Male Genital Trauma in Sports
Stanley R. Hunter, MDa, Timothy S. Lishnak, MD, CAQSMb, Andria M. Powers, MDc and David K. Lisle, MD, CAQSMbd∗
aMilton Family Practice, Department of Family Medicine, University of Vermont College of Medicine, 111 Colchester Avenue, Burlington, VT 05401, USA. E-mail address: David.Lisle@vtmednet.org
Keywords
Testicular hemotoma
Rupture
Urethral injury
Urethrogram
Scrotal hematocele
Background and mechanisms
Male genital trauma is a rare but potentially serious sports injury. Although such an injury can occur by many different mechanisms, including falls, collisions, straddle injuries, kicks, and equipment malfunction, the clinical presentation is typically homogeneous, characterized by pain and swelling. Almost all sports-related male genital injury comes from blunt force trauma, with involvement of scrotal structures far more common than penile structures.1 Most injuries can be treated conservatively, but catastrophic testicular injury must first be ruled out. Despite being relatively uncommon compared with other sports injuries, more than half of all testicular injuries are sustained during sports.1 Ninety percent of blunt testicular injuries are isolated; 5% are associated with penile injury, and less than 2% are bilateral.2
Blunt trauma with suspected testicular rupture
Testicular rupture is characterized by rupture of the tunica albuginea and extravasation of seminiferous tubules.1 Severity may vary from a small laceration with minimal extravasation to complete parenchymal destruction.3 The mechanism is usually via a direct blow with compression of the scrotum against the pelvis or thigh.3 According to a 1946 case report, approximately 50 kg compression is required to cause rupture, although this number is not substantiated or referenced.4 This force is likely less in the setting of tumor or other structural compromise, leading to the possibility of uncovering an underlying condition from trauma.3
Testicular mobility, the cremasteric reflex, and the strength of the tunica albuginea all contribute to making testicular rupture uncommon.2 Most male genital injuries from sports are minor contusions that resolve without treatment.1
Clinical History
Presenting symptoms include severe pain, nausea, emesis, and sometimes syncope.3 Usually the time and mechanism of trauma are obvious. When a patient presents late, a history of improvement of symptoms does not rule out rupture. Pain will improve gradually, even with untreated testicular rupture.3
Physical Examination and Testing
The goal of the physical examination and adjunctive testing is to separate those injuries requiring surgical exploration from those that may be treated conservatively. An examination may be difficult due to the presence of pain and swelling, but the location of swelling can have prognostic value. One set of authors describes an examination technique of grasping the neck of the scrotum with 3 fingers posterosuperiorly to the involved testis and the thumb anteriorly. Swelling below the thumb implicates testicular injury, epididymal injury, or hydrocele. Swelling above thumb implicates incarcerated hernia or spermatic cord injury.5
Swelling, ecchymosis, and tenderness to palpation are typically appreciated on examination.1 A hemiscrotal hematocele is often apparent as a tender mass larger than a baseball and causing loss of rugae of the scrotal skin. Such a hematocele is common in association with testicular rupture and will not transilluminate.3
Imaging
Adjunctive imaging is valuable due to poor specificity of examination findings and the necessity for a low threshold for surgical exploration in suspected testicular injury. An ultrasound scan of 7.5 to 10 MHz with a linear array transducer became a standard in the evaluation of testicular trauma in the mid 1980s.2,6 Doppler ultrasound studies can evaluate perfusion of a jeopardized testicle.7 Although several studies report discordant results about the utility of ultrasound in diagnosing intrascrotal injuries, some of the discrepancy seems to be due to changes and improvements in ultrasound technology in the last 25 years. One 2008 French study performed retrospectively on a series of patients compiled sensitivity and specificity estimates for ultrasound of various types of intrascrotal injury.8 All patients in this study underwent both ultrasound and the diagnostic gold standard of surgical exploration (Table 1).
Table 1
Accuracy of ultrasonography for blunt scrotal trauma
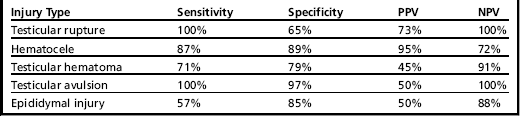
Data from Guichard G, El Ammari J, Del Coro C, et al. Accuracy of ultrasonography in diagnosis of testicular rupture after blunt scrotal trauma. Urology 2008;71(1):52–6.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








