Abstract
Introduction
Neurectomy of the tibial nerve plays a major role in the relief of disabling spasticity, which is refractory to drug treatment and physiotherapy. Although the immediate postoperative results are generally satisfactory, few evaluations of the procedure’s long-term efficacy have been published.
Objective
To estimate the long-term efficacy of total or partial neurectomy of the motor branches of the tibial nerve (combined with additional orthopaedic surgery in some cases).
Method
A descriptive, retrospective study of 25 brain-damaged patients having undergone neurectomy at least 4 years ago.
Results
The mean post-neurectomy follow-up period was 11 years. Twenty patients became less dependent on the use of walking aids. Of the 18 patients unable to walk barefoot before surgery, 11 could do so after surgery. Of the 12 patients unable to walk on uneven ground before surgery, seven could do so afterwards. The walking distance increased for 20 patients. In 22 cases, the spasticity disappeared immediately after the operation and did not reappear in the long-term. In three other cases, spasticity persisted postoperatively and, in the long-term, affected the soleus (the denervation of which had been incomplete or not performed). Eighty-three percent of the patients were satisfied with the operation’s outcome.
Conclusions
The observed maintenance of the benefits of total or partial neurectomy after an average follow-up period of 11 years confirms the value of this procedure. The few mediocre outcomes (observed in cases of partial neurectomy of the soleus) are in agreement with literature reports and emphasize the role of the soleus in this pathology.
Résumé
Introduction
La neurectomie du nerf tibial joue un rôle important dans un projet de réadaptation en cas de spasticité délétère résistant aux traitements médicaux et à la kinésithérapie. Les résultats postopératoires immédiats sont satisfaisants, mais peu d’évaluations de son efficacité sur le long terme ont été publiées.
Objectif
Évaluer l’efficacité à long terme des neurectomies des branches motrices du nerf tibial, associées ou non à des temps orthopédiques.
Méthode
Étude descriptive, rétrospective, portant sur 25 patients cérébrolésés ayant subi une neurectomie depuis plus de quatre ans.
Résultats
Le recul moyen par rapport à la neurectomie était de 11 ans. Chez 20 patients, les aides de marche avaient été allégées durablement. Onze patients sur 18 pouvaient marcher pieds-nus et sept sur 12 pouvaient marcher sur terrain accidenté alors que cela leur était impossible ou très difficile avant l’intervention. Vingt patients avaient augmenté leur périmètre de marche. Dans 22 cas, la spasticité avait disparu en postopératoire immédiat. Elle n’était pas réapparue à distance. Dans les trois autres cas, une spasticité persistait en postopératoire et était retrouvée à distance sur le soleus sur lequel l’hyponeurotisation avait été incomplète ou non réalisée. Quatre-vingt-trois pour cent des patients étaient satisfaits de l’intervention.
Conclusions
Le maintien à plus de 11 ans des bénéfices valide notre technique de neurectomie. Les moins bons résultats, observés en cas d’hyponeurotisation incomplète du soleus sont en accord avec la littérature et confortent le rôle du soleus dans cette pathologie.
1
English version
1.1
Introduction
In the hemiplegic patient, recovery of the ability to walk and perform transfers is an essential condition for personal independence and the return to a domestic environment. As such, these activities constitute a high priority in rehabilitation programmes . According to the literature, around 80% of the hemiplegic patients treated in physical medicine and rehabilitation departments in France regain the ability to walk alone (either completely unaided or with the use of a walking aid) .
However, foot dysfunction during or after rehabilitation may compromise a patient’s ability to recover functional gait. In the hemiplegic patient, equinovarus foot is the most common leg deformation and most troublesome in terms of gait. Partial neurectomy of the tibial nerve (including neurotomy and the latter’s technical variants) plays a major role in the rehabilitation of disabling spasticity which is refractory to drug treatment and physiotherapy. The goal of partial neurectomy is to correct pathological spasticity, re-establish the foot’s muscle balance and treat any so-called “orthopaedic” bone and joint deformities. Although this procedure is known to have good immediate postoperative outcomes , its long-term efficacy has rarely been assessed . The results of a recent study suggest that the benefit of neurotomy of the spastic upper limb is maintained over time . The objective of the present study was thus to evaluate the long-term efficacy of direct total or partial neurectomy of the motor branches of the tibial nerve (combined with additional “orthopaedic” bone and joint or soft-tissue operations in some cases).
1.2
Patients and methods
We performed a retrospective, descriptive study of adult hemiplegic stroke or head injury patients having undergone total or partial neurectomy of the tibial nerve. The patients were seen in consultation as long as possible after the operation (between December 2007 and January 2008). The same diagnostic, therapeutic and surgical protocol was applied in all cases and consisted of initial physiotherapeutic care, one or more multidisciplinary neuro-orthopaedic team consultations (comprising an orthopaedic surgeon, a nerve surgery specialist and several physical medicine and rehabilitation physicians) and then clinically appropriate neurectomy. The patients had already been assessed immediately after the operation.
1.2.1
Preoperative assessment
The preoperative assessment consisted of:
- •
a detailed examination of the foot, with analysis of motor parameters (evaluation and scoring of the clonic and tonic components of spasticity for the various leg and foot muscles (notably the triceps surae) with the knee extended and flexed), voluntary motor control (notably screening for synkinesis of the tibialis anterior), sensory parameters (screening for cutaneous and deep-tissue sensory disorders) and “orthopaedic” parameters (a forefoot and ankle joint examination and screening for muscle and sheath or ligament retraction);
- •
a review of the use of walking aids;
- •
a gait examination (with the patient barefoot and then wearing their usual shoes) and determination of the gait pattern.
Whenever necessary, motor block of the tibial nerve was performed in order to distinguish between spasticity and muscle retraction and, above all, reversibly simulate the outcome of the neurectomy.
The decision to operate and improve gait was made according to the risk-benefit ratio and whenever an adequate level of functional benefit appeared to be sufficiently likely. Of course, one or more preoperative interviews with the patient and his/her family were of major importance in carefully presenting and reviewing the operation’s objectives (the potential for aid-free walking, improved stability and a greater walking distance) and, above all, limitations (so as not to raise false hopes).
With respect to surgery, the chosen procedure consisted of partial or total neurectomy of the terminal nerve branches of the gastrocnemius and soleus muscles (with no intra-trunkal neurotomy) . We defined the triceps surae branches for neurectomy, i.e. those innervating the medial and lateral heads of the gastrocnemius and one or more branches of the soleus. For each of these branches, we specified the extent of neurectomy (usually 100, 75 or 50%). We also decided whether or not to perform other “orthopaedic” interventions (tendon lengthening, arthrolysis, metatarsal/subtalar arthrodesis, treatment of claw toe deformities, etc) during the same operating session. The clinical examination and the surgical procedures were reassessed by the two surgeons at the patient’s bedside on the eve of the operation.
1.2.2
Immediate postoperative assessment
The immediate postoperative assessment enabled us to note:
- •
the presence or absence of residual tonic and/or clonic spasticity. Unfortunately, these parameters were not always scored on the Ashworth’s scale ;
- •
the presence of persisting varus and/or equinus deformities and their aetiologies (retractions or residual spasticity);
- •
any surgical complications;
- •
the immediate functional benefit: improved gait and a reduced need for orthotic devices and/or walking aids, etc;
- •
patient’s satisfaction.
1.2.3
Long-term assessment
The long-term assessment (performed as long as possible after the operation) included:
- •
identification of postoperative events and ongoing spasticity treatments and/or rehabilitation therapy;
- •
the patient’s age and the date of the neurectomy;
- •
the type of neurectomy and any additional orthopaedic operations performed at the same time;
- •
analysis of interim assessments in the patient’s medical records;
- •
a detailed examination of the foot, including:
- ∘
angle measurement for passive dorsal foot flexion, with the knee extended and flexed,
- ∘
voluntary motor control (good/average/poor/null),
- ∘
screening for synkinetic tibialis anterior activity when standing (via active hip flexion) and synkinesis of use in gait,
- ∘
a residual spasticity score, with separate assessment of the tonic and clonic components for the heads of the triceps surae. Despite the lack of a reliable measurement device and the risk of low accuracy, this evaluation was performed clinically. In particular, differentiation between gastrocnemius and soleus was performed by direct palpation of the body of the muscle. In fact, the soleus (which lies more deeply and is in contact with bone) can be easily identified in the middle third of the leg, immediately behind the tibia’s medial border. The body of the gastrocnemius muscle is proximal and nearer to the surface; one can easily palpate this muscle over the proximal third of the leg (i.e. the most rounded part of the calf). We consider that this examination method is more reliable that the classic distinction of Silfverskiöld retaining, in the presence of an appearing clonus
- ∘
flexed knee, the only responsibility of the soleus:
- –
the tonic component was scored on the Ashworth’s scale (from 0 to 4),
- –
spastic clonus of the ankle was scored on the following scale: 0: absence of clonus; +: rapidly transient clonus; ++: transient clonus; +++: sustained clonus;
- ∘
the presence of spasticity in other muscle groups (notably the tibialis posterior),
- ∘
cutaneous and deep-tissue sensory disorders (the ability to sense knee joint movement and the segmental positions of the hallux and the knee) and any trophic disorders,
- •
a functional gait analysis, to assess whether the situation had changed after the operation and whether the therapeutic effect had persisted over time in terms of:
- •
- ∘
the use of walking aids,
- ∘
the ability to walk (1) barefoot, (2) outside the home and (3) over uneven ground (in a garden or in woodland, for example) at the time of the consultation,
- ∘
the new functional ambulation classification (nFAC) before the operation, immediately afterwards and at the time of the last consultation. Student’s t test was used to check for any statistically significant changes over time,
- ∘
at the end of the consultation, a measure of the comfortable gait velocity on 10 m was performed ;
lastly, we asked the patient about his/her opinion on the operation’s outcome, any changes over time and its efficacy in terms of the changes in the walking distance.
1.2.4
The surgical procedure
Of the many available procedures, surgical treatment of spasticity can draw on neurectomy procedures with resection of the motor fibres involved in the segmental reflexes which cause spasticity and the motoneuron axons; the resulting paralysis of the innervated muscle is proportional to the extent of the fascicular resection. Fascicular neurotomy within the nerve trunk is the most common procedure and has been extensively described in the literature ; it includes an intraneural dissection phase in order to locate the fascicles for resection. This identification is based on the topographic information provided by mapping of the tibial nerve and peroperative electrical stimulation.
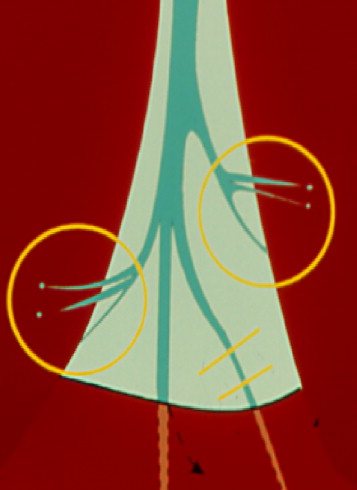
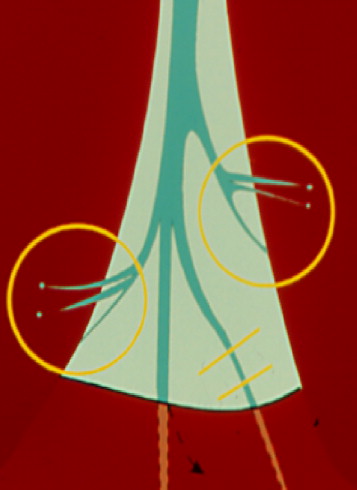
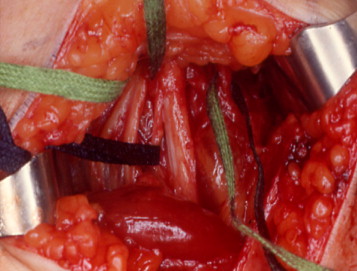
Our operating procedure involved selective neurectomy of the terminal motor branches (downstream of their emergence). Neurectomy was performed on the terminal ramifications of the branch going to the gastrocnemius and the branch of the superior nerve of the soleus ( Fig. 1 ).
1.3
Results
Thirty-seven patients fulfilled our inclusion criteria. Three separate assessments were available for 25 of these subjects (68%) and will thus be described below. Two patients were unable or unwilling to attend the last assessment: one patient had moved far away from the investigating centre and the other refused to participate. Two patients had agreed to participate but failed to attend the consultation. Three patients had died in the meantime and five others were lost to follow-up.
The study population consisted of 15 men (60%) and 10 women (40%). Thirteen patients had right-side hemiplegia and 12 had left-side hemiplegia.
The hemiplegia had vascular and traumatic aetiologies: traumatic head injury (seven cases), ischaemic stroke (13 cases), haemorrhagic stroke (four cases) and thrombophlebitis (one case).
None of the patients (including the stroke patients, in particular) had suffered a relapse since the initial incident.
The mean time since onset of hemiplegia was 38 years (range: 3 to 68 years).
The mean time interval between the incident having caused the hemiplegia and the neurectomy was 5 years and 2 months (range: 6 months to 37 years). The median time interval was 3 years and 2 months.
The mean age of the study population at the time of the last assessment was 54.5 (range: 36 to 81).
The mean time since neurectomy was 11 years and 3 months (range: 4 to 19 years).
All but six of the 25 patients had undergone a tibial nerve block during the preoperative assessment, with partial relief (nine cases) or full relief (10 cases) of the spasticity. Ongoing anticoagulant treatment ruled out the procedure in two patients and a third patient had undergone femoropopliteal bypass surgery on the hemiplegic side. In the three other cases, the reason for the lack of performance of a motor block was not specified in the medical records.
1.3.1
Details of the surgical procedure
Twenty-three patients had undergone neurectomy of the soleus (complete neurectomy in 14 cases, 50% neurectomy in eight cases and 75% neurectomy in one case). The partial neurectomies consisted of an early surgical procedure in which 1 or 2 cm of a group of fascicles were resected and others were left untouched. This procedure was subsequently forsaken in favour of complete resection of the superior branch of the soleus.
Twenty-four patients had undergone partial or complete neurectomy (50, 75 or 100%) of the lateral and medial heads of the gastrocnemius. Complete neurectomy was performed in 12 cases.
Five patients had undergone complete neurectomy of the soleus and the gastrocnemius.
Twenty-one patients had undergone at least one other operation at the same time as the neurectomy:
- •
eight patients had undergone tenotomy of the tibialis posterior;
- •
11 patients had undergone Bardot’s tenodesis procedure (fixation of the distal end of the peroneus brevis to the tendon of the tibialis anterior, in order to re-enable foot eversion);
- •
seven patients had undergone tenotomy of the flexor digitorum longus and six others had undergone tenotomy of the flexor hallucis longus;
- •
one patient had undergone tenodesis of the extensor hallucis longus and the tibialis anterior (Haglund’s procedure);
- •
one patient had undergone medial mediotarsal (talonavicular) arthrodesis;
- •
one patient had undergone neurectomy of the tibialis posterior.
1.3.2
Postoperative complications
Only three superficial scarring problems were observed (slow scarring, local wound infection and subcutaneous bruising).
1.3.3
Spasticity
1.3.3.1
The preoperative assessment
All the patients displayed detrimental spasticity of the triceps surae, which was refractory to drug treatment and physiotherapy. The Ashworth’s score was 3 or 4. Ankle clonus (whether transient or sustained) was always present.
1.3.3.2
The immediate postoperative assessment
Spasticity was evaluated qualitatively (i.e. the score Ashworth was not calculated):
- •
spasticity had completely disappeared in 21 cases;
- •
in one case, the spasticity had disappeared but then rapidly reappeared at the lateral head of the gastrocnemius, with signs of re-innervation on electromyogram. This required repeat surgery with neurectomy of the lateral head of the gastrocnemius and the tibialis posterior (after neurectomy of the gastrocnemius, there was residual activity in the Achilles’ tendon during peroperative electrical stimulation; this was linked to a branch of the tibialis posterior via “coupling” with the triceps surae);
- •
in three cases, tonic and/or clonic spasticity persisted.
1.3.3.3
Last postoperative assessment
The last postoperative assessment was performed after a long follow-up period:
- •
the spasticity had not reappeared in 22 cases: the Ashworth’s score was either 0 (in 21 cases) or 1 (in one case), with the complete disappearance of ankle clonus (in 14 cases) or the persistence of slight, rapidly transient ankle clonus (in eight cases);
- •
for the three patients still affected by spasticity immediately after the operation, this condition was still present at the last assessment: one patient had an Ashworth’s score of 1 and sustained ankle clonus. The second patient only had sustained ankle clonus and the third had an Ashworth’s score of three and transient clonus. Spasticity mainly affected the soleus, for which neurectomy had been partial (50%) or not performed at all.
Hence, only one case of (rapid) re-innervation was observed. This complication responded favourably to repeat surgery.
Overall, the neurectomy’s impact on spasticity was maintained over the long-term distance because this symptom was absent (or minimal) in 22 of our 25 patients. For the three patients with persistent spasticity, the condition had not worsened.
Lastly, we did not observe any symptoms related to hypercorrection (such as iatrogenic talipes foot).
1.3.4
Functional benefits
Twenty of the 23 patients (and not 25, since two patients had been able to walk unaided in flat shoes before the operation) had a long-term lowering of orthotic devices or walking aids (e.g. shoes, a walking stick, a brace, a walking frame, a wheelchair, etc) ( Table 1 ).
| Number of patients | |||
|---|---|---|---|
| Before surgery | Immediately after surgery | Long after surgery | |
| Flat town shoes | 3 | 13 | 12 |
| Heeled town shoes | 6 | 6 | 5 |
| Light orthopaedic shoes | 3 | 3 | 5 |
| Heavy orthopaedic shoes | 13 | 3 | 3 |
| Ankle-foot brace | 4 | 2 a | 3 a |
| Knee-foot brace | 2 | 0 | 0 |
| A single walking stick | 16 + 1 (outside) b | 10 + 5 (outside) b | 10 + 6 (outside) b |
| Tripod cane | 1 | 1 | 1 |
| Walking frame | 1 | 0 | 0 |
| Wheelchair permanently | 3 | 0 | 0 |
| Wheelchair outside the home | 5 | 4 | 4 |
a Including one patient who wore a knee-foot brace before the operation.
Three patients did not enjoy continued benefits:
- •
although the first patient did not experience any functional improvements, the initial situation had not worsened. This patient was one of those with significant residual spasticity of the soleus (after 50% neurectomy of the latter and 100% neurectomy of the gastrocnemius) but did not wish to undergo repeat surgery;
- •
the second (traumatic head injury) patient’s condition had worsened, with the appearance of non-spastic muscle retraction requiring the use of heavy orthopaedic shoes. The patient suffered from cognitive disorders and was not receiving maintenance physiotherapy. Furthermore, her medical follow-up was very erratic. Achilles’ tendon lengthening would have been possible but the patient did not wish to undergo repeat surgery;
- •
although the third patient had been less dependent on walking aids immediately after the operation, knee pain appeared after several years and was related to significant recurvatum (but with no recurrence of spasticity). The condition was treated through use of orthopaedic shoes and a brace.
1.3.4.1
Ability to walk barefoot
Of the 18 patients who found it impossible or very difficult (i.e. with the need for significant technical assistance) to walk barefoot before the operation, 11 became able to do so immediately afterwards. This benefit has been maintained ever since.
1.3.4.2
Ability to walk on uneven ground
Of the 12 patients who found it impossible or very difficult to walk on uneven ground before the operation, seven became able to do so immediately afterwards. This benefit has been maintained ever since.
1.3.4.3
Ability to walk outside the home
Of the five patients unable to walk outside before the operation, four became able to do so immediately afterwards. This benefit has been maintained ever since.
1.3.4.4
Confort
For the three patients with skin lesions due to rubbing on the shoe or rapid wear of the shoe, comfort improved markedly.
1.3.4.5
New functional ambulation classification scores
Comparison of the mean nFAC scores ( Table 2 ) before the operation (5.12), immediately afterwards (5.8) and long afterwards (5.8) revealed a significant overall improvement ( P < 0.02).
| New functional ambulation classification (nFAC) | Number of patients | |||
|---|---|---|---|---|
| Before surgery | Immediately after surgery | Long after surgery | ||
| 0 | Patient cannot ambulate or requires assistance from more than one person during ambulation | 0 | 0 | 0 |
| 1 | Patient requires permanent assistance from no more than one person during ambulation | 1 | 0 | 0 |
| 2 | Patient requires intermittent assistance from no more than one person during ambulation | 2 | 0 | 0 |
| 3 | Patient can ambulate without manual contact but needs verbal assistance | 1 | 0 | 1 |
| 4 | Patient can ambulate independently on level surfaces but cannot negotiate stairs | 1 | 2 | 1 |
| 5 | Patient can ambulate independently on level surfaces but requires a person’s assistance to negotiate stairs (manual contact or just supervision) | 7 | 5 | 4 |
| 6 | Patient can ambulate independently on level surfaces and can negotiate stairs without assistance by using the handrail or a walking stick | 10 | 14 | 15 |
| 7 | Patient can ambulate independently on level surfaces and can negotiate stairs without assistance or use of a walking aid but does so abnormally (slow pace, limping) | 3 | 4 | 4 |
| 8 | Patient can ambulate independently on level surfaces and can negotiate stairs normally, without use of the handrail or a walking stick | 0 | 0 | 0 |
| Total | 25 | 25 | 25 | |
| Mean nFAC | 5.12 | 5.8 | 5.8 | |
1.3.4.6
Mean comfortable gait speed
The mean comfortable gait speed was 0.52 m/s at the last assessment. This parameter had not been measured before or immediately after the operation. The median value was 0.5 m/s.
1.3.5
Repeat surgery
Several patients had undergone repeat surgery:
- •
seven patients underwent repeat surgery for complications of their hemiplegia:
- ∘
three patients had persistent, non-spastic foot deformities related to muscle retraction and had undergone an additional “orthopaedic” operation a few months after the neurectomy: Achilles’ tendon lengthening (in two cases) and gastrocnemius lengthening (in one case), combined with Bardot’s procedure. One patient had developed a retracted, non-spastic equinovarus foot due to reflex neurodystrophy and underwent Achilles’ tendon lengthening several years after the neurectomy,
- ∘
three patients had developed claw toe several years after the operation and thus required tenotomy of the toe flexors;
- •
two patients underwent surgery for problems unrelated to their hemiplegia:
- ∘
one patient underwent several additional operations for deformities resulting from major foot trauma incurred at the same time as the traumatic head injury (again, with no recurrence of spasticity),
- ∘
one head injury patient had also undergone subtalar arthrodesis for a fracture suffered in a road accident.
Hence, none of the subsequent operations (except the case of spontaneous neurotization) were related to recurrence of spasticity.
1.3.6
Patient’s satisfaction
Twenty-four patients answered this question. Eighty-three percent of the patients (i.e. 20 out of 24) stated that they were satisfied with the operation’s outcome (both immediately afterwards and long afterwards).
1.3.7
Patient’s satisfaction with their walking distance
During the last interview, patients were asked to compare their postoperative and preoperative situations:
- •
immediately after surgery, the walking distance had increased in 20 out of 25 cases (80%);
- •
long after surgery, the walking distance had increased (relative to the preoperative situation) in 20 out of 25 cases;
- •
in five cases, the walking distance had decreased between the immediate postoperative assessment and the last assessment but was still greater than the preoperative distance. This decrease was related to intercurrent events: a fall (in one case), a fall with hip pain (in one case), a subtalar fracture following an accident (in one case), neuropathic pain at the back of the foot (in one case) and knee pain (in one case).
1.4
Discussion
1.4.1
Bias and limitations
In order to evaluate the study results as objectively as possible and thus avoid bias potentially related to worsening of the condition (degenerative conditions, for example), we decided to only include patients presenting with acquired, non-degenerative hemiplegia (i.e. with traumatic and vascular aetiologies).
The study limitations were as follows:
- •
the partially retrospective nature of the study design, with a number of missing data items (preoperative and immediately postoperative gait speed, for example);
- •
the low number of patients;
- •
the subjective nature of certain data items, such as patient satisfaction and walking distance (since the latter was difficult to determine otherwise).
However, we also based our analysis on valid, objective data, such as spasticity measurements and functional benefits.
One key strength of the present study is its long post-neurectomy follow-up period (mean period: 11 years and 3 months; range: 4 years and 1 month to 19 years); to the best of our knowledge, this is the longest follow-up to be published. In fact, few studies have evaluated the long-term efficacy of tibial nerve neurectomy . In 1988, Sindou and Mertens reported on a series of 53 patients with an average follow-up period of 3 years (range: 15 months to 10 years). In 2000, Decq et al. described a series of 46 patients with an average follow-up period of 15 months (range: 8 to 28 months). In 2003, Roujeau et al. published the results for six patients with an average follow-up period of 29 months (range: 10 to 48 months) and Deltombe’s et al. 2006 publication reported on three cases monitored over 2 years. In 1998, Berard et al. published results for 13 paediatric patients with an average follow-up period of 3.2 years (range: 1.5 to 5.3 years).
1.4.2
The surgical procedure
Fascicular intra-trunkal neurotomy enables controlled, partial neurectomy but runs the risk of:
- •
postoperative pain syndrome, due to the trauma and ischaemia induced by intraneural dissection. This neuropathic-type pain can be particularly refractory to treatment;
- •
unintentional damage to sensory components: this is likely to be particularly harmful in patients with poor foot control and thus high-pressure zones.
We believe that these risks are too high and so we adopted a partial neurectomy technique, which does not require intraneural dissection and directly targets the tibial nerve’s terminal motor branches. This peripheral neurectomy procedure is not new but fell into disuse because of the supposedly high rate of nerve regrowth. In order to circumvent this disadvantage, we worked on the following aspects:
- •
the procedure does not result in neurotomy per se ; it corresponds to neurectomy with 1 or 2 cm of nerve resection, in order to avoid any risk of complete nerve regrowth;
- •
the branches are located with respect to the local anatomy and are unambiguously confirmed by peroperative electoral stimulation;
- •
great attention is paid to the proximal end of the neurectomy zone by checking that it remains well clear of the adjacent muscle body. We try to keep a gap of at least 1 cm between these two structures, in order to avoid any risk of direct muscle neurotization by secondary nerve regrowth;
- •
the partial neurectomy only affects the gastrocnemius and the soleus. In fact, the efferents to the tibialis posterior and (above all) to the flexor digitorum longus and the flexor hallucis longus are usually too distal for use of this method. Any weakening of the latter muscles is implemented peripherally via direct action on the end tendons.
This procedure has a certain number of advantages ( Fig. 2 ):
- •
it is technically simple and does not require significant optical magnification or the use of a surgical microscope. Simple magnifying glasses (with a magnification of 2.5 to 3) are sufficient;
- •
it enables selective neurectomy of the gastrocnemius. The fact that there are three terminal ramifications of the afferent branch enables selective, partial neurectomy (100, 75 and 25% or even 50%, due to the frequent presence of one ramification, which is larger than the others) and can be used optionally on one or more of gastrocnemius’ heads. In terms of the soleus, the superior nerve is easily identified and the literature data suggest that neurectomy of the latter is sufficient ;
- •
the procedure is compatible with a lateral decubitus position, since the leg is held by a support on each side of the popliteal region. This position is also compatible with subnormal hip mobility: internal rotation enables good exposure of the popliteal fossa and external rotation provides access to the anterior part of the neck of the foot and the foot’s dorsal aspect. Under these conditions, it is possible of perform other “orthopaedic” operations (such as peripheral tenotomies or tendon transfer) during the same anaesthetic session without changing the patient’s position.
1.4.3
Long-term spasticity
Long-term spasticity had almost completely disappeared in 22 of our 25 patients (including one after repeat neurectomy), i.e. 88% of the study population. These results confirmed the efficacy of our neurectomy procedure in relieving spasticity; the proportion of good outcomes is comparable to that reported in the literature for fascicular neurotomy procedures. Feve et al. reported that spasticity has disappeared in 91% of patients (11 out of 12, evaluated on the Held’s scale ). Caillet et al. observed the disappearance of the spasticity in all nine patients (rated on the modified Ashworth’s scale) , whereas Decq et al. noted the disappearance of spasticity in 95% of patients (44 out of 46, evaluated on the modified Ashworth’s scale and the Tardieu’s scale ). Lastly, in two publications by Sindou et al., spasticity (as evaluated on the Ashworth’s scale) disappeared in 89% (33 out of 37) and 92% (57 out of 62) of patients, respectively ).
In the three (out of 25) patients with incomplete outcomes, spasticity persisted immediately after and long after the operation. It is noteworthy that the spasticity mainly affected the soleus, for which the neurectomy had been incomplete (50%) or not performed. Neurectomy (75 or 100%) was chiefly performed on the gastrocnemius. These results are in agreement with the literature: indeed, by performing selective motor blocks of the soleus and the gastrocnemius in a series of 16 patients, Decq et al. demonstrated the predominant role of the soleus, which was fully responsible for the spasticity in 75% of cases. The gastrocnemius alone was responsible for 12.5% of cases, whereas both muscles were involved in the remaining 12.5%. Three other more recently published studies also confirm these results . It is noteworthy that we inconsistently observed a lower branch of the soleus nerve; when present, it emerged over a distance of between 25 and 156 mm (82 mm, on average) across the popliteal fold . This location can thus be very distal and it may be impossible to resect this branch when using the initial approach. Some researchers suggest that this branch has only a slight effect on spasticity because selective block of the superior branch of the soleus nerve inhibits the patients’ spasticity. However, these studies deal with small series of patients . In our study, the three cases of persistent spasticity and the one case of early re-innervation can be explained without the action of this branch. Studies with larger series are nevertheless required to establish whether or not the lower branch has a role in spasticity. Of these three patients, only one failed to gain functional benefit and did not wish to undergo repeat surgery. In the second case, the residual spasticity was not unduly troublesome and patient was able to walk freely in flat town shoes. The third patient improved immediately after the operation but then lost some of the benefits due to heminegligence and the resulting functional fluctuations.
We observed one case of re-innervation at the lateral head of the gastrocnemius (after complete neurectomy of the soleus and the gastrocnemius). Decq et al. reported just 1% of spasticity recurrence in the leg (regardless of the type of neurectomy), whereas Buffenoir et al. did not observe any recurrence of spasticity 10 months after the operation (in 55 patients). In contrast, the results of tibial nerve neurectomies in children are less good; Berard et al. reported that spasticity recurred in eight out of 13 children (61%) between 5 and 17 months after the operation (using the same intrafascicular surgical procedure). The biopsies performed in four cases evidenced re-innervation of the surgically denervated muscle fibres. However, the reason for these relapses was not unambiguously demonstrated. In an electrophysiological follow-up study, Roujeau et al. confirmed that fascicular neurectomy did not induce permanent denervation. There is a re-innervation by sprouting of residual alpha motoneurons, but interruption of myotatic reflex is still abolished in the long-term, which means a permanent damage on reflex afferences. For them, motor re-innervation is therefore probably not responsible for recurrence of spasticity because the myotatic reflex was still abolished. The question of other central and peripheral mechanisms (including the muscles themselves) behind this residual hypertonia (particularly in the child) arises and thus remains to be investigated.
1.4.4
The new functional ambulation classification score
The nFAC score revealed a significant improvement. Nevertheless, this scale did not appear to be very pertinent for our assessments because it took account of items for which improved foot stability does not necessarily result in functional gain (notably the ability to climb stairs for scores of five or more). The nFAC scale has very rarely been used in the various published studies evaluating the efficacy of tibial nerve neurectomy: only one recent study recent by Rousseaux et al. compared the respective effects of botulinum toxin and tibial nerve neurectomy on spasticity and functional parameters. The results showed an improvement in the nFAC score (0 to 5) but only when walking barefoot. The improvement was greater after neurectomy.
1.4.5
The mean comfortable gait speed
The mean comfortable gait speed over 10 m was 0.52 m/s but, unfortunately, this parameter had not been measured before the operation. Hence, the effect of tibial nerve neurectomy on gait could not be evidenced. In an initial study, Caillet et al. noted a significant improvement in gait speed but this outcome was not confirmed in a subsequent study of a more homogeneous population with a high degree of personal independence in terms of gait : the mean gait speed was 0.51 m/s before neurectomy and 0.54 m/s 6 months afterwards. Decq et al. and Feve et al. did not see any improvement. Only Buffenoir et al. noted a gain in the comfortable gait speed while barefoot and when wearing shoes (increasing from 0.18 to 0.29 m/s and from 0.24 to 0.33 m/s, respectively) on a series of 55 patients.
1.4.6
Additional surgery
For the four patients who underwent orthopaedic surgery (lengthening, plus Bardot’s procedure in some cases), it is clear that the functional benefit was related, at least in part, to this additional operation. Given the population of patients studied here, the existence of additional operations was inevitable . However, it should be noted that none of these cases presented a recurrence of spasticity and that only retractions were involved.
We wish to emphasize the importance of regular, long-term medical follow-up for preventing secondary complications – notably retraction of the triceps but also claw toe (the three cases in our series underwent tenotomy of the toe flexors) – which are frequent after the profile of the sole of the foot has been significantly modified.
The long-term efficacy of tibial nerve neurectomy was objectively evidenced by the lasting functional benefit in terms of gait (an increased walking distance (20 of the 25 patients concerned), reduced need for walking aids (20 of the 23 patients concerned) and the ability to walk barefoot (11 of the 18 patients concerned), on uneven ground (seven of the 12 patients concerned) and outside (four of the five patients concerned) and improved comfort for orthopaedic shoe wearers (all three patients concerned).
The patients were generally satisfied with the outcome of the operation (83%).
1.5
Conclusion
This work demonstrated the validity of our procedure for direct neurectomy of the motor branches of the tibial nerve, in terms of a lasting effect on spasticity (mean follow-up period: 11 years). The operation is simple and complication-free. Our results also confirm the importance of the soleus in the origin of spasticity; incomplete outcomes corresponded to insufficient, partial neurectomy of this muscle.
Partial neurectomy of the tibial nerve is a surgical treatment of choice for foot hemiplegia in the adult as part of an overall patient management strategy which:
- •
includes consultations and the implementation of multidisciplinary therapeutic care;
- •
is based on an accurate diagnosis, which takes account of not only spasticity in all its forms (spread, forms of expression, intensity, etc) but also the overall accompanying symptoms, i.e. voluntary motor control of the tibialis anterior and the peroneal muscles, the presence or absence of synkinesis, the presence or absence of cutaneous and (above all) deep-tissue sensory disorders (the intensity of which may constitute a contraindication or at least limit therapeutic expectations), and bone and joint status (and the distinction between spasticity, on one hand, and joint stiffness, on the other). Optimal integration of neurosurgical and additional orthopaedic procedures is therefore essential .
Conflict of interest statement
The authors have not declared any conflict of interest.
2
Version française
2.1
Introduction
La récupération de la marche et des transferts, condition essentielle de l’autonomie et du retour à domicile, est un objectif prioritaire de la rééducation de l’hémiplégique . Ainsi de nombreux travaux montrent que environ 80 % des hémiplégiques rééduqués (en service de médecine physique et réadaptation) retrouvent une marche indépendante avec ou sans aide technique .
La survenue d’un dysfonctionnement du pied en phase de rééducation comme en phase séquellaire hypothèque la valeur fonctionnelle de la marche. Chez le patient hémiplégique, l’attitude du pied en varus équin est la déformation la plus habituelle du membre inférieur et celle qui perturbe le plus la marche. Les interventions d’hyponeurotisation du nerf tibial (dont les neurotomies au sens large et leurs variantes techniques) jouent un rôle important dans un projet de réadaptation en cas de spasticité délétère résistant aux traitements médicaux et à la kinésithérapie. Cette chirurgie a pour but de corriger une spasticité pathologique, de rétablir l’équilibre musculaire du pied et traiter d’éventuelles déformations ostéoarticulaires (dites « orthopédiques »). Elle a fait la preuve de bons résultats immédiats , mais son efficacité n’a pas vraiment fait l’objet d’une évaluation à long terme . Au membre supérieur, une étude récente semble montrer que le résultat des neurotomies se maintient au long cours . L’objectif de cette étude est donc d’évaluer l’efficacité à long terme des neurectomies directes des branches motrices du nerf tibial (totales ou partielles), associées ou non à des temps complémentaires ostéoarticulaires ou sur les parties molles (temps orthopédiques).
2.2
Patient et méthode
Il s’agissait d’une étude rétrospective, descriptive effectuée chez des hémiplégiques adultes par accident vasculaire cérébral (AVC) ou traumatisme crânien, opérés d’une neurectomie sélective du nerf tibial. Ces patients avaient été revus en consultation, à distance de l’intervention, entre décembre 2007 et janvier 2008. Tous les opérés avaient fait l’objet du même protocole diagnostique et thérapeutique. Ce dernier comportait une prise en charge kinésithérapeutique initiale, puis une (ou plusieurs) consultation(s) multidisciplinaire(s) de neuro-orthopédie (réunissant un chirurgien orthopédiste, un spécialiste de la chirurgie nerveuse, et des médecins de médecine physique et de réadaptation) et la réalisation d’une neurectomie adaptée à la situation clinique. Les opérés avaient déjà été évalués en postopératoire immédiat.
2.2.1
L’évaluation préopératoire
L’évaluation préopératoire lors de cette consultation comprenait :
- •
un examen analytique du pied. Sur le plan moteur, pour la spasticité : une évaluation et une cotation de la composante clonique et tonique des différents muscles de la jambe et du pied et notamment pour le triceps surae, genou étendu et fléchi ;
- •
une appréciation de la commande motrice volontaire, la recherche de syncinésies du tibialis anterior notamment. Sur le plan sensitif : la recherche de troubles de la sensibilité superficielle et profonde. Et sur le plan « orthopédique » : un examen articulaire (cheville, couple de torsion et avant-pied), la recherche de rétractions musculaires et capsuloligamentaires ;
- •
une analyse des aides techniques de marche ;
- •
un examen de la marche pieds-nus (si possible) et avec les chaussures habituelles, et une détermination du schème de marche.
Chaque fois que nécessaire, un bloc moteur du nerf tibial était réalisé pour faire la part respective de la spasticité et des rétractions musculaires, et surtout simuler, de façon réversible, le résultat de la neurectomie.
La décision chirurgicale, motivée par un objectif d’amélioration des possibilités de marche, était retenue, à la lumière du rapport avantages/risques, à chaque fois que le bénéfice fonctionnel apparaissait suffisamment fondé en termes de probabilité et de qualité. Bien entendu, l’entretien préopératoire, avec le patient et sa famille avait une importance de tout premier plan, pour préciser les objectifs de l’intervention et surtout ses limites, afin d’éviter de susciter des espoirs hors de proportion avec la réalité thérapeutique. Lors de ces entretiens, volontiers répétés, les objectifs de l’intervention (allègement des aides de marche, amélioration de la stabilité, du périmètre de marche) étaient soigneusement et clairement passés en revue.
Sur le plan chirurgical, la technique était celle d’une hyponeurotisation des rameaux terminaux des nerfs du gastrocnemius et des nerfs du soleus sans aucun temps de neurotomie intratronculaire . Pour le triceps surae étaient définies les branches sur lesquelles devaient porter les différentes neurectomies, à savoir rameaux destinés aux chefs médial et latéral du gastrocnemius et branches(s) du soleus. Pour chacune de ces branches était précisé le pourcentage d’hyponeurotisation (le plus souvent 100 ou 50 %, voire 75 %). De même était décidée l’indication d’éventuels temps « orthopédiques » associés (allongements tendineux, arthrolyse, arthrodèse du couple de torsion, cure de griffes d’orteils). L’examen clinique et les modalités de l’intervention étaient réévalués la veille de l’intervention, au lit du malade par les deux opérateurs.
2.2.2
L’évaluation postopératoire immédiate
L’évaluation postopératoire immédiate avait permis de noter :
- •
l’existence ou non d’une spasticité tonique et/ou clonique résiduelle. Elle n’avait malheureusement pas toujours été évaluée précisément par l’échelle d’Ashworth ;
- •
l’existence de déformations persistantes (varus et/ou équin) et leur étiologie (rétractions ou spasticité résiduelle) ;
- •
les complications liées à la chirurgie ;
- •
le bénéfice fonctionnel immédiat : amélioration de la marche, allègements de l’appareillage et/ou des aides techniques ;
- •
la satisfaction du patient.
2.2.3
L’évaluation à distance
L’évaluation à distance, au recul maximum, comprenait :
- •
la recherche d’évènements intercurrents depuis l’intervention, les traitements antispastiques actuels et la poursuite de la rééducation ;
- •
l’âge du patient et la date de la neurectomie ;
- •
le type de neurectomie et les temps orthopédiques éventuels ;
- •
une analyse des évaluations intermédiaires dans le dossier médical ;
- •
un examen analytique du pied avec :
- ∘
la mesure angulaire de la dorsiflexion passive du pied, genou étendu et fléchi,
- ∘
la cotation de la commande motrice volontaire (bonne/moyenne/faible/nulle),
- ∘
la recherche d’une activité syncinétique du tibialis anterior lors de l’examen debout (par flexion active de hanche) et d’une syncinésie utile à la marche,
- ∘
la cotation de la spasticité résiduelle avait cherché à évaluer séparément les composantes tonique et clonique sur les différents chefs du triceps surae. En dépit du risque d’inexactitude et faute de moyen instrumental de mesure fiable, cette évaluation avait été effectuée cliniquement. En particulier, la différentiation entre gastrocnemius et soleus s’était effectuée par palpation directe des corps musculaires. En effet, le soleus, qui est plus profond et au contact du squelette osseux, est facilement identifiable au tiers moyen de jambe, immédiatement en arrière du bord médial du tibia. Les corps musculaires du gastrocnemius sont superficiels et proximaux. On les palpe facilement au tiers proximal de jambe (sur le galbe du mollet). Cette méthode d’examen nous avait semblé plus sûre que la classique distinction de Silfverskiöld retenant, en présence d’un clonus apparaissant genou fléchi, la seule responsabilité du soleus :
- –
l’évaluation de la composante tonique s’était effectuée selon l’échelle d’Ashworth (de 0 à 4),
- –
l’évaluation de la spasticité clonique par la recherche d’un clonus de cheville, avec la cotation suivante : 0 = absente ; + = clonus vite épuisable ; ++ = clonus épuisable ; +++ = clonus inépuisable ;
- ∘
l’existence de spasticité sur d’autres groupes musculaires (tibialis posterior, notamment),
- ∘
les troubles de sensibilité superficielle et profonde (sens de position segmentaire de l’hallux et du genou et sens arthrokinétique du genou), ainsi que les troubles trophiques éventuels ;
- •
une analyse de la marche avec un bilan fonctionnel permettant de noter si la situation avait évolué après l’intervention et si l’effet thérapeutique s’était maintenu au cours du temps, notamment en termes :
- ∘
d’aides techniques à la marche,
- ∘
de possibilités de marcher pieds-nus, en extérieur (à l’interrogatoire) et sur terrain accidenté (à l’interrogatoire : jardin, forêt…),
- ∘
une mesure de la functional ambulation classification (FAC) modifiée avant l’intervention, en postopératoire immédiat et à distance était réalisée. La comparaison des résultats a été effectuée par un test de Student pour rechercher une différence significative,
- ∘
au décours de la consultation avait été effectuée la mesure d’une vitesse confortable de marche sur 10 m ;
enfin, une appréciation par le patient du bénéfice de son intervention et du profil évolutif avait été demandée, ainsi que l’efficacité sur son périmètre de marche.
2.2.4
Technique chirurgicale
Au sein de très nombreux procédés, la chirurgie de la spasticité peut faire appel à des techniques d’hyponeurotisation obtenue par section des fibres motrices participant aux différents réflexes segmentaires responsables de la spasticité et des axones des motoneurones entraînant de ce fait une paralysie du muscle tributaire proportionnelle à l’importance des sections fasciculaires. Les procédés habituellement utilisés réalisent des neurotomies fasciculaires intratronculaire. Ce sont ces dernières qui font l’objet des publications de la littérature . Ces techniques comportent un temps de dissection intraneural pour repérage des fascicules dont on souhaite interrompre la continuité. Ce repérage se fonde sur les renseignements topographiques apportés par les données de la cartographie du nerf tibial et sur celles de la stimulation électrique peropératoire.
Notre technique opératoire réalise une neurectomie effectuée à la demande sur les branches motrices terminales en aval de leur émergence. La neurectomie porte sur les rameaux terminaux (ramuscules) de la branche destinée au gastrocnemius et sur la branche du nerf supérieur du soleus ( Fig. 1 ).