities, minimal body fat, and thin, narrow faces. Bone ages may be delayed or normal. Approximately 15% fail to catch up by 2 years of age, and approximately half of these children will remain short as adults.
Skeletal dysplasias resulting in poor growth occasionally may be subtle. The skeletal abnormalities usually are evident on physical examination. Careful measurement of upper and lower segment ratios may aid in establishing the diagnosis. Radiologic studies can help identify the specific abnormalities.
Nutritional deficiencies are an important cause of growth retardation throughout the world. In the developed countries, it may be caused by GI pathology, familial psychosocial problems, or self-imposed caloric deprivation. The last one is an important problem in the United States. Anorexia nervosa is associated with both inadequate weight gain and linear growth retardation. Normal GH levels and low insulinlike growth factor (IGF-1) have been observed. Linear growth and lab markers typically normalize with refeeding.
Psychological factors also have been associated with poor growth. Children in disturbed families may have psychosocial dwarfism, with disturbed eating and sleeping behaviors and transient pituitary hormone deficiencies, especially of GH and adrenocorticotropic hormone. When the child is removed from the adverse home environment, catch-up growth occurs and the hormonal levels normalize.
Various medications may produce poor growth. Glucocorticoids will be discussed later in this chapter. Stimulants such as amphetamines and methylphenidate and similar medications, especially in high doses, have been associated with short-term impairment of weight and height. However, longer-term studies have shown no evidence of height deficits in late adolescence and no difference in adult stature.
Familial or genetic short stature is characterized by height below the third percentile, normal growth rate, and skeletal age appropriate for chronologic age. It is a common cause of short stature in children. Usually the parents’ heights are in the lower normal percentiles for adults. Children with familial short stature are entirely normal. Their heights usually are at or slightly below the third percentile but not at or more than
three SDs below the mean. They have normal growth velocities, and their height curves parallel the third percentile. Their bone ages are normal, and their pubertal growth spurts are normal in timing and magnitude.
three SDs below the mean. They have normal growth velocities, and their height curves parallel the third percentile. Their bone ages are normal, and their pubertal growth spurts are normal in timing and magnitude.
BOX 375.1 Causes of Short Stature or Poor Linear Growth
Major organ system disease
Central nervous system
Cardiac
Pulmonary
Hematologic
Renal
Gastrointestinal or nutritional
Chromosomal disorders: Turner syndrome, others
Inborn errors of metabolism
Intrauterine growth restriction (small for gestational age)
Familial or genetic short stature
Constitutional delay of growth and adolescence
Endocrine disorders
Cortisol excess (exogenous or endogenous)
Hypothyroidism
Pseudohypoparathyroidism
Poorly controlled diabetes
Growth hormone deficiency (e.g., idiopathic, organic, familial, psychosocial)
Growth hormone insensitivity (resistance)
Shifting linear percentiles
Skeletal disorders
Nutritional
Deprivation or psychosocial dwarfism
Medications
One or both of the parents may be short for a pathologic reason, such as familial GH deficiency or mild chondrodysplasias, which the child may have inherited. If a parent’s height is more than two SDs below the mean (i.e., less than the third percentile) or if the parent is disproportionately short for his or her family, both parent and child may have a pathologic cause for their short stature.
Children may exhibit a delayed growth pattern, characterized by a 2to 4-year lag in height, bone age, and pubertal development. Epiphyseal fusion is delayed, and most individuals reach normal adult height. This pattern of growth is commonly a manifestation of constitutional delay of growth. This variant of normal growth is seen more frequently in boys than in girls. Often, the family history in parents, older siblings, or other family members is positive for this growth pattern.
If the growth rate is normal, the height is at or slightly below the third percentile, the bone age is delayed by 2 to 4 years, and predicted height falls within genetic target range, no additional evaluation is needed. However, if any concern about a subnormal growth velocity exists, further evaluation is indicated. Patients with chronic illness, such as sickle cell disease, asthma, or inflammatory bowel disease, or with milder degrees of GH deficiency may resemble children with constitutional delay. Because growth velocity gradually drops with age and is at its lowest just before the pubertal growth spurt begins (Fig. 375.2), teenagers with constitutional delay may spend a prolonged time at this low rate. Growth velocity should be assessed in relation to bone age, chronologic age, and pubertal stage.
Patterns of growth failure often are distinct. However, more than one pattern can be present in an individual. For example, the combination of familial or genetic short stature and constitutional delay may occur together, producing severe short stature.
Endocrine abnormalities resulting in short stature include glucocorticoid excess, hypothyroidism, and growth hormone deficiency. Pseudohypoparathyroidism (PHP) is a rare disorder with a characteristic phenotype that includes short stature. Poorly controlled insulin-dependent diabetes mellitus may be associated with short stature and poor linear growth rate. The growth retardation in poorly controlled diabetes can be severe. Improving metabolic control usually normalizes the growth rate, and catch-up growth can occur.
Glucocorticoid excess (i.e., cortisol in greater amounts than physiologic needs) produces short stature, whether the excess cortisol is exogenous (caused by oral, topical, or inhalant glucocorticoids) or endogenous (as in Cushing disease). Children with cortisol excess have a subnormal linear growth rate and delayed bone age, and they may exhibit cushingoid features: round, plethoric “moon” face; centripetal obesity; increased dorsal fat pad (“buffalo hump”); and proximal muscle weakness. When the source of excess glucocorticoids is removed, the growth rate increases, but the ultimate height can be compromised by having had glucocorticoid excess for years.
Hypothyroidism in children is characterized by a subnormal linear growth rate, increased weight gain, and a delayed bone age. When the diagnosis is made and appropriate treatment given, children undergo catch-up growth, although their ultimate height can be compromised. The threshold for performing thyroid function tests should be low for a child with a question of poor growth rate because the diagnostic tests and treatment are of minimal risk, inexpensive, and effective. Treatment often has dramatic effects on clinical signs and symptoms and on growth.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree