Abstract
Background
The dynamics behavior of patients with idiopathic scoliosis obviously requires some biomechanical compensatory strategies. Our objective is to analyze the ground reaction forces (GRF) exerted during gait initiation in order to determine the dynamic consequences of idiopathic scoliosis.
Methods
Ten adolescent girls suffering from idiopathic scoliosis with a right thoracic curvature (Cobb > 15°) and 15 healthy adolescents participated in this study. Two force plates were used to record the ground force evolution for the right and left limbs tested during gait initiation.
Results
Whichever limb was used to initiate gait, gait initiation duration was found to be significantly longer in persons with scoliosis than in healthy subjects. In the scoliosis group (SG), the impulses, occurrences and forces values were also greater than in healthy subjects. Under the stance foot, the anteroposterior and vertical forces were always increased. Under the swing foot, the SG showed the same characteristics associated to decreased mediolateral impulses parameters. Even greater differences were observed between these two groups in terms of peak occurrences during left-limb gait initiation. The intragroup comparisons only unveiled very few differences between the two limbs for the control group (CG), whereas significantly higher values were recorded for the group of scoliosis patients when gait was initiated with the left limb rather than with the right one.
Conclusion
For patients with scoliosis specific dynamic behavior adjustment are made during gait initiation patterns, for both limbs in order to maintain balance during gait to compensate for their spine deformation. Patients with scoliosis always showed slower dynamic patterns than healthy controls. These results show the importance of including specific evaluation and dynamic physical rehabilitation for patients with idiopathic scoliosis.
Résumé
Objectif
La scoliose idiopathique induit une réorganisation du comportement dynamique du patient. Notre objectif est d’analyser les conséquences de la déformation rachidienne sur l’initiation de la marche via l’évolution des forces de réaction du sol.
Patients et méthode
Dix adolescentes présentant une scoliose idiopathique thoracique droite (Cobb > 15°) et 15 sujets témoins ont participé à cette étude. Deux plateformes de forces ont permis d’enregistrer l’évolution de la force de réaction du sol au cours de la réalisation d’une initiation de la marche (pas initiés par les membres inférieurs droit et gauche).
Résultats
Pour l’ensemble des tests, la durée de l’initiation du pas était significativement augmentée pour les patients par rapport aux sujets témoins. La scoliose idiopathique induit lors de l’initiation du pas une augmentation des impulsions, des occurrences et des amplitudes de la force de réaction du sol. Sous le pied d’appui, c’est principalement les composantes verticales et antéropostérieures qui sont les plus perturbées. Sous le pied initiant le mouvement, ces mêmes caractéristiques ont pu être observées, mais, elles sont associées à une diminution des impulsions pour la force médiolatérale. Les différences entre les groupes sont particulièrement visibles lorsque le mouvement est initié par le membre du côté concave (gauche). Pour le groupe de patient, l’initiation par ce même côté induit une augmentation systématique de tous les paramètres par rapport à l’initiation du côté droit. Peu de différences ont pu être mises en évidence entre les côtés pour le groupe de sujets témoins.
Conclusion
La scoliose idiopathique induit le développement de stratégies adaptatives lors de l’initiation de la marche, caractérisées par un ralentissement du mouvement et une asymétrie comportementale entre les pas du côté de la convexité et du côté de la concavité. Ces résultats montrent l’importance d’inclure une évaluation et une rééducation lors du mouvement pour les patientes présentant une scoliose idiopathique.
1
English version
1.1
Introduction
Gait initiation is defined as the transition phase between standing and gait . To start walking, muscular and gravitational actions are required to create the initial posture dynamic condition for moving forward . Thus, gait initiation starts by a backward displacement of the center of pressure (CP) towards the leading limb initiating the movement whereas the center of gravity moves forward towards the stance limb . This center of gravity/CP de-coupling generates the best conditions required for gait initiation . Two factors may influence gait velocity: the length of the anticipatory posture adjustments phase , and the initial position of the person’s center of gravity .
The invariant characteristics of gait initiation result from the interdependence of biomechanical parameters (position of the CP and the center of gravity) and time/distance parameters (stride length, time to start, duration time and velocity) .
Some asymmetric pathology affecting the lower limbs (knee osteoarthritis, congenital talipes equinovarus-clubfoot, hemiplegia) also influence gait initiation through spatiotemporal adaptation of the kinetics and kinematics parameters but also with the onset of dynamic asymmetries . Actually, no asymmetric spinal cord pathology has been tested during gait initiation, even though we believe that the balance mechanisms involve the trunk, as it was reported during gait .
Studies focusing on gait and posture unveiled some posture dynamic characteristics specific to adolescent idiopathic scoliosis (AIS) . This pathology is characterized by a three-dimensional spine deformation (lateral curvature, decreased sagittal curvature and rib hump) that progresses particularly during adolescence . Despite the latest scientific advances and numerous studies on this pathology, AIS remains an etiological enigma. The answer is most probably an interaction between all these hypotheses . Thus, a defective gene could trigger a disorder in melatonin synthesis that would lead to a temporary dysfunction of the nervous system during the child’s growth including vision , proprioceptive and vestibular disorders . These disorders could be at the source of posture imbalance and compensatory mechanisms used by AIS patients during standing and gait. . Very recently, it has been proven that kinetics’ analysis is more reliable than kinematics’ analysis in order to define the posture dynamics behavior of patients affected by AIS .
In a standing position, AIS triggers an increase in the amplitude of posture-induced oscillations and a shifting of the CP compared to control subjects . Spine deformation changes the relationship between the position of the various body parts (spinal cord and limbs), thus requiring new strategies to achieve and maintain balance control . Two factors of instability were identified in AIS patients:
- •
single curve scoliosis ;
- •
ectomorphic body morphology type (tall and lanky) .
The analysis of lateral stepping and forward stepping unveiled a displacement of the CP increased in AIS patients compared to control subjects, associated to an asymmetry in terms of ground reaction forces (GRF) . During gait, AIS involves spatiotemporal GRF disruption mainly characterized by an increased asymmetry of the lower limbs and an increased variability of the dynamics parameters .
In light of the importance of spatiotemporal disruptions observed during posture and gait, it seemed necessary to define the transition between these two stages (stand to walk) . The displacement of the center of gravity correlated to the spine deformation should mainly impact the strategies and velocity of gait initiation . We could bring up the hypothesis that a three-dimensional asymmetric spine deformation related to disruptions of the sensory systems could generate different kinds of management strategies between AIS patients and control subjects, but also between the steps initiated on the convex side and concave side of the deformity . Such compensatory strategies secondary to the scoliosis pathologies should be more visible on the orthogonal component of the movement direction, since the latter was described as the one most controlled during movement .
The aim of the study was to define adaptive strategies in persons with AIS during gait initiation. We analyzed the pathology’s influence on gait initiation but also the deformation’s influence on the compensatory mechanism of each limb initiating stepping.
1.2
Patients and methods
Twenty-five young adolescent girls participated in the study; 15 of them made up the control group (CG) and the other 10 were in the scoliosis group (SG). Both groups were paired in age (SG: 13.8 ± 2.15 vs 12.57 ± 1.34 for CG), in height (SG: 1.6 ± 0.09 vs 1.55 ± 0.073), and body mass (for the SG: 49,17 ± 8,89 vs 47.55 ± 9.83 for the CG, Table 1 ).
| Patients with right thoracic curve | ||||
|---|---|---|---|---|
| Age | Height | Weight | Cobb | |
| S4 | 11 | 1,4 | 33,02 | 20 |
| S5 | 12 | 1,6 | 47,82 | 57 |
| S6 | 12 | 1,61 | 46,54 | 20 |
| S7 | 13 | 1,61 | 43,98 | 18 |
| S9 | 16 | 1,58 | 55,94 | 33 |
| S11 | 15 | 1,7 | 54,09 | 24 |
| S13 | 18 | 1,68 | 57,18 | 31 |
| S14 | 13 | 1,53 | 41,16 | 17 |
| S15 | 13 | 1,56 | 45,97 | 78 |
| S16 | 15 | 1,72 | 66,04 | 36 |
| Mean | 13,8 | 1,60 | 49,17 | 33,4 |
| Standard deviation | 2,15 | 0,09 | 8,89 | 18,74 |
| Healthy subjects | ||||
|---|---|---|---|---|
| C2 | 13 | 1,62 | 51,81 | |
| C3 | 13 | 1,58 | 56,08 | |
| C4 | 11 | 1,5 | 40,99 | |
| C5 | 11 | 1,55 | 42,13 | |
| C6 | 11 | 1,63 | 68,18 | |
| C7 | 11 | 1,52 | 50,24 | |
| C8 | 12 | 1,44 | 37,29 | |
| C9 | 11 | 1,45 | 36,72 | |
| C10 | 12 | 1,59 | 39,64 | |
| C11 | 13 | 1,42 | 31,19 | |
| C12 | 14 | 1,6 | 48,82 | |
| C13 | 14 | 1,66 | 60,78 | |
| C14 | 14 | 1,61 | 51,06 | |
| C15 | 14,5 | 1,58 | 51,24 | |
| C16 | 14 | 1,57 | 47,04 | |
| Mean | 12,57 | 1,55 | 47,55 | |
| Standard deviation | 1,348 | 0,073 | 9,826 | |
The control subjects were recruited in several different middle schools (Junior High) after obtaining the requisite administrative agreements. The AIS patients were recruited in the pediatrics orthopedic unit of the hospital La Timone (Hôpital de la Timone, Marseille, Pr. G. Bollini’s unit). Only AIS patients with right thoracic scoliosis (Cobb < 15°) and a dominant ectomorphic morphology type (90%) were included in the protocol. These two characteristics were found to induce maximal disruptions of posture dynamics in .
All subjects and their legal guardians were given detailed information and we collected their signed informed consent to participate in the study. The local ethical committee also gave their agreement (ID RCB: 2006-A00289-42). The participation in this study was on a voluntary basis and patients were free to quit the experimental protocol at any time. Recorded data remained strictly confidential.
The initial medical exam was performed by a surgeon specialized in spinal cord surgery and scoliosis pathology. A detailed overview of the pathological history unveiled the context of onset of this pathology (family medical history, personal history, initial discovery date of the pathological process, former treatments…). Then, X-ray imagings coupled to a clinical exam were done in order to assess the Cobb angle, Risser Test, gibbosity, and pelvic and scapular girdles balance. Each AIS patient presented a single curvature (non-compensated scoliosis) with a ≥ 18 °Cobb angle (33.4° ± 18.74 average), and a 16-mm mean gibbosity (5 mm minimum and 27 mm maximum), and a Risser test evaluated on average at 3.1 (1 mm minimum, and 4 mm maximum). Out of the group of 10 young girls, only two of them achieved a horizontal balance of both girdles in the coronal plane. However, no length disparity was reported for the lower limbs. Each patient followed a treatment with an orthotic brace (treatment average 8 months ± 3), but none of the patient had surgery for his or her AIS.
Regarding the control subjects, a detailed screening was also done (family and individual medical history) to limit potential pathological biases in the study (scoliosis, length disparity, orthopedics pathologies of the lower limbs, neurological, mental or sensory pathologies).
All subjects were tested for foot laterality (dominant and non-dominant limb) by a posterior push resulting in a forward stepping with the dominant foot. All participants had right foot laterality. In light of that fact, in the results part of this study, we will talk about right or left limb rather than dominant or not dominant for an easier read. All tests were conducted while patients were not wearing an orthotic brace despite of the brace seems not to have influence on the standing balance .
The experiment took place in a room dedicated to movement analysis using two force plates inserted into the ground (AMTI ® , BP6001200 ). The acquisition frequency for the GRF was set at 100 Hz . Initially, the subject was asked to stand up spontaneously with a foot positioned on each force plate. The “stance” force plate corresponded to the stance foot and the “swing” force plate was the one located under the foot starting the movement. At the signal (go), the subject performed two series of five successive gait initiations while the examiner was indicating the side of the initiation at the very last moment and in a random order.
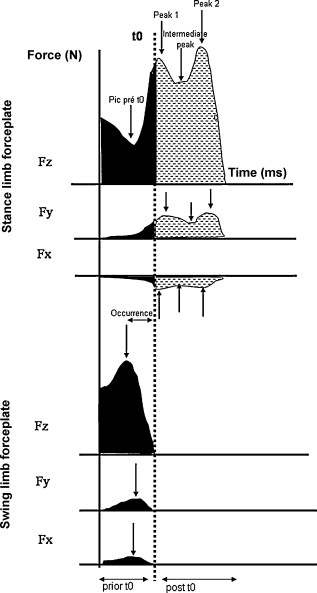
The data processing analysis of the three GRF components (anteroposterior–Fy, mediolateral–Fx and vertical–Fz) was done with MATLAB™ v.6 and Mathworks™ . The analysis was subdivided into various successive steps to extract the time distance parameters for the GRF ( Fig. 1 ):
- •
normalization of the amplitudes of the forces signals according to each subject’s mass;
- •
identification of “t0” (moment in time corresponding to the lift of the foot initiating the movement);
- •
computation of the area under the curve (force × time) for impulse measurement;
- •
identification and extraction of the peaks of the forces values (force values [N] and occurrences [ms]) to characterize the force pattern of the gait initiation for the control subjects. The force value corresponds to the amplitude of the force displacement and occurrence corresponds to the time when such a peak appeared in regards to “t0”.
For each computed parameter, the normality of the data dispersion was tested using the Shapiro-Wilk test. The statistical validity of the hypothesis was tested using Anova (Statistica™, v.6, Statsoft™). The value p < 0.05 was considered the threshold to reject the null hypothesis. Finally, analysis of the a-posteriori interactions between variables was done using the Newman-Keuls test for specific effects.
1.3
Results
1.3.1
Duration of step initiation
Regardless of the step-initiating side, scoliosis patients required a significantly longer time to achieve the entire total movement (in terms of all three components) compared to the CG ( Fig. 2 ). More specifically, the SG showed a significantly increased duration for mediolateral component (6% for the right side, p < 0.0004; 9% for the left side, p < 0.002), anteroposterior component (3% for the right side, p < 0.01; 2% for the left side, non significant) and vertical component (2% for the right side, non significant; 9% for the left side, p < 0.0002). No differences in movement duration between the right and left side were reported in the SG. For the CG, the difference between right and left sides was only significant for the anteroposterior component (right side: 824 ms ± 126; left side: 866 ± 131, p < 0.043).

1.3.2
The Stance limb force plate
The intergroup impulse comparisons showed significant differences only for the vertical component data ( Fig. 3 ). The SG systematically produced larger impulses than the healthy group prior to t0 (i.e. prior to the single foot stance phase) (right side: CG: 19,109 Nms ± 4987 vs SG: 22,232 Nms ± 11,667, p < 0.01; left side: CG: 18,599 Nms ± 5813 vs SG: 22,436 Nms ± 11,560, p < 0.008) and after t0 (right side: CG: 50,881 Nms ± 7169 vs SG: 60,451 Nms ± 21,719, p < 0.0003; left side: CG: 51,360 Nms ± 8793 vs SG: 58,966 Nms ± 19,218, p < 0.002).

The occurrence data allowed for differentiating the two groups for all three components of the GRF ( Table 2 ).
| F x | F y | F z | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Healthy | AIS | p | Healthy | AIS | p | Healthy | AIS | p | ||
| Peak 1 | R | 42 ± 35 | 53 ± 51 | NS | 84 ± 54 | 57 ± 37 | *** | 39 ± 14 | 38 ± 15 | NS |
| L | 37 ± 27 | 49 ± 48 | NS | 88 ± 55 | 86 ± 57 | NS | 40 ± 18 | 51 ± 31 | *** | |
| P | NS | NS | NS | *** | NS | *** | ||||
| Intermedial peak | R | 167 ± 56 | 184 ± 85 | NS | 262 ± 80 | 228 ± 86 | ** | 157 ± 32 | 159 ± 52 | NS |
| L | 171 ± 68 | 180 ± 84 | NS | 234 ± 90 | 232 ± 76 | NS | 171 ± 59 | 170 ± 54 | NS | |
| P | NS | NS | ** | ** | NS | NS | ||||
| Peak 2 | R | 355 ± 62 | 405 ± 72 | *** | 436 ± 68 | 475 ± 57 | *** | 380 ± 60 | 401 ± 69 | NS |
| L | 382 ± 79 | 383 ± 71 | NS | 445 ± 71 | 465 ± 42 | NS | 390 ± 72 | 393 ± 46 | NS | |
| P | ** | ** | NS | NS | NS | NS | ||||
In the case of mediolateral force, comparison between groups showed significant differences only for peak 2 when the step was initiated by the right side ( Table 2 ). With the anteroposterior force, on that same side, scoliosis patients showed lower peak 1 and intermediate peak values, and higher peak 2 value in terms of timing ( Table 2 ) and amplitudes (Peak 1: CG: 145 N ± 38 vs SG: 127 N ± 53, p < 0.029/intermediate peak: CG: 113 N ± 34 vs SG: 100 N ± 44, p < 0.018/Peak 2: CG: 201 N ± 43 vs SG: 221 ± 93, p < 0.05). For the vertical force, regardless of the side initiating the movement, scoliosis patients, compared to healthy subjects, showed increased occurrences values during the pre-t0 phase (right side: CG: −209 ms ± 44 vs SG: −234 ms ± 57, p < 0.003/left side: CG: −207 ms ± 56 vs SG: −256 ms ± 70, p < 0.0006) as well as for peak 1 during left-side step initiation ( Table 3 ). No differences between groups were observed in the Fz amplitudes during the pre-peak phase, contrary to what occurred during the post-peak phase. For the post-t0 phase and when the step was initiated with the left limb, scoliosis patients systematically showed higher Fz values (Peak 1: CG: 1069 N ± 100 vs SG: 1175 N ± 360, p < 0.002/Intermediate peak: CG: 914 N ± 99 vs SG: 1032 N ± 306, p < 0.0001/Peak 2: CG: 1141 N ± 107 vs SG: 1242 N ± 392, p < 0.006), whereas when the step was initiated with the right side, these patients only showed an increase in peak 1 and intermediate peak values (peak 1: CG: 1062.41 N ± 78.43 vs SG: 1165.51 N ± 278.90, p < 0.007/Intermediate peak: CG: 909.87 N ± 82.11 vs SG: 1016.99 N ± 232.09, p < 0.0009).
| F x | F y | F z | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Healthy | AIS | p | Healthy | AIS | p | Healthy | AIS | p | ||
| Impulses | R | 2079 ± 608 | 1746 ± 638 | *** | 1318 ± 599 | 1530 ± 679 | ** | 21 446 ± 6408 | 27 463 ± 10 918 | *** |
| L | 1845 ± 491 | 1726 ± 454 | NS | 1284 ± 541 | 1684 ± 844 | *** | 21 227 ± 5585 | 31 187 ± 14 390 | *** | |
| p | ** | NS | NS | NS | NS | *** | ||||
| Occurrences | R | −181.78 ± 49 | −191.62 ± 53 | NS | −134.38 ± 54 | −146.04 ± 50 | NS | −211.37 ± 52 | −226.28 ± 52 | NS |
| L | −175.40 ± 52 | −214.3 ±1 26 | *** | −135.32 ± 53 | −175.40 ± 97 | *** | −206.95 ± 58 | −256.37 ± 66 | *** | |
| p | NS | *** | NS | *** | NS | *** | ||||
| Amplitude | R | 78.00 ± 17 | 57.21 ± 19 | *** | 59.02 ± 23 | 61.80 ± 22 | NS | 715.03 ± 117 | 778.46 ± 218 | ** |
| L | 74.45 ± 18 | 52.43 ± 12 | *** | 59.52 ± 22 | 64.67 ± 26 | NS | 719.46 ± 126 | 805.13 ± 248 | *** | |
| p | ** | ND | NS | NS | NS | NS | ||||
For the CG, the comparison between right side and left-side initiations showed a significant increase in the peak occurrences when the step was initiated on the left side for the mediolateral (peak 2, Table 2 ) and anteroposterior forces (intermediate peak, Table 2 ). For scoliosis patients, when the step was initiated on the left side, there was an increase of the occurrence values for peak 1 (anteroposterior and vertical forces), intermediate peak (anteroposterior force) and a decrease of occurrences values for peak 2 (mediolateral force, Table 2 ). For this same group, the anteroposterior amplitudes were larger when stepping was initiated on the left side in terms of peak 1 (right: 127 N ± 53 vs left: 144 N ± 55, p < 0.04) and intermediate peak (right: 100 N ± 44 vs left: 115 N ± 42, p < 0.04).
1.3.3
The swing limb force plate
Data recorded for the swing limb force plate are listed in Table 3 .
For impulses, the intergroup comparison unveiled a significant difference regardless of the side initiating the step.
The patients showed significantly higher anteroposterior and vertical impulses as well as a decreased of lower mediolateral impulses ( Table 3 ). The comparisons between the left and right side clearly highlighted significant differences for scoliosis patients on vertical component impulses of the GRF (the values recorded on the left side were greater than the ones on the right side). For control subjects, the computed impulses of the mediolateral force allowed for differentiating the initiation sides (the values recorded on the right side were greater than the ones on the left side).
When the step was initiated on the left side, the SG showed significant increased in occurrences values, versus the CG, for each GRF component. Intragroup comparison for the SG showed that the left side was characterized by a significant increase in occurrence values (mediolateral, anteroposterior and vertical forces) compared to the right side.
Regardless of the initiating limb, scoliosis patients showed lower mediolateral amplitudes, but significantly increased vertical amplitudes ( Table 3 ) compared to the CG. No significant difference between sides was reported for the SG. However, for the CG, stepping with the right limb was characterized by greater mediolateral amplitude than stepping with the left limb.
1.4
Discussion
Our results revealed compensatory strategies in AIS patients versus control subjects, characterized by the changes in GRF dynamics parameters during gait initiation. These results validate the results found in the literature regarding standing position and gait in AIS patients . During gait initiation, AIS patients produce a slower movement associated to increased impulse values and displacement of the three GRF components. It is systematically the left limb (concave side) that induces an increase of all parameters (impulses, occurrences, amplitudes). For the stance limb force plate, the vertical force is the most disrupted, whereas for the swing limb force plate all three GRF components are affected. Our results associated to those in the literature show that the vertical component of the ground force reaction is a parameter of choice to characterize the dynamics behavior of AIS patients . However, some authors underline that AIS pathology disrupts principally the GRF mediolateral component during gait . These different observations can be explained by movement choice (gait vs gait initiation/standing position) and parameters analyzed, but also by the heterogeneity of the scoliosis population group in most studies . The impact of AIS type on posture dynamics management has been described previously , this is the reason we chose to focus our study on right thoracic curve scoliosis without compensatory curve, since this curvature type induces the most instability . Furthermore, we have chosen specific GRF parameters (impulses, peaks and occurrences) according to dynamic patterns of gait initiation. The study of Fortin et al. showed the relevance and reliability of a detailed kinetic analysis to characterize the compensatory mechanisms of AIS patients as opposed to kinematics analysis.
The left limb/right limb comparison showed that the instability depends on the side initiating the step. When the step is initiated on the right side (convex side), AIS patients adopt a stabilization strategy by decreasing lateral displacement prior to the movement in order to control and direct the force towards the movement. On the other hand, when the step is initiated on the left side (concave side), the spine deformity induces a systematic instability for the movement direction force but also for the balance control force . The consequences of this pathology vary according to the gait initiation side, thus enabling to argue the results showing dynamics asymmetry between both sides during gait and during lateral stepping .
In spite of a large number of studies devoted to the etiology of AIS, very few studies focused on compensatory posture management for these patients that lead very active lives similar to non-pathological young adults. Studies’ results on standing position , lateral stepping and gait suggest that it is currently difficult to ignore the impact of this pathology on postural compensatory strategies during movement. The “strategy or mechanism” term implies more or less a deliberate choice among various available techniques . During simple standing position, the subject develops global posture strategies, on the other hand for a complex movement; the subject will use local reflexes limiting the possibilities of precise compensatory strategies . So, the patients with scoliosis develop specific strategies in a priority aim of postural balance, which are of neurophysiological and biomechanical origins.
To elaborate the movement action and organize balance, subjects perceive and analyze their surrounding environment and adjust their orientation to achieve balance control . Consequently, postural regulation requires integrating some sensory information in order to get the necessary elements for achieving balance control, the latter being a mandatory prerequisite to any action . The vestibular, visual and somatoproprioceptive receptors are involved in the continuous and intermittent balance control . Indeed, AIS pathology has been correlated to sensory , spatial orientation (vertical and horizontal planes) as well as anatomical/physiological modifications . All these disruptions induce a differential context in which the patient must manage his/her balance based on false sensorimotor parameters . Consequently, postural instability observed during standing , gait and step initiation seems to be correlated to modified intrinsic and extrinsic information specific to the scoliosis pathology. Sensory systems are not only disrupted but they also present more asymmetries at cortical integration level . Consequently, motor strategies are different according to the side initiating the movement (right vs left/convex vs concave) during step initiation, with a systematic increase of the spatiotemporal parameters when the left limb on the concave side initiates the step.
Movement production depends on external constraints (environment, ground…) and internal constraints (body mass, muscle physiology, postural balance…) . For internal constraints, besides sensory disorders, some muscular particularities have been associated to AIS. The asymmetry of muscle fiber composition between concave and convex sides could be related to compensatory strategy involving muscles in the lumbar area for AIS patients . However, while one study promotes this hypothesis by an asymmetrical EMG response of paraspinal muscles in a sitting position , another study on gait did not report any asymmetrical EMG response for paraspinal muscles . In the future, additional studies will have to determine the anatomophysiological impact of thoracic back muscles on the compensatory strategies observed during step initiation.
During step initiation, total movement duration is systematically longer for AIS patients than for healthy subjects. This relative slowness can be associated to an increase in electromyography activity , energy production and displacement of GRF and CP during movement . The slowing down of the movement is at its most visible when the task is unusual for the patient . During gait initiation, a usual task, the duration increase depends on the movement’s phase. In fact, AIS induces a decrease of preparatory phase duration (pre-t0) associated to an increase in movement phase duration (post-t0). The intergroup time differences are especially obvious when the step initiation is done with the left limb (concave side). The intragroup comparison for control subjects showed very little differences between the sides initiating the step; whereas in AIS patients, the left side systematically induces an increase of the spatiotemporal parameters (amplitude and occurrences) compared to the right side.
Researches on gait and standing position in AIS patients unveiled the relevance to study the three GRF components . The patients’ compensatory behavior result on one hand from the instability directly linked to this pathology but also the impact of the spine deformity on the sagittal and coronal planes. According to Winter, it is the force perpendicular to the movement that controls its balance . Thus, during stepping, instability could be translated by a disruption of the mediolateral component of the GRF. However, our results show that the most disrupted are the vertical and anteroposterior GRF components (increased impulses, amplitudes and occurrences) as previously demonstrated during gait analysis . Consequently, for the entire movement (stance and swing force plates), the anteroposterior and vertical components are the most relevant parameters to differentiate the groups. The AIS induced biomechanical modifications lead to a preferential control for the pathological group associated to body mass management towards the movement, validating the fact that AIS patient primarily controls kinetic parameters before muscular force. Whereas control subjects, in agreement with Winter , primarily control the balance perpendicular to the movement’s plane. Such dynamics strategies adopted by AIS patients aim to minimize the consequences of the asymmetric displacement of masses secondary to spine deformation by first controlling movement preparation during step initiation. Actually, the peak of movement preparation appears earlier for patients than for the control subjects whereas the total duration remains longer for AIS patients. This simplified strategy can be directly linked to the patients’ incapacity to manage the various degrees of freedom during movement because of the disrupted proprioceptive information. . Our analysis showed a difference in priority management of the GRF components between an almost dynamic movement and a dynamic movement (step initiation vs gait) . However, the vertical force is the systematic reflection of the patient’s strategies during standing , gait initiation and gait . The evolution of the GRF vertical component is the result of the dynamic behavior of the mediolateral and anteroposterior forces . This vertical force affected directly by the individual’s mechanical behavior is also under the influence of asymmetric properties generated by the AIS pathology .
Whereas the spinal cord of the healthy subject is characterized by a perfect symmetry in the frontal plane and with sagittal curvatures that balance themselves . The scoliosis deformation induces a spinal cord asymmetry in all the different planes . When the spinal cord is symmetric (healthy subjects) and when it is asymmetric (AIS patients), the symmetric bearing of a schoolbag triggers spatiotemporal disruptions of GRF on the gait movement . For the SG, these dynamic strategies plus the addition of an external mass must be associated to the compensatory strategies induced by spine deformities. So, just like when a control subject carries a schoolbag in an asymmetric manner, the scoliosis patient presents an asymmetry of masses’ distribution on the trunk, this was even quantified in a sitting position . In our study, all AIS patients presented right thoracic curvatures with a displacement of the center of gravity towards the right side (convex side – coronal plane), right rotation (gibbosity – horizontal plane), and backward displacement (sagittal plane) . Therefore, the patient manages the movement from a specific biomechanical situation correlated to the spine deformation and type of scoliosis . Our results showed a disrupted behavior on the concave side of the curvature, corresponding to the side associated to a decreased ischiatic loading in a sitting position .
The morphology progression during growth, related to the evolution of the spine deformation could explain a more variable movement management for AIS patients than for control subjects. This fact may explain the increase of the GRF amplitude but also the variability increase. Actually, for all studied parameters, AIS generates a variability increase compared to control subjects, for gait, standing position or lateral stepping .
Our results suggest that the dynamic behavior is directly adapted according to the biomechanical, and neurophysiological characteristics of the individual patient . Indeed, the progression of the spine deformity and the dynamic compensatory phenomenon must be taken into account for AIS therapeutic care. The results of our work associated to the literature show the relevance of a posture dynamic evaluation for patients presenting an idiopathic scoliosis in clinical practice. Future studies will have to determine reliable clinical criteria determining specific characteristics for AIS patients.
1.5
Conclusion
In conclusion, the consequences of AIS linked to morphological modifications induce a compensatory dynamic posture behavior during gait initiation. A slower movement characterizes the patients during gait. This extended duration is linked to an increase of occurrences, amplitudes and impulses of the GRF components compared to control subjects. However, the dynamic patterns are similar between the two groups and between the two limbs initiating the movement. The left side (concave side), associated to the anteroposterior and vertical forces, increases the intergroup differences. The patient’s specific behavior depends on the spine deformation and curvature progression. It appears essential to analyze separately the different GRF to understand the three-dimensional strategies linked to AIS. Consequently, the improvement of assessment methods and AIS rehabilitation treatments must not only include imaging exams and static clinical exams but also a thorough dynamic analysis of daily life activities.
2
Version française
2.1
Introduction
L’initiation de la marche est définie comme la phase de transition entre la posture et la marche . Des actions initiales musculaires et gravitationnelles sont nécessaires pour créer la condition posturodynamique de progression . Ainsi, l’initiation débute par un mouvement du centre de pression vers l’arrière et vers le membre initiant le mouvement alors que le centre de masse se déplace en avant vers la jambe d’appui . Ce découplage du centre de masse et du centre de pression permet de créer les conditions d’aptitude au démarrage . Deux facteurs semblent influencer la vitesse de marche : la longueur de la phase d’ajustements posturaux anticipés et la position initiale du centre de masse du sujet .
L’invariance de l’amorce de la marche vient de l’interdépendance entre les paramètres biomécaniques (position du centre de pression et du centre de masses) et les paramètres spatiotemporels (longueur du pas, temps d’initialisation, temps d’exécution et vitesse d’exécution) .
Certaines pathologies asymétriques des membres inférieurs (gonarthrose, pied bot varus équin, hemiplégie) influencent l’initiation de la marche par une adaptation spatiotemporelle des paramètres cinétiques et cinématiques ainsi que par l’apparition d’asymétries dynamiques . Actuellement, aucune pathologie rachidienne asymétrique n’a été testée lors de l’initiation du pas, alors que nous pensons que les mécanismes d’équilibration impliquent le tronc, comme cela a pu être rapporté lors de la marche .
Les études concernant la posture et la marche ont permis de déceler des caractéristiques posturodynamiques propres à la scoliose idiopathique de l’adolescence (SIA) . Cette pathologie est caractérisée par une déformation rachidienne tridimensionnelle (incurvation latérale, diminution des courbures sagittales et gibbosité) , particulièrement évolutive lors de l’adolescence . Malgré les progrès de la recherche et un nombre très conséquent de travaux dans ce domaine, la SIA reste encore une énigme étiologique. Une interaction entre l’ensemble des hypothèses semble être la plus probable . Ainsi, un gène défectueux provoquerait un défaut de synthèse de la mélatonine qui engendrerait un dysfonctionnement provisoire du système nerveux lors de la croissance intégrant des troubles des systèmes visuel , proprioceptif et vestibulaire . Ceux-ci seraient à l’origine de l’instabilité posturale et des stratégies adaptatives observées chez les patients scoliotiques lors de la posture et de la marche . Alors que ces travaux ont porté sur la cinématique et la cinétique, une étude récente a montré que l’analyse cinétique est plus fiable que la cinématique pour caractériser le comportement posturodynamique des patients porteurs d’une SIA .
Lors de la position debout, la SIA induit une augmentation de l’amplitude des oscillations posturales et de l’excursion du centre de pression par rapport à des sujets témoins . La déformation rachidienne modifie la relation entre la position des différents segments du corps (rachis et membres), ce qui induit le développement de nouvelles stratégies pour maintenir l’équilibre postural . Deux facteurs d’instabilités ont pu être identifiés chez les patients :
- •
la SIA à simple courbure ;
- •
le morphotype ectomorphe (longiligne) .
L’analyse d’un pas latéral et d’un pas antérieur a montré un déplacement du centre de pression augmenté par rapport aux sujets témoins, associé à un comportement asymétrique des forces de réaction du sol . Lors de la marche, la SIA implique des perturbations spatiotemporelles de la force de réaction du sol caractérisées principalement par une augmentation de l’asymétrie entre les membres inférieurs et une augmentation de la variabilité des paramètres dynamiques .
À la vue de l’ensemble des perturbations posturodynamiques observées lors de la posture et de la marche, il semble indispensable de caractériser la transition entre ces deux états . La modification de la position du centre de masse liée à la déformation rachidienne devrait influencer particulièrement les stratégies et la vitesse de l’initiation de la marche . Nous pensons que la déformation rachidienne tridimensionnelle asymétrique associée aux perturbations des systèmes sensoriels devrait induire une gestion différentielle entre les patients et les sujets témoins, mais, également entre les pas initiés du côté de la convexité et du côté de la concavité de la déformation . Ces stratégies adaptatives secondaires au processus scoliotique devraient être particulièrement visibles sur la composante orthogonale au sens du mouvement car c’est cette composante de force qui a été décrite comme étant celle qui est prioritairement contrôlée lors du mouvement .
L’objectif de cette étude est de caractériser les stratégies adaptatives des patients présentant une SIA lors de l’initiation de la marche. Nous avons étudié l’influence de la pathologie sur l’initiation du pas, mais également l’influence de la déformation sur les stratégies adaptatives de chaque membre initiant le mouvement.
2.2
Patients et méthode
Vingt-cinq jeunes filles participaient à cette étude dont un groupe « témoin » (GT) de 15 jeunes filles adolescentes et un groupe de dix jeunes filles adolescentes « scoliotiques » (GS). Les deux groupes étaient appariés en âge (pour le GS : 13,8 ± 2,15 vs 12,57 ± 1,34 pour le GT), en taille (pour le GS : 1,6 ± 0,09 vs 1,55 ± 0,073) et en masse (pour le GS : 49,17 ± 8,89 vs 47,55 ± 9,83 pour le GT, Tableau 1 ).







