Chapter 169 Gout
 Diagnostic Summary
Diagnostic Summary
• Acute onset, frequently nocturnal, with typically monoarticular joint pain, involving the metatarsophalangeal joint of the big toe in about 50% of cases
• Elevated serum uric acid level
• Asymptomatic periods between acute attacks
• Identification of urate crystals in joint fluid
• Aggregated deposits of monosodium urate monohydrate (tophi) chiefly in and around the joints of the extremities but also in subcutaneous tissue, bone, cartilage, and other tissues
 General Considerations
General Considerations
Gout is a common type of arthritis caused by an increased concentration of uric acid (the final breakdown product of purine metabolism) in biological fluids. In gout, uric acid crystals (monosodium urate) are deposited in joints, tendons, kidneys, and other tissues, where they cause considerable inflammation and damage.1 Gout is a condition characterized biochemically by increased serum uric acid levels, leukotriene levels, and neutrophil accumulation. Gout may lead to debilitation owing to the tophaceous deposits around the joints and tendons; renal involvement may result in kidney failure due to either parenchymal disease or urinary tract obstruction.
Gout is associated with affluence and is often called the “rich man’s disease.” Throughout history, the sufferer of gout has been depicted as a portly, middle-aged man sitting in a comfortable chair with one foot resting painfully on a soft cushion as he consumes great quantities of meat and wine. In fact, the traditional picture does have some basis in reality, as meats, particularly organ meats, are high-purine foods, whereas alcohol inhibits uric acid secretion by the kidneys. Furthermore, even today, gout is primarily a disease of adult men; more than 95% of sufferers of gout are men older than age 30. The incidence of diagnosed gout cases has been estimated at 2.13% of the 2009 U.S. population, although 10% to 20% of the adult population has hyperuricemia. Gout is a strong predictor of the metabolic syndrome and an increased risk for type 2 diabetes.1–4
Causes of Gout
Gout is classified into two major categories: primary and secondary. Primary gout accounts for about 90% of all cases, whereas secondary gout accounts for only 10%. Primary gout is usually idiopathic (i.e., the underlying metabolic defect is unknown). However, there are several genetic defects in which the exact cause of the elevated uric acid is known.1 The synthesis and degradation of purines are summarized in Figure 169-1.
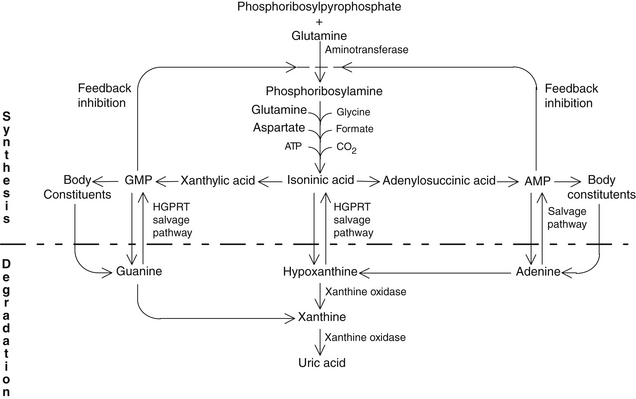
FIGURE 169-1 Purine synthesis and degradation.
(From Nutrition Foundation. Nutrition reviews’ present knowledge in nutrition, ed 5. Washington, DC: Nutrition Foundation, 1984:740-756.)
The term secondary gout refers to those cases in which the elevated uric acid level is secondary to some other disorder such as excessive breakdown of cells or some form of renal disease. Diuretic therapy for hypertension and low-dose aspirin therapy are also important causes of secondary gout because they cause decreased uric acid excretion.
• Increased synthesis of uric acid, found in a majority of individuals
• Reduced ability to excrete uric acid, typical of a smaller group (about 30%)
• Overproduction of uric acid, as well as underexcretion of uric acid—a small minority
Although the exact metabolic defect in gout is unknown in the majority of cases, gout is one of the most controllable metabolic diseases. Box 169-1 summarizes the causes of gout.
BOX 169-1 Causes of Hyperuricemia
Metabolic
• Increased production of purine (primary)
• Specific enzyme defects (e.g., Lesch-Nyhan syndrome, glycogen storage disease)
• Decreased enzyme activity (e.g., hypoxanthine-guanine phosphoribosyltransferase is decreased in 1% to 2% of adults with gout)
• Increased enzyme activity (e.g., phosphoribosylpyrophosphate synthetase)
• Increased production of purine (secondary)
• Increased turnover of purines
• Myeloproliferative disorders
• Lymphoproliferative disorders
• Carcinoma and sarcoma (disseminated)
• Increased de novo synthesis (e.g., glucose-6-phosphatase deficiency)
• Increased catabolism of purines
• Fructose ingestion or infusion
Renal
• Decreased renal clearance of uric acid (primary)
• Decreased renal clearance of uric acid (secondary)
• Functional impairment of tubular secretion
• Drug-induced (e.g., thiazides, probenecid, salicylates, ethambutol, pyrazinamide)
• Hyperlacticemia (e.g., lactic acidosis, alcoholism, toxemia of pregnancy, chronic beryllium disease)
• Hyperketoacidemia (e.g., diabetic ketoacidosis, fasting, starvation)
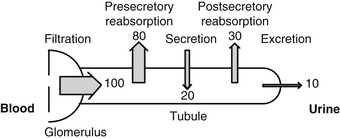
Almost all of the plasma urate is filtered at the glomerulus: only the small amount bound to protein is not filtered. Renal excretion is peculiar in that about 80% of the filtered uric acid is reabsorbed in the proximal tubule of the nephron. Actually, the distal tubule secretes most of the uric acid found in the urine. Distal to this site, some postsecondary reabsorption occurs. These events are summarized in Figure 169-2.
Uric acid is a highly insoluble molecule; at pH 7.4 and body temperature, the serum is saturated at 6.4 to 7 mg/100 mL. Although higher concentrations do not necessarily result in urate deposition (some unknown factor in serum appears to inhibit urate precipitation), the chance of an acute attack is greater than 90% when the level is above 9 mg/100 mL (Table 169-1). Lower temperatures decrease the saturation point of uric acid, which may explain why urate deposits tend to form in areas such as the pinna of the ear, where the temperature is lower than the mean body temperature (Table 169-2). Uric acid is insoluble below pH 6 and can precipitate as the urine is concentrated in the collecting ducts and passed to the renal pelvis.
TABLE 169-1 Prevalence of Gouty Arthritis by Maximum Urate Level
| SERUM URATE (mg/100 mL) | MEN (%) | WOMEN (%) |
|---|---|---|
| <6 | 0.6 | 0.08 |
| 6-6.9 | 1.9 | 3.3 |
| 7-7.9 | 16.7 | 17.4 |
| 8-8.9 | 25 | 0 |
| 9+ | 90 | 0 |
Data from Faller J, Fox IH. Ethanol-induced hyperuricemia: evidence for increased urate production by activation of adenine nucleotide turnover. N Engl J Med 1982;307:1598-1602.
TABLE 169-2 Solubility of Urate Ion as a Function of Temperature in 140 mM Na+
| TEMPERATURE (°C) | MAXIMUM SOLUBILITY (mg/100 mL) |
|---|---|
| 37 | 6.8 |
| 35 | 6 |
| 30 | 4.5 |
| 25 | 3.3 |
| 20 | 2.5 |
| 15 | 1.8 |
| 10 | 1.2 |
Data from Faller J, Fox IH. Ethanol-induced hyperuricemia: evidence for increased urate production by activation of adenine nucleotide turnover. N Engl J Med 1982;307:1598-1602.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree