Chapter 1 Good posture and how it can be achieved
INTRODUCTION
Posture when observed in others may be felt to range between good and bad, and these deviations are difficult to identify without a prescription for ideal, erect human posture. However, it must be noted that in reality normal posture and particularly good normal posture rarely exists, and when assessing and correcting posture it is essential to consider inherent physical features such as body type and proportions, together with ligament length and joint mobility. For example, people with loose ligaments tend to stand with hyperextended knees and hips (resting on their iliofemoral ligaments) and with flexible, exaggerated curves of the spine that are much greater than those seen in people with tighter ligaments.
HOW THE MODERN HUMAN REMAINS ERECT
Gravity is constantly pulling the body as a whole towards the ground. This force is counteracted by the tone of the postural muscle group, a role that cannot be overestimated because the bones of the skeleton, especially the long limb bones, are too irregularly shaped to stand upon each other and maintain the upright position alone. However, muscles do not maintain the erect position alone and their ability to counteract gravity is under the control of the central nervous system which is implemented by information contributed by ligaments, tendons, joints and the muscles themselves, together with input from special senses, mainly visual and vestibular, which help to identify the position of the head in space. Other systems involved less directly by contributing to metabolic homeostasis include the respiratory, circulatory, excretory, digestive and endocrine systems (Thibodeau & Patton 1993).
Summary
Advantages of good posture
 It ensures that the progressive, but controlled, development of all the postural muscles is both promoted and maintained.
It ensures that the progressive, but controlled, development of all the postural muscles is both promoted and maintained. It helps to maintain overall body fitness so that physical activity is efficient and well coordinated.
It helps to maintain overall body fitness so that physical activity is efficient and well coordinated. It helps to compensate for skeletal changes that occur, for instance in prolonged illness, as well as with advancing age.
It helps to compensate for skeletal changes that occur, for instance in prolonged illness, as well as with advancing age.GOOD ERECT POSTURE
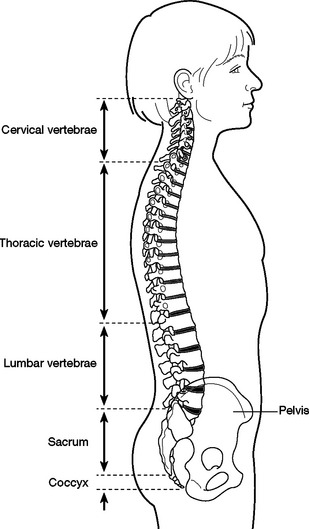
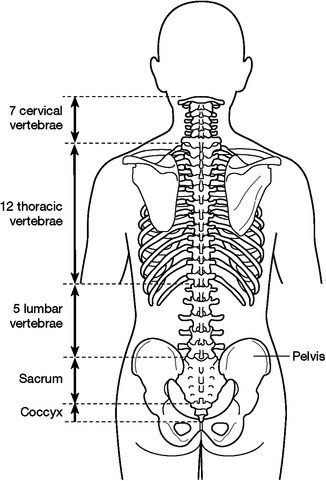
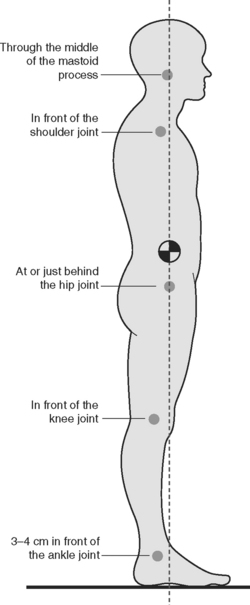
Good erect posture (Fig. 1.1) requires an understanding of the vertebral column’s structure and function as well as the basic principles of maintaining an upright stance. It also demands the ability to observe and assess posture so as to recognize common postural habits, faults and movement patterns.
These are discussed under the following headings:
BASIC PRINCIPLES OF MAINTAINING AND UPRIGHT STANCE
Spinal anatomical structures
‘The back’ or ‘the spine’ comprises the vertebral column and associated ligaments and muscles, together with the intervertebral discs and the contents of the vertebral canal (Figs 1.2 & 1.3).
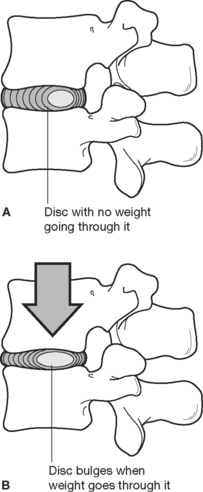
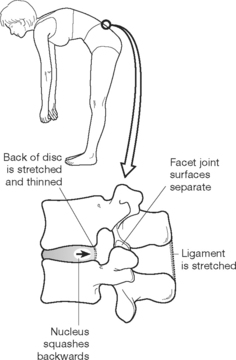
The intervertebral discs cushion the bony vertebrae, providing shock absorption and giving flexibility for the spine to move. The shock absorption properties of the discs are essential in protecting the spine from trauma during everyday activities and are particularly effective for walking, going up or down steps or inclines, running, etc. In addition, the health and integrity of the intervertebral discs determine to a great extent the overall function of the spine as the discs allow movement to occur between each vertebra during bending, stretching and twisting, and movements comprised of combinations of these possibilities.
In a healthy disc, the spongy, jelly-like nucleus is enclosed within a fibrous ring (annulus) that allows the disc to change shape during movement but prevents the nucleus leaking out. The ability of the nucleus to change shape during loading and unloading of the spine is demonstrated in Figures 1.4–1.6.
As the disc nucleus contains a great deal of water, constant pressure exerted on the discs throughout the day will adversely affect their overall size, sponginess and shock-absorbing properties. As the day progresses, water leaks from the discs causing shrinkage of the nucleus. This leads to a loss of disc height that results in less effective disc function and overall mobility and function of the spine itself. However, these changes are reversed during periods of rest, especially when recumbent in bed at night, and varying the amount of pressure exerted on the discs throughout the day can also help to maintain and improve disc health and function (Fig. 1.7).
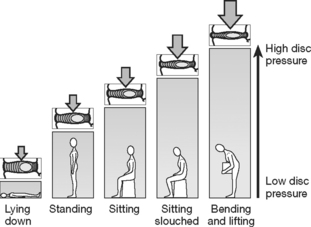
Figure 1.7 How pressure on the discs is affected by different postures.
Redrawn with permission from Oliver (1999).
The intervertebral discs permit movement of the spine, and the range and types of movement are limited by the shape and structure of the different types of vertebra (compare the cervical and lumbar regions) and the strength and length of the ligaments. Movement is controlled by the muscles of the spine and trunk under the influence of motor nerve impulses from the brain.
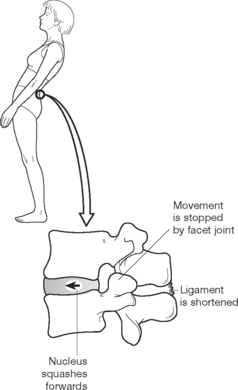
In the normal spine, the small facet joints on the posterolateral aspects of the vertebrae fit neatly together, so that hyperextension and extreme twisting movements are limited. However, narrowing of the intervertebral space through an exaggerated lumbar lordosis or damage to the intervertebral discs places undue stress on the joints causing pain (Fig. 1.8).
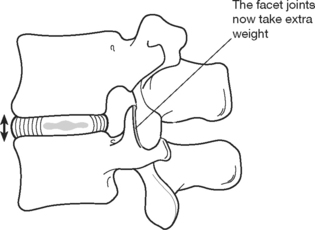
Figure 1.8 Narrowing of disc space increases pressure on facet joints.
Redrawn with permission from Oliver (1999).
Muscles and ligaments supporting the vertebral column
Muscles
The erector spinae is a longitudinal mass of muscles ascending along the posterior aspect of the vertebral column from the sacrum to the skull (Figs 1.9 & 1.10A&B). This large and somewhat complex extensor of the spine is divided into three parallel columns termed deep, middle and superficial, each further subdivided into individually named components arranged in ascending series.
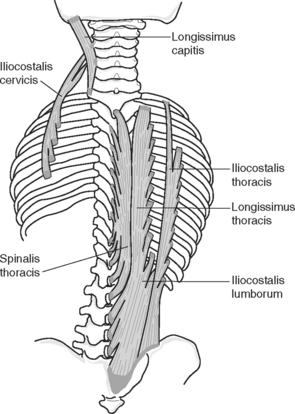
Figure 1.10B The erector spinae muscle showing its constituent parts.
Reproduced with permission from Palastanga et al (2006).
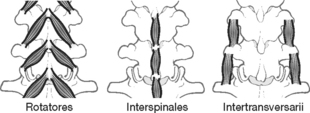
Deep layer – interspinales, intertransversarii, rotatores
 Interspinales: these small muscles, lying in series together with the interspinous ligaments, join adjacent spinous processes.
Interspinales: these small muscles, lying in series together with the interspinous ligaments, join adjacent spinous processes. Intertransversarii: these are a similar series of thin muscles that join adjacent transverse processes; they tend to be stronger in the upper part of the erector spinae.
Intertransversarii: these are a similar series of thin muscles that join adjacent transverse processes; they tend to be stronger in the upper part of the erector spinae. Rotatores: these join one transverse process to the spinous process of the vertebra above; they are confined to the thoracic spine, which is where the only true rotation of the vertebral column can occur.
Rotatores: these join one transverse process to the spinous process of the vertebra above; they are confined to the thoracic spine, which is where the only true rotation of the vertebral column can occur.Middle layer – multifidus, semispinalis, levatores costarum
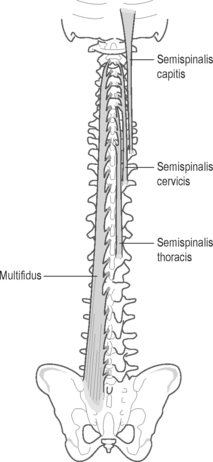
 Multifidus: this has the deepest and shortest muscle fibres in this layer. Each extends from the laminae and mamillary processes of one vertebra to the spinous process of a vertebra that is positioned two or three segments above. Multifidus extends in series from the sacrum to the upper part of the neck.
Multifidus: this has the deepest and shortest muscle fibres in this layer. Each extends from the laminae and mamillary processes of one vertebra to the spinous process of a vertebra that is positioned two or three segments above. Multifidus extends in series from the sacrum to the upper part of the neck. Semispinalis: the fibres of this muscle lie superficial to multifidus, and extend over three levels from the lower thoracic region to the base of the skull, named in ascending order: semispinalis thoracis, cervicis and capitis:
Semispinalis: the fibres of this muscle lie superficial to multifidus, and extend over three levels from the lower thoracic region to the base of the skull, named in ascending order: semispinalis thoracis, cervicis and capitis: Levatores costarum: these are small, strong, triangular muscle pairs, 12 in number, found between the eleventh thoracic and seventh cervical vertebrae. Each of the 12 pairs descends from the transverse process of the vertebra above to the upper border of the rib below, near its tubercle. The fibres fan out as they pass downwards and laterally (Palastanga et al 2002, p. 481).
Levatores costarum: these are small, strong, triangular muscle pairs, 12 in number, found between the eleventh thoracic and seventh cervical vertebrae. Each of the 12 pairs descends from the transverse process of the vertebra above to the upper border of the rib below, near its tubercle. The fibres fan out as they pass downwards and laterally (Palastanga et al 2002, p. 481).Superficial layer – iliocostalis (lateral), longissimus (intermediate) and spinalis (medial)
 Iliocostalis: the lateral column has three sections ascending in series: iliocostalis lumborum, thoracis and cervicis.
Iliocostalis: the lateral column has three sections ascending in series: iliocostalis lumborum, thoracis and cervicis. Longissimus: the intermediate and strongest column similarly has three sections: longissimus thoracis, cervicis and capitis.
Longissimus: the intermediate and strongest column similarly has three sections: longissimus thoracis, cervicis and capitis. Spinalis: is the relatively insignificant medial column, subdivided into spinalis thoracis, cervicis and capitis, of which spinalis thoracis is the most clearly defined. Spinalis cervicis and capitis are small, poorly defined and are frequently merged with adjacent sacrospinalis muscle columns.
Spinalis: is the relatively insignificant medial column, subdivided into spinalis thoracis, cervicis and capitis, of which spinalis thoracis is the most clearly defined. Spinalis cervicis and capitis are small, poorly defined and are frequently merged with adjacent sacrospinalis muscle columns.Body mass and centre of gravity
The centre of mass of an object is defined as the point about which the mass is evenly distributed and this definition cannot easily be applied to the irregularly shaped human body. However, by first considering the mass of the whole body and then assessing the percentage that the head, neck, trunk, upper and lower limbs individually contribute, allows an approximation of where the centre of gravity would lie when the body is standing upright (Table 1.1).
Table 1.1 Mass of each body segment in percentage of total body mass
| Segment | % of body mass |
|---|---|
| Trunk | 49.7 |
| Head and neck | 8.1 |
| Upper arm | 2.8 each |
| Lower arm | 1.6 each |
| Hand | 0.6 each |
| Total arm | 5.0 each |
| Upper leg | 10.0 each |
| Lower leg | 4.7 each |
| Foot | 1.4 each |
| Total leg | 16.1 each |
Reproduced with permission from Palastanga et al (2002).
Balance and stability
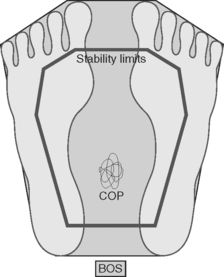
A body’s shape, mass and orientation in relation to the surface area, shape and position of its base of support determines where both its centre and line of gravity will lie (Fig. 1.11). All these factors contribute to overall balance and stability.
A stable body will have a stable centre of gravity lying sufficiently low above its base of support to ensure this. Additionally, its line of gravity should fall through the centre of pressure to lie within the base of support.
POSTURAL OBSERVATIONAL SKILLS AND ASSESSMENT
Body types
The basic anthropometrics classifications are as follows:
 Endomorphs are inclined to be pear shaped with comparatively shorter limbs and extra subcutaneous fat around the hips and thighs.
Endomorphs are inclined to be pear shaped with comparatively shorter limbs and extra subcutaneous fat around the hips and thighs. Ectomorphs tend to have slender, lean bodies with comparatively poor muscular development, do not gain body weight easily and may even be underweight.
Ectomorphs tend to have slender, lean bodies with comparatively poor muscular development, do not gain body weight easily and may even be underweight.Assessment procedures
Assessment of static standing posture
Exercises to improve spine mobility should aim to provide continuous support for the intrinsic spinal structures whilst moving each vertebral joint through its optimum range of movement (see Chapter 4).
Assessment of sitting
Ideal sitting posture
In correct sitting posture the body weight is adjusted to balance over the ischial tuberosities so that, together with the thighs, they provide a stable base of support (Fig. 1.12). The knees are flexed approximately 90 degrees and the lower legs are perpendicular, with the heels aligned with the backs of the knees.
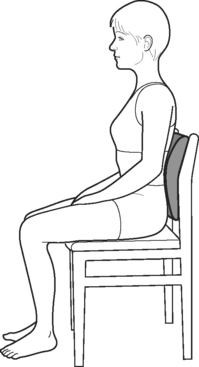
Figure 1.12 A backrest or cushion behind your low back helps to straighten it.
Redrawn with permission from Oliver (1999).
Assessment of forward bending
Normal
To progress forward bending, the lumbar spine continues to reduce its lordosis until the curve has just flattened. Once this has occurred, hip flexion continues the motion to the end of the range of forward bending. Ideally, the alignment at that stage should have remained balanced over the feet with the knees passively extended and with no exaggerated swaying back at the ankles, knees or hips. The hips will then be flexed by approximately 70–80 degrees, the lumbar spine just flattened and the thoracic spine forming a lengthened, gentle and smooth curve (Palastanga et al 2002, p. 58).
Variations in alignment at the end of forward bending
 Limited hip flexion causing lower thoracic spine flexion with a backwards sway of the hips, as may occur in individuals with a trunk that is long in relation to the lower limbs.
Limited hip flexion causing lower thoracic spine flexion with a backwards sway of the hips, as may occur in individuals with a trunk that is long in relation to the lower limbs. Normal hip flexion (70–80 degrees) with a flattened lumbar spine but with excessive thoracic flexion, as may occur in individuals with impaired segmental spine mobility.
Normal hip flexion (70–80 degrees) with a flattened lumbar spine but with excessive thoracic flexion, as may occur in individuals with impaired segmental spine mobility. Normal hip flexion but with the lumbar spine curve being actually reversed as opposed to only flattened, as may occur in individuals with a trunk that is short in relation to their lower limbs.
Normal hip flexion but with the lumbar spine curve being actually reversed as opposed to only flattened, as may occur in individuals with a trunk that is short in relation to their lower limbs. Limited hip and spine flexion and with an exaggerated swaying back of the ankles, knees and hips, as may occur in individuals with restricted spine mobility and short or tight calf musculature, particularly gastrocnemius.
Limited hip and spine flexion and with an exaggerated swaying back of the ankles, knees and hips, as may occur in individuals with restricted spine mobility and short or tight calf musculature, particularly gastrocnemius. Excessive lumbar flexion, as may occur in individuals with a flat back posture. The normal range of lumbar flexion is no more than approximately 50 degrees, and when moving into flexion from the normal lordotic position the first 20–35 degrees will only bring the lumbar spine into a neutral position, thereby allowing a further 15–20 degrees of lumbar flexion during forward bending. When an individual with a flat back posture flexes the lumbar spine from a neutral position, 50 degrees of lumbar flexion can still occur during forward bending. This could allow the lumbar spine a degree of flexion outside its safe anatomical range which might damage ligaments and other soft supporting structures at the back of the spine.
Excessive lumbar flexion, as may occur in individuals with a flat back posture. The normal range of lumbar flexion is no more than approximately 50 degrees, and when moving into flexion from the normal lordotic position the first 20–35 degrees will only bring the lumbar spine into a neutral position, thereby allowing a further 15–20 degrees of lumbar flexion during forward bending. When an individual with a flat back posture flexes the lumbar spine from a neutral position, 50 degrees of lumbar flexion can still occur during forward bending. This could allow the lumbar spine a degree of flexion outside its safe anatomical range which might damage ligaments and other soft supporting structures at the back of the spine.Assessment of return from forward bending
Normal
When returning from forward bending the initial part of the motion is hip extension, and then the hips and spine extend concurrently and smoothly, with the vertebral segments mobilizing in sequence to return to the upright position. A correct movement pattern demonstrates combined lumbar spine and hip extension, and, as the hips have the greatest overall range of movement, they can be seen to move the most. Once the upright position is achieved, the normal spinal curves are re-established to balance the body correctly over the lower limbs and feet (Palastanga et al 2002, p. 60).
Common faults in movement sequencing during flexion and return from flexion
During flexion:
 More than 50% of the total range of lumbar flexion occurring before the initiation of hip flexion occurs in individuals with excessive lumbar spine mobility and restricted segmental movement in other areas of the spine and who commonly have associated low back pain.
More than 50% of the total range of lumbar flexion occurring before the initiation of hip flexion occurs in individuals with excessive lumbar spine mobility and restricted segmental movement in other areas of the spine and who commonly have associated low back pain. Failure of each segment of the vertebral column to contribute its optimum range of movement can be found in individuals with exaggerated spinal curves or where pathology or pain limits overall mobility. Some segments may then become hypermobile whilst others become correspondingly hypomobile.
Failure of each segment of the vertebral column to contribute its optimum range of movement can be found in individuals with exaggerated spinal curves or where pathology or pain limits overall mobility. Some segments may then become hypermobile whilst others become correspondingly hypomobile. Lumbar flexion greater than 25–30 degrees at the end of forward flexion is a feature in some individuals with low back pain associated with excessive lumbar spine mobility and restricted movement in other areas of the spine.
Lumbar flexion greater than 25–30 degrees at the end of forward flexion is a feature in some individuals with low back pain associated with excessive lumbar spine mobility and restricted movement in other areas of the spine. An exaggerated swaying back of the hips and ankles with restricted hip and spine flexion, as may be associated with calf muscle tightness and reduced spine mobility.
An exaggerated swaying back of the hips and ankles with restricted hip and spine flexion, as may be associated with calf muscle tightness and reduced spine mobility.During return from flexion:
 The motion initiates in, or is confined more to, the lumbar spine soon after the hips begin to extend, as may occur in individuals who have low back pain caused by extension, or who habitually use the lumbar spine rather the hips when performing everyday activities.
The motion initiates in, or is confined more to, the lumbar spine soon after the hips begin to extend, as may occur in individuals who have low back pain caused by extension, or who habitually use the lumbar spine rather the hips when performing everyday activities. During the motion the hips and ankles sway forwards markedly to reduce the load on the hips as found in those with swayback posture and weak hip flexors.
During the motion the hips and ankles sway forwards markedly to reduce the load on the hips as found in those with swayback posture and weak hip flexors. The motion initiates in and remains confined more to the hips with minimal spine mobilization as found in individuals such as gymnasts who repeatedly hyperextend the lumbar spine and who possibly have strong, tight anterior abdominal wall muscles that may limit thoracic spine mobility.
The motion initiates in and remains confined more to the hips with minimal spine mobilization as found in individuals such as gymnasts who repeatedly hyperextend the lumbar spine and who possibly have strong, tight anterior abdominal wall muscles that may limit thoracic spine mobility. Failure of each segment of the vertebral column to contribute its optimum range of movement can be found in individuals with exaggerated spinal curves or where pathology or pain limits overall mobility. Some segments may then become hypermobile whilst others become correspondingly hypomobile. This can contribute to low back pain.
Failure of each segment of the vertebral column to contribute its optimum range of movement can be found in individuals with exaggerated spinal curves or where pathology or pain limits overall mobility. Some segments may then become hypermobile whilst others become correspondingly hypomobile. This can contribute to low back pain.Assessment of lateral flexion or side bending
Normal
The total range of side bending motion may be greater than 75 degrees depending on the number of mobile thoracic spine segments involved. Movement occurs most freely in the lower segments of the thoracic spine (approximately 8–10 degrees per segment) where the ribs do not restrict side bending. In the other thoracic and the lumbar spine segments side bending is comparatively restricted (approximately 6 degrees per segment) but fairly evenly distributed between them; however, at the lumbosacral junction only about 3 degrees of lateral movement is possible.
Observable faults during the side bending motion
During side bending to the right:
 Failure of each segment of the vertebral column to contribute its optimum range of movement can be found in individuals with exaggerated spinal curves or where pathology or pain limits overall mobility. Some segments may then become hypermobile whilst others become correspondingly hypomobile. This can contribute to low back pain.
Failure of each segment of the vertebral column to contribute its optimum range of movement can be found in individuals with exaggerated spinal curves or where pathology or pain limits overall mobility. Some segments may then become hypermobile whilst others become correspondingly hypomobile. This can contribute to low back pain. Lumbar spine straightness as found in those individuals with very well-developed paraspinal muscles, the stiffness of which might inhibit lumbar vertebral movement, so that during side flexion the lumbar spine remains straight apart from one axis of rotation towards its base at the lumbosacral junction.
Lumbar spine straightness as found in those individuals with very well-developed paraspinal muscles, the stiffness of which might inhibit lumbar vertebral movement, so that during side flexion the lumbar spine remains straight apart from one axis of rotation towards its base at the lumbosacral junction. To assess and correct this, the teacher may support the subject at the level of the iliac crest to stabilize the pelvis before side flexion and then cue for the lower ribs to be drawn in towards the waist on the side of flexion. If the above measures correct the problem, and the lumbar spine then curves during side flexion, the lumbar paraspinal muscles are probably stiff but not necessarily shortened.
To assess and correct this, the teacher may support the subject at the level of the iliac crest to stabilize the pelvis before side flexion and then cue for the lower ribs to be drawn in towards the waist on the side of flexion. If the above measures correct the problem, and the lumbar spine then curves during side flexion, the lumbar paraspinal muscles are probably stiff but not necessarily shortened. Lumbar spine straightness may also result from tensor fasciae latae tightness that may restrict lumbar spine mobility when side bending to the opposite side.
Lumbar spine straightness may also result from tensor fasciae latae tightness that may restrict lumbar spine mobility when side bending to the opposite side. Restricted side bending movement to one side, with comparatively free side bending to the other, can be attributed to the postural rotation of spinal segments occurring in conditions such as scoliosis. Should the spine habitually rotate to the right during side bending, its rotation to the left is limited, so restricting side bending to the right. Conversely, as the spine is already rotated to the right, side bending to the left is relatively free.
Restricted side bending movement to one side, with comparatively free side bending to the other, can be attributed to the postural rotation of spinal segments occurring in conditions such as scoliosis. Should the spine habitually rotate to the right during side bending, its rotation to the left is limited, so restricting side bending to the right. Conversely, as the spine is already rotated to the right, side bending to the left is relatively free.Assessment of spine rotation
The thoracic spine allows approximately 35 degrees of rotation in each direction, the lumbar spine approximately 13 degrees and at the lumbosacral junction there is normally about 5 degrees of motion, making it the most mobile single junction. The thoracic spine is where spine rotation should mostly occur, as the shape and orientation of each thoracic vertebra allow an optimum range of movement for each spinal segment. The lumbar spine and the lumbosacral junction are prone to injuries caused by excessive, repetitive rotary motions with the lumbar spine flexed, and therefore should be comparatively immobile during spine rotation (Tables 1.2 & 1.3).
Table 1.2 Summary of ideal movement during bending forwards and returning from bending forwards
| Movement sequencing into forward bending | Movement sequencing to return from forward flexion |
|---|---|
Table 1.3 Summary of ideal movement during spine lateral flexion and rotation*
| Lateral flexion | Rotation |
|---|---|
* Based on data from Bobath (1978), Larson & Gould (1974), Sahrmann (2002), White 1969, White & Panjabi (1978).
Ideal alignment
Static postural observation from the side
In this position the imaginary plumb line represents the postural line of gravity and facilitates the observation of relative symmetry in the sagittal plane. Beginning with the spine, observe in relation to the plumb line the positions of the head, tips of the shoulders, hip and knee joints, and note unnecessary tension in associated muscles and soft tissue (Figs 1.13–1.15).
When observing the lower legs and feet, note whether the line of gravity falls approximately through the lateral malleolus as well as the state of the knee joints and leg muscles which should appear comparatively relaxed. Also note the tone and development of the hamstring and gluteal muscles in relation to one another.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree