3 Gentian Violet Treatment of Severe Chronic Paronychia
3.1 Introduction
Chronic paronychia is most commonly caused by Staphylococcus aureus and Candida albicans and is thought to be due to bits of nail beneath the eponychium, which act as a foreign body. Since the new millennium, the most common bacteria found in hand infection is methicillin-resistant S. aureus (MRSA).
Early gentian violet study by Churchman in 1912 showed gram-positive organisms (especially S. aureus) to be highly susceptible to gentian violet dye, even at marked dilution, and it was the antimicrobial treatment of choice until penicillin became popular after 1943. It has long been a favored treatment for thrush (C. albicans) as recommended by the World Health Organization. There is no report of resistant Staphylococcus to gentian violet dye, thought to be due to the dye’s penetration of the bacterial cell wall and the mitochondrial membrane (thus, most gram-positive organisms are susceptible), obviating opportunity to mutate into a resistant form.
Though most surgery texts recommend one of two surgical approaches for chronic paronychia, either marsupialization or resecting the proximal nail, these have significant morbidity and often have recurrence. Topical application of the simple, inexpensive over-the-counter gentian violet treatment should be attempted. This treatment has successfully managed MRSA infections of femoral prostheses, decubitus ulcers, chronic otitis, empyema, and skin ulcerations.
Typically, we instruct our patients to topically apply 1 or 2% gentian violet liquid dye directly along the inflamed eponychium once or twice a day until it is no longer painful, usually 3 to 7 days, unless the patient has Raynaud’s syndrome. In those patients, once-a-day application may be necessary for 2 to 3 weeks, because they heal so slowly. Thereafter, no further treatment is required. No antibiotics are utilized and the patient knows how to manage a recurrence or if another digit becomes involved. Additional digital involvement is frequent among the patients who have Raynaud’s syndrome and scleroderma.
The author has not operated on a patient with chronic paronychia in over 30 years. Two cases are presented here to show how this noninvasive approach can help the patient avoid surgery.
3.2 Patient History Leading to the Specific Problem: Case A
This 80-year-old woman was referred by infectious disease with a request for index digit amputation. While she was in a nursing home, she developed an MRSA-infected gouty tophus of her index digit, which then led to mid-face cellulitis and MRSA sepsis. She was hospitalized, responded to intravenous (IV) vancomycin, and was discharged on oral clindamycin, but referred a month after onset with request for index amputation for recalcitrant MRSA finger infection.
3.3 Anatomic Description of the Patient’s Current Status: Case A
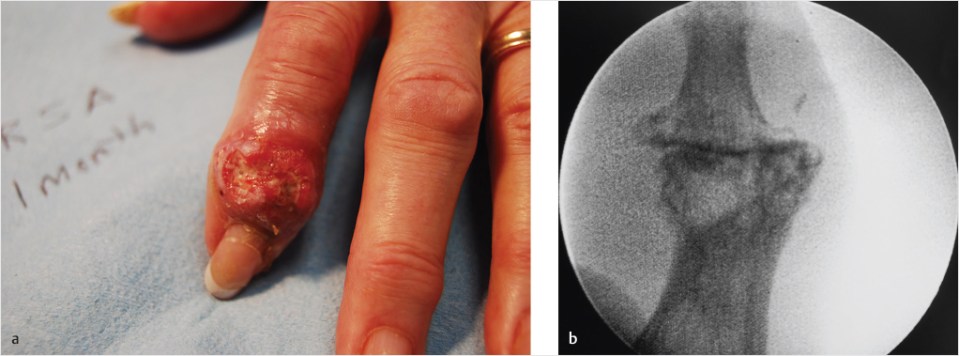
Initial examination findings showed the patient to be weak, faint and pale, and obviously dehydrated, with a chief complaint of diarrhea and a secondary complaint of a painful index digit. Her X-ray had changes of gout, although osteomyelitis was mentioned as a possibility (▶Fig. 3.1).
Fig. 3.1 (a, b) One month after infected gouty tophus with MRSA (methicillin-resistant Staphylococcus aureus).
3.4 Recommended Solution to the Problem: Case A
Although referred for amputation, unless there was osteomyelitis, gentian violet dye should adequately control the MRSA infection, and clindamycin discontinued due to the troublesome side effects.
3.5 Technique: Case A
This patient was given an initial treatment of 2% gentian violet dye topically in the office, told to stop taking clindamycin, and then sent to the emergency department where she was given IV fluids and loperamide (Imodium). She returned to the office in 2 days and said this was less painful, and was again treated with topical gentian violet. At 4 days on return, she stated she was pain free, and dye was reapplied with a return appointment scheduled (▶Fig. 3.2).
3.6 Postoperative Photographs and Critical Evaluation of Results: Case A
The patient did not return for her scheduled follow-up. Calls to the skilled nursing facility where she resided assured us she was well, but she continued to cancel her return appointments. Finally, the surgeon went to the facility to visit her, and she was found to be well healed, explaining that she did not return because she was told “the surgeon might cut your finger off” and it was no longer bothering her. She has had no recurrence (▶Fig. 3.3).