Chapter 168 Glaucoma
Acute (Angle Closure) and Chronic (Open Angle)
 General Considerations
General Considerations
In the United States, approximately 3 million people have glaucoma, which is undetected in 25% of them.1 The chronic open-angle type, for which there appears to be no consistent anatomic basis, accounts for 70% to 75% of these cases. Histologically, however, there is a strong correlation between the content and composition of collagen and the glaucomatous eye.2
Collagen is the most abundant protein in the body, including the eye. In the eye it provides tensile strength and integrity to the tissues (e.g., cornea, sclera, lamina cribrosa, trabecular meshwork, vitreous). Inborn errors of collagen metabolism (e.g., osteogenesis imperfecta, Ehlers-Danlos syndrome, Marfan syndrome) are often associated with ocular complications: glaucoma, myopia, retinal detachment, ectopia lentis, and blue sclera.3 Morphologic changes in the lamina cribrosa (the scleral area that is pierced by the optic nerve fibers and blood vessels), trabecular meshwork (the connective tissue network through which aqueous humor must pass to reach the canal of Schlemm), and papillary blood vessels in the eye have all been observed in glaucomatous eyes.2,4–6 These changes may result in elevated IOP readings or, perhaps more significantly, lead to the progression of peripheral visual loss. Changes in collagen structure would explain the following2,4–6:
• Similar peripheral vision loss in patients with normal and elevated IOP
• Cupping of the optic disc even at low IOP levels
 Diagnosis
Diagnosis
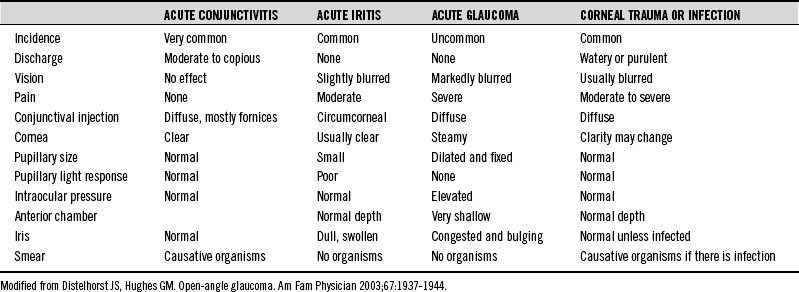
The primary challenge with acute glaucoma is early recognition, because delay in referral for surgical intervention increases the risk of blindness. Table 168-1 provides an overview of the differential diagnosis of the inflamed eye.
 Therapeutic Considerations
Therapeutic Considerations
Corticosteroids
The importance of collagen destruction in the etiology of glaucoma is apparent in corticosteroid-induced glaucoma.2 Corticosteroid use should be discouraged in the glaucoma patient, as it is known to inhibit the biosynthesis of collagen and glycosaminoglycans, thereby worsening the patient’s glaucoma.2
Supplements and Diet
Vitamin C
Of foremost importance in achieving collagen integrity are optimal tissue concentrations of ascorbic acid (AA). Furthermore, AA has been demonstrated to lower IOP levels in many clinical studies.7–11 A daily dose of 0.5 g/kg, whether in single or divided doses, reduces the IOP by an average of 16 mm Hg.11 Near normal tension levels were achieved in some patients unresponsive to acetazolamide (a carbonic anhydrase inhibitor) and 2% pilocarpine (a miotic agent).11
The hypotonic action of AA on the eye is long-lasting if supplementation is continued, and intravenous administration results in an even greater initial reduction in IOP.7,9–11 The patient must be monitored to determine the appropriate individual dose, because some patients respond to as little as 2 g/day, whereas others will respond only to extremely high doses (e.g., 35 g/day).7–11 Abdominal discomfort as a side effect of high doses is common but usually resolves after 3 to 4 days.11
The proposed mechanisms by which AA lowers IOP include the following:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree