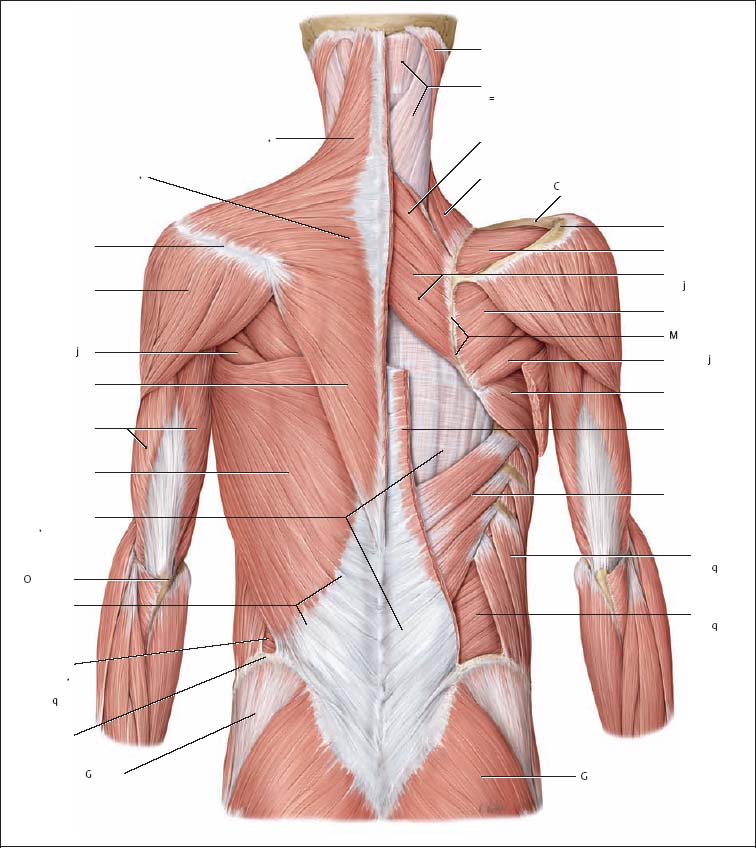
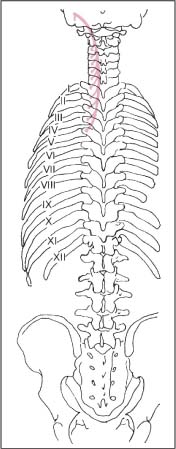
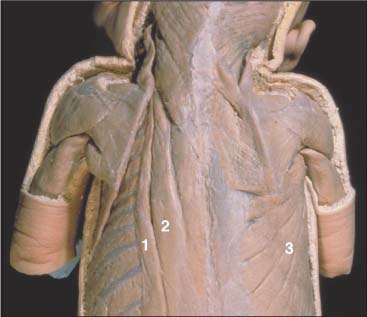
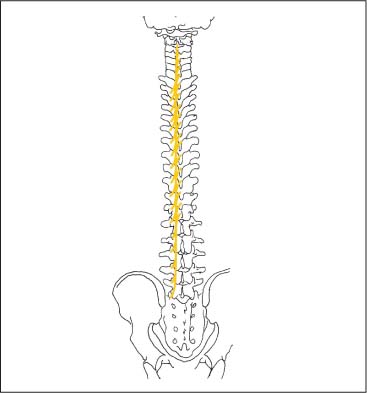
17 Functional Examination and Treatment of Muscles Manual medicine, in addition to addressing the various articular dysfunctions, also emphasizes the importance of a thorough assessment of the muscles and fascia and their proper treatment. The purpose is to “look beyond” the concept of articular dysfunctions per se. The clinician searches for the relevant interactions and connections between muscles, fasciae, and joints. The search of a particular “pain generator,” be it muscle, fascia or articular (somatic) dysfunction, is considered one of the primary goals in the patient’s management. Assuming sinister pathology has been ruled out, the progession of investigation is to assess the patient for localized (e. g. segmental), regional or global dysfunctions that have led to adaptive, compensatory or decompensatory changes, that in turn may again be segmental, regional or global. The five primary goals in the evaluation of muscle and fascia are as follows: 1. To determine the presence of hypertonic muscles, typically called “spasms,” or “tight muscles.” Again, the term “spasm” has no relationship to the neurologically specific term of “spasticity,” as the latter refers to upper motor neuron involvement (e. g. stroke, spinal cord injury, traumatic brain injury, etc.). A term that can be used for “spasm” is “hypertonicity of the muscle,” indicating that there is simply increased muscle tone for that particular patient. On clinical examination, the muscle that is hypertonic in comparison to the uninvolved, “normal” muscles, reveals increased “tension” or “plasticity” upon palpation. There may not be any loss of range of motion, or only little such loss in the presence of a hypertonic muscle. 2. To determine muscle length (to see if there is a shortened muscle in response to injury or associated with a particular dysfunction); this would more typically involve muscles with a preponderance of type I (slow-twitch fiber) muscle fibers. In manual medicine, the assessment of muscle length and the associated loss of range of motion is of great significance as this is part of the assessment of the quality of motion, in addition to the overall range of motion assessment. 3. To determine muscle strength (e. g. weakened due to injury or associated with a particular dysfunction). This would more typically involve muscles with a preponderance of type II (fast-twitch fiber) muscle fibers. The assessment of strength has been part of the standard physical therapeutic evaluation for quite some time, and is equally useful in the field of manual medicine. The muscle strength scale most often used is a six-point scale from “0” (none whatsoever) to “5/5” which has full muscle strength. Naturally, the muscle strength assessment is part of an integral neurologic examination especially when there are signs of muscle weakness (e. g. paresis or overt paralysis). 4. To determine myofascial tissue changes (e. g. myofascial tissue restrictions; e. g. the ease of displacement of the various fascial and myofascial planes and connections); this may also include the evaluation of such empirical entities as the “tender points” (according to the strain–counterstrain system described by LH Jones, D.O. (1981). See Chapters 4 and 6 of this text for additional information. 5. To determine the presence of one or several myofascial trigger points within the context of the definition of the myofascial pain syndrome (Travell and Simons 1992, 1993)(whether a muscle or several muscles act as pain generator [e. g., myofascial pain]) and to determine any abnormal muscle functioning in form of a muscular imbalance between those muscles that have shortened (e. g., typically those muscles that show a preponderance of the slow-twitch fibers) and those that have become weak (e. g., those that have a preponderance of fast-twitch fibers), for instance. The myofascial trigger point examination and treatment are presented in a separate chapter (Chapter 18). For practical purposes it has been found useful to utilize a four-layer system of muscles to assist in the visualization and three-dimensional orientation of the relevant muscles of the back, the neck and the thoracic and lumbar spine (Fig. 17.1 and Tab. 17.1). Like any system, there are advantages and disadvantages, and the interested reader is naturally referred to standard anatomic texts or recent updates (Bogduk, 1997). The lateral and anterior muscles of the neck, trunk and abdomen as well as a number of extremity muscles can be grouped according to particular categorizations as well and are included in this chapter, following those of the back. The four-layer system presented here (Table 17.2) applies to both the muscles of the back and neck. Fig. 17.1 The outermost two layers of muscle of the back and the superficial thoracolumbar fascia that separates them from the deeper two layers (see also Tabs. 17.1 and 17.2). (From Schuenke, Thieme Atlas of Anatomy Vol. I, 2007.)
Examination and Treatment of Muscles–Overview
Muscles of the Posterior Regions of the Neck and Back
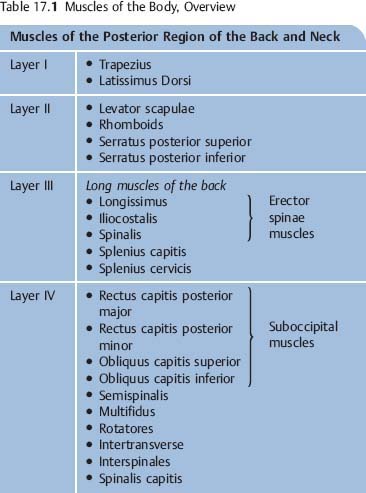
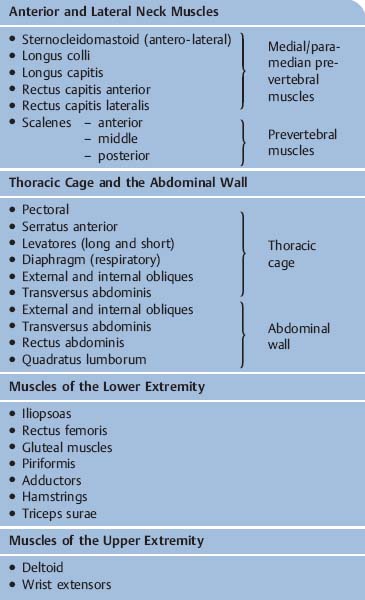
Four-Layer Muscle Orientation | Back and Neck Muscles (posterior layers) | Comments |
Layer I (most superficial) | • Trapezius1 • Latissimus dorsi | Innervated by anterior primary rami primarily 1 a) Trapezius muscle is also innervated by CN IX (spinal accessory nerve), which supplies the major proportion its motor function b) Sensory function of pain and proprioception of trapezius is primarily supplied by anterior primary rami of C 2 and C 3 |
Layer II (superficial) | • Levator scapulae • Rhomboids • Serratus posterior superior • Serratus posterior inferior | Innervated by anterior primary rami primarily |
Thoracodorsal fascia separates Layers I and II from Layers III and IV | ||
Layer III (deep) | Erector Spinae • Longissimus • Iliocostalis • Spinalis Splenius capitis and cervicis (neck) | Innervated by posterior primary rami primarily Some authors include the spinalis as the third partner of the erector spinae group while others only list the ilicostalis and longissimus as the sole two members of the erector spinae |
Layer IV (deepest) | Representatives in the neck • Suboccipital muscles (short nuchal mm) of the neck (in the region between the occipiput and C1 or C2) • Spinalis capitis2 Representatives in the back • Transverso-spinalis muscles • Semispinalis3 • Mulftifidus • Intertransverse • Interspinales4 | Innervated by posterior primary rami primarily 2 This muscle is often not present or is part of the semispinalis capitis 3 The semispinalis starts out in the deepest layer, but when it reaches the neck, it is located near the surface as it inserts at the nuchal line of the occiput 4 Interspinales muscles are present only from C2–T3, and then again from T12 to S2. |
Trapezius Muscle
Origin
The origin of the trapezius muscleh extends between the occipital bone and the twelfth thoracic vertebra. It is useful to anatomically and spondylogenically divide this muscle into three sections: the descending, horizontal, and ascending portions (Figs. 17.2, 17.3).
• Descending portion: The muscle arises from the superior nuchal line, 2 cm lateral to the external occipital protuberance; the nuchal ligament to the sixth cervical vertebra.
• Horizontal portion: Arises from the spinous processes of C7–T3.
• Ascending portion: Arises from the spinous processes of T4–T12.
Insertion
• Descending portion: Inserts at the superior surface of the spine of the scapula, the acromioclavicular joint, and the posterosuperior margin of the lateral third of the clavicle (Fig. 17.2).
• Horizontal portion: Inserts at the superior surface of the spine of the scapula from the base to the acromioclavicular joint. At the spine of the scapula, this portion overlies the insertion of the descending portion (important for palpation) (Fig. 17.2).
• Ascending portion: The inferior edge of the spine of the scapula, between the tuberosity and the lumbar triangle (Fig. 17.2).
Course and Relations
The muscle bundles arising from the occiput run sharply inferiorly, whereas the fibers continuing below course away from the ligamentum nuchae at a sharp angle. The fibers from the most inferior portion of the cervical spine approximate the transverse direction (Fig. 17.3).
Innervation
The descending portion of the spinal accessory nerve and the rami of C2–C4.
Action
• Descending portion: Elevates the shoulder blade.
• Horizontal portion: Adducts the shoulder blade.
• Ascending portion: Depresses the shoulder blade.
Fig. 17.2 Insertions of the trapezius muscle.
a Descending portion
b Ascending and horizontal portions
Fig. 17.3 Course of the trapezius.
Palpatory Approach
To gain an overview of whether myotendinotic changes are present, the muscle belly of the descending portion is grasped by the thumb and index finger half-way between the shoulder and the neck. The examiner moves up and down perpendicularly in the direction of the muscle fibers (Fig. 17.4). At the spinous processes, the spine of the scapula, and the clavicles, the tendinoses are best palpated in the direction of the incoming fibers (Figs. 17.2 and 17.5).
Comments
It should be noted that the descending and ascending portions of the trapezius muscle are partially covered by fibers of the horizontal portion at the level of the spine of the scapula.
Due to its superficial location, the trapezius is a muscle well suited to learn one’s palpatory skills of muscle and the various muscle fiber directions as well as the palpatory assessment of the various other subcutaneous tissues.
SRS Correlation
The trapezius muscle is extremely important for routine diagnosis of the SRS. Seldom is the trapezius muscle responsible for an isolated segmental dysfunction of an individual vertebrae or vertebrae. The individual myotenones result in painful pathological changes (myotendinosis) in the presence of thoracic or lumbar dysfunction (Fig. 17.2).
Evaluation of Muscle Length
Examination Procedure
The trapezius muscle can be examined with the patient sitting or supine. The examiner stands behind the seated or supine patient. Using the forearm, the examiner stabilizes one of the patient’s shoulders at the level of the acromioclavicular joint. While cradling the patient’s parietal region with the other hand, the examiner introduces side-bending and slight rotation to the opposite side (i. e., in the direction opposite to the location of the stabilized shoulder). The examiner evaluates muscle tension and the contour of the trapezius muscle, as well as the range of motion and end-feel at the barrier (Figs. 17.6 and 17.7).
• Descending portion: Flexion and cervical side-bending to the opposite side.
• Horizontal portion: Side-bending to the opposite side without cervical flexion.
Positive Findings
Motion restriction with significant soft end-feel is an indication of muscle shortening and is usually accompanied by an insertion tendinosis at the spine of the scapula or the clavicle.
Fig. 17.4 Palpation of the trapezius.
Fig. 17.5 Palpation of the trapezius.
Fig. 17.6 Length testing of the trapezius, patient seated.
Fig. 17.7 Length testing of the trapezius, patient supine.
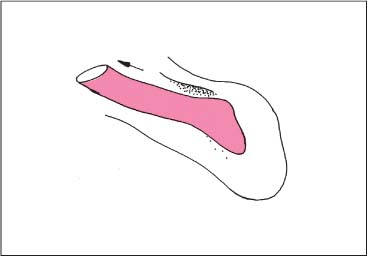
Stretching of the Trapezius Muscle (Descending Portion)
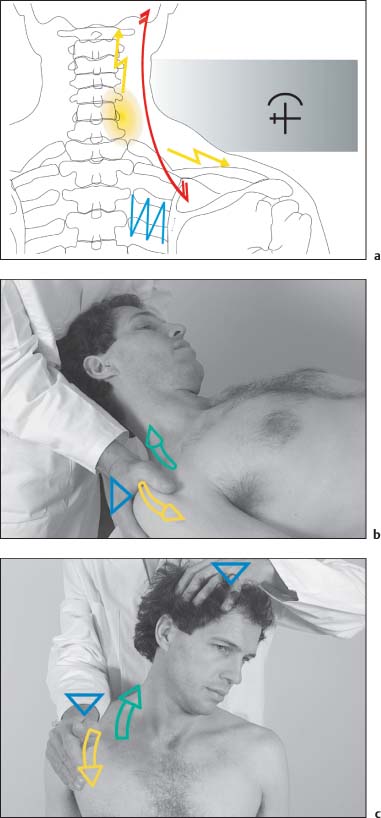
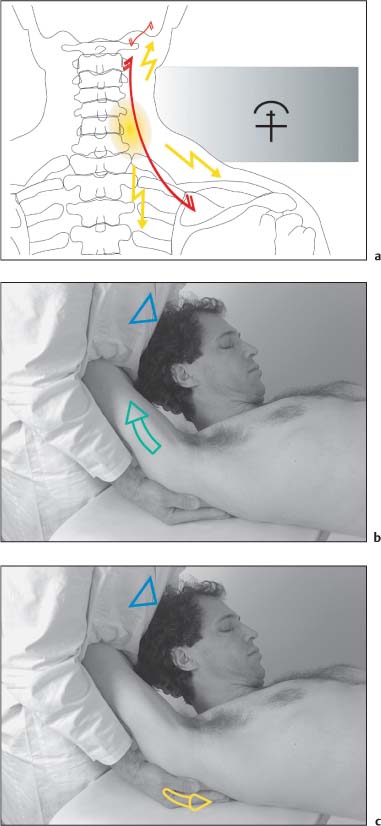
NMT 2 (Figs. I17.1a–c)
Indications
• Pain: Neck pain, often chronic, may radiate toward the occiput and occasionally the arms (a).
• Motion testing: Decreased cervical spine side-bending with soft end-feel.
• Muscle testing: The descending portion of the trapezius muscle is shortened, with characteristic pain when stretched. Often the medial shoulder blade fixator muscles are weak at the same time.
Patient Positioning and Set-up
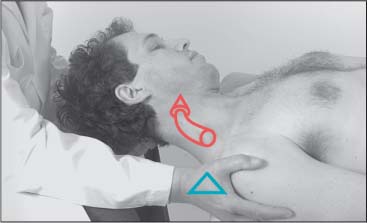
• The patient is supine with his head beyond the examination table.
• The physician places one hand over the occiput while the other hand is placed flat over the patient’s shoulder.
• Passive maximal side-bending and rotation is introduced to the cervical spine (b).
Treatment Procedure
• The physician applies a resistive counterforce against the patient’s shoulder.
• Optimal isometric contraction of the trapezius muscle (descending portion) is performed by the patient.
• During the postisometric relaxation phase the muscle is passively stretched by the physician translating the shoulder girdle inferiorly and laterally (b).
• The cervical spine is guided to its new barrier, and treatment can be repeated, in accordance with the induced stretch of the muscle.
Note: One should introduce some careful traction to the cervical spine when applying this maneuver. This technique can also be carried out with the patient in the sitting position (c).
Comments
If the patient reports dizziness or pain during positioning or with treatment, the cervical spine and the first rib should be examined for segmental dysfunctions and, if necessary, these areas should be treated before stretching this muscle.
Latissimus Dorsi Muscle
Origin
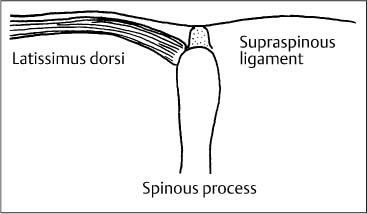
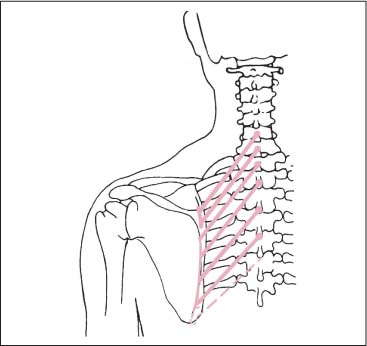
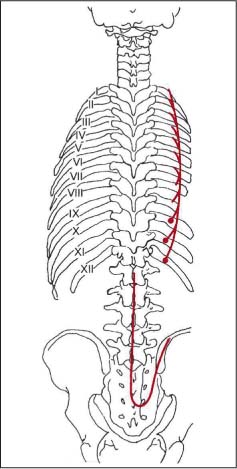
1. Spine: Arises from the spinous processes and the supraspinous ligaments at T7 or T8–L5, and occasionally from the median sacral crest (Fig. 17.8).
2. Iliac region: Arises from the external lip of the iliac crest, at the junction of the iliac tuberosity and the iliac crest.
3. Ribs: Arises as thin fascicles from the outer surfaces of ribs X–XII; between the origins of the obliquus externus abdominis and the insertions of the serratus posterior inferior muscles (Figs. 17.9, 17.10).
4. Thoracolumbar fascia: The fourth and longest structure from which the latissimus dorsi arises is the thoracodorsal fascia.
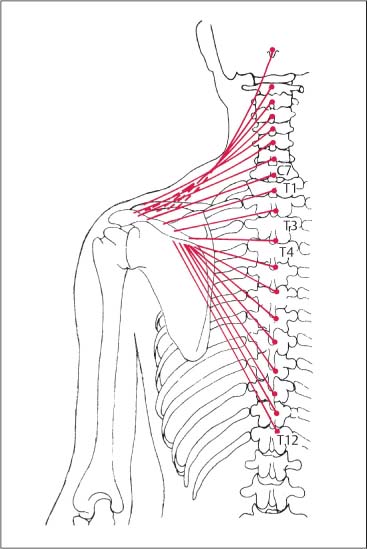
Fig. 17.8 Origin of the latissimus dorsi muscle.
Insertion
Inserts at the proximal end of the crest of the humeral lesser tuberosity, connecting distally to the insertion of the subscapularis muscle. The proximal portion of the insertion belongs to the distal vertebral, iliac, and costal myotenones. The distal portion of the insertion correlates with the proximal vertebral myotenones, which explains the slightly twisted arrangement of the latissimus dorsi muscle (Fig. 17.9).
Course and Relations
The superior bundles run horizontally above the inferior angle of the scapula and cover the teres major muscle at its origin. In the axilla, however, this broad and flat muscles assumes a rather prominent volume.
The lateral edge of the muscle descends almost vertically from the axilla to the ilium (Fig. 17.10).
Innervation
Thoracodorsal nerves C6–C8.
Motor End Plates
The latissimus dorsi muscle is a nonpennate muscle whose fibers converge in the arm. The end plates are arranged in several small units (Fig. 17.11).
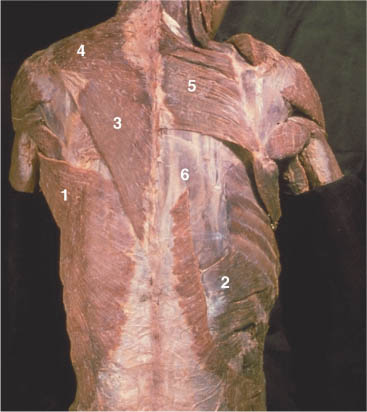
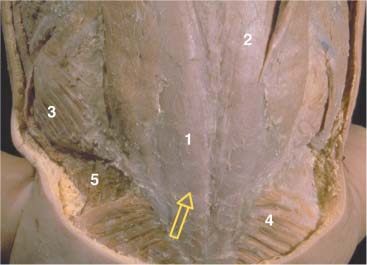
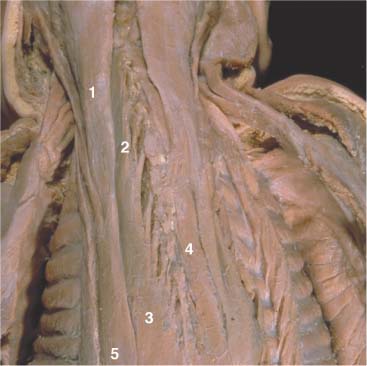
Fig. 17.9 Latissimus dorsi muscle—insertion and arrangement.
1 Latissimus dorsi
2 Serratus posterior inferior
3 Trapezius (ascending part)
4 Trapezius (descending part)
5 Rhomboids
6 Longissimus dorsi and iliocostalis
Action
Adduction, extension, and internal rotation of the arm. The costal origins participate as accessory respiratory muscles.
Palpatory Approach
The iliac crest, the latissimus dorsi muscle, and the external abdominal oblique muscle form the lumbar triangle (of Petit). Due to the flat origin aponeurosis, a myotendinosis in the lumbar region is almost impossible to palpate. Better information about the muscle is gained in the posterior axillary fold (Fig. 17.12). When investigating the condition of the latissimus dorsi muscle, the approach is similar to that described for the descending portion of the trapezius muscle. The myotendinosis is palpated perpendicular to the muscle fiber orientation in both directions: superiorly to the insertion at the crest of the lesser tuberosity and inferiorly. At the spinous processes, the origin of the latissimus dorsi, which is often painful, must be distinguished from the longissimus thoracis muscle, which lies below. The myotendinosis of this flat muscle can be palpated when pressing it against the underlying rib and following it from one costal/vertebral level to the next.
Fig. 17.10 Course of the latissimus dorsi.
Fig. 17.11 Motor end plates of the latissimus dorsi (with kind permission of Dr. J. Chomiak).
Fig. 17.12 Palpation of the latissimus dorsi.
Comments
The latissimus dorsi muscle is frequently involved in the spondylogenic event. Patients usually complain about constant low back pain that follows a fan-shaped distribution.
Levator Scapulae Muscle
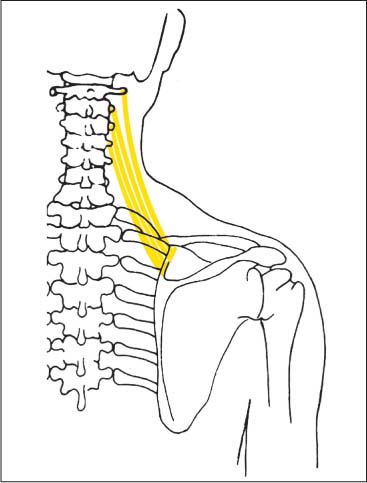
Origin
The levator scapulae muscle arises by four tendinous slips or fascicles from the transverse processes of the first four cervical vertebrae. The uppermost originating fascicle is the strongest and attaches in a rather broad area along the lateral and inferior portion of the transverse process of the atlas. The tendinous slips from C2 to C4 arise from the posterior tubercles. The first two fascicles are completely fused with the tendons of the splenius cervicis muscle, and the last two are generally fused with the longissimus cervicis muscle (Fig. 17.13).
Insertion
The muscle inserts at the medial border of the scapula between the superior angle and the base of the spine of the scapula. The muscle bundles associated with C1 insert immediately below the superior angle of the scapula. The insertions of the muscle fibers originating from C2 to C4 reach the base of the spine of the scapula at a sharp, nearly vertical angle (Fig. 17.13, Fig. 17.17).
Course and Relations
The levator scapulae muscle is located at the back of the side of the neck between the anterior and posterior muscle mass. From the C5 and C6 level and below, the levator scapulae muscle is covered by fibers of the trapezius muscles.
Innervation
C3, C4, C5, via the dorsal scapular nerve.
Motor End Plates
The motor end plates of the levator scapulae muscle are found in the middle one-third of the muscle, following the double innervation of this muscle (Fig. 17.14).
Fig. 17.13 Levator scapulae. Origin at the transverse processes of the first four cervical vertebrae. Insertion at the medial shoulder margin.
Fig. 17.14 Motor end plates (with kind permission of Dr. J. Chomiak).
1 Levator scapulae
2 Sternocleidomastoid
Action
Elevation of the scapula. With the scapula held stationary or fixed, the levator scapulae bends the neck laterally toward the same side as the contracted muscle. It assists the trapezius muscle in raising the shoulder and bracing it against weights.
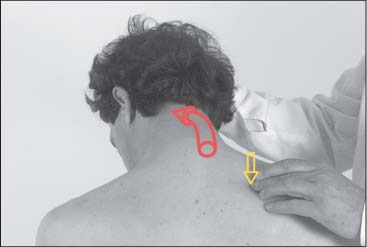
Palpatory Approach
The origins of the levator scapulae are not accessible to palpation and cannot be differentiated from other muscles that originate in the same area. However, the muscle can be palpated relatively easily at its insertion at the medial border of the scapula, especially when there is increased tone (insertion tendinosis). Due to the steeply angled insertion, the palpatory direction is from a superior direction (Fig. 17.15).
Fig. 17.15 Length testing of the levator scapulae. Palpate the insertion at the superior angle at the medial margin of the shoulder. (Note: This may be tender to the patient, especially in the presence of a myofascial trigger point.)
SRS Correlation
Increased muscle tone in the levator scapulae muscle may be associated with dysfunctions in the upper thoracic spine.
Comments
When myotendinotic changes are present in both the levator scapulae muscle and the descending portion of the trapezius muscle, a very painful “cross-myosis” at the T1 level may be observed, about three finger-widths from the spinous process. This may complicate the correct execution of manipulation to be applied to C3 and C4.
Fig. 17.16 Length testing of the levator scapulae. Guide the patient’s head into side-bending away (contralateral side-bending) followed by rotation of the head to the contralateral side and introducing just sufficient flexion. (Memory aid for levator scapulae: side-bend away and rotate away from the side of the muscle to be tested.)
Length Testing of the Levator Scapulae Muscle
Examination Procedure
The arm of the sitting patient is maximally abducted and elevated at the shoulder. This causes the scapula to externally rotate. The patient’s elbow comes to rest against the abdomen of the examiner, who stands behind the patient.
With one hand, the examiner fixates the patient’s superior angle and the upper margin of the patient’s scapula (Figs. 17.15, 17.16). With his other hand, the examiner introduces flexion and rotation of the head in the opposite direction. There are three things the examiner looks for: (1) the presence or appearance of pain associated with this maneuver, (2) any range of motion loss, and (3) palpatory soft-tissue changes proximal to the superior angle including changes in muscle tone with hypertonicity, for instance. If pain or compensatory motions become apparent upon this maneuver, such findings should be followed up with the appropriate examinations accordingly.
Positive Findings
1. Loss of range of motion with soft end-feel, accompanied by pain between the shoulder blades.
2. Typically, when the levator scapulae is shortened, the muscle attachments can be palpated with relative ease at the superior angle and the upper medial margin of the scapula.
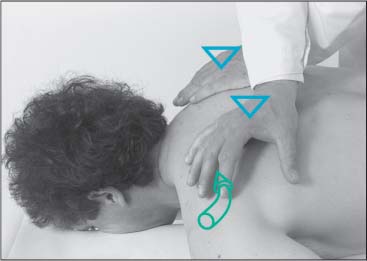
Treatment of the Levator Scapulae Muscle
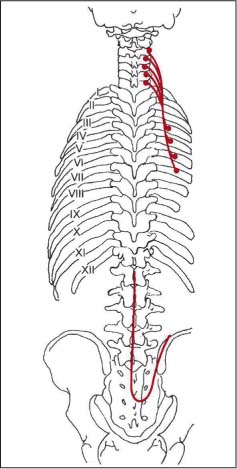
NMT 2 (Figs. I17.2a–c)
Indications
• Pain: Chronic pain in the neck region. Often the pain radiates toward the occiput and/or the region between the shoulder blades (a).
• Motion testing: Diminished upper cervical spine flexion with soft end-feel.
• Muscle testing: The levator scapulae muscle is shortened with characteristic pain on stretching. There is often associated suboccipital muscle shortening.
• Palpation: It is often difficult to test muscle length. A shortened levator scapulae muscle exhibits both muscle tension (texture) changes and “crepitations” that can be ascertained by palpating the distal muscle portion.
Patient Positioning and Set-up
• The patient is supine with the head beyond the examination table.
• The physician places one hand flat over the patient’s occiput. The other hand is placed under the patient’s scapula after having introduced maximal abduction and external rotation to the arm, locking the shoulder joint in this position.
• The cervical spine is flexed and rotated to the opposite side, introducing maximal stretch to the muscle (b).
Treatment Procedure
• The physician provides the resistant force to the patient’s elbow and spine of the scapula.
• Optimal isometric contraction of the levator scapulae muscle is performed by the patient.
• During the postisometric relaxation phase, passive stretch is introduced by pushing the scapula inferiorly and laterally via the patient’s arm (c).
• By engaging the cervical spine at its new barrier the muscle is stretched further.
• Starting from this new barrier, the stretching technique is repeated.
Note: Slight traction to the cervical spine should be maintained throughout the entire procedure.
Comments
• If dizziness or pain appears with positioning or during the treatment procedure itself, one should terminate this maneuver and examine and treat the cervical spine if indicated.
• If it is difficult to position the arm in abduction and external rotation, one should also be careful not to elevate the arm so as not to displace the shoulder inferiorly.
Rhomboid Major and Minor Muscles
Origin (Figs. 17.17–17.19)
• The rhomboid minor muscle arises via a short aponeurosis from the nuchal ligament at the C6 level and from the spinous process of C7. Some authors also describe a spine attachment at T1.
• The rhomboid major muscle arises from the spinous processes of T1 or T2 through T4. There may be a rudimentary origin at T5.
Insertion
Both muscles insert along the medial border of the scapula. The rhomboid minor muscle inserts at the level of the spine of the scapula above the rhomboid major muscle.
The insertion of the rhomboid major muscle starts where the inferiormost portion of the rhomboid minor ends. Its insertion occupies most of the medial border of the spine between the base of the scapular spine and the inferior angle of the scapula (Figs. 17.17–17.19).
Motor End Plates
The rhomboid minor and major muscles are nonpennate muscles. The motor end plate is located in the central portion of the muscle belly and its course is parallel to the muscle fiber direction between the muscle origin at the spinal aponeurosis and the insertion at the scapula (see Fig. 17.56).
Innervation
Nerve of the rhomboids (dorsal scapular nerve, C4 and C5).
Action
Theses two muscles adduct, elevate, and rotate or draw the scapula medially.
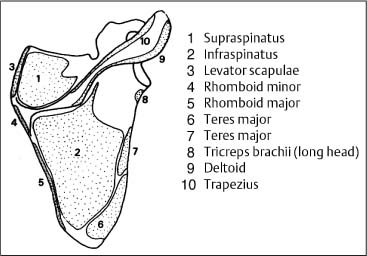
Fig. 17.17 Muscle attachments at the scapula.
Fig. 17.18 Course of rhomboid muscles.
Fig. 17.19 Rhomboid muscles.
1 Trapezius (on left)
2 Rhomboid minor
3 Rhomboid major
Palpatory Approach
The close proximity to the trapezius muscle (horizontal portion) requires that the palpating finger presses deeply, approaching the muscle from a lateral and inferior direction. A definitive differentiation is possible at the medial border of the scapula where the incriminated muscle can be palpated at its insertion (insertion tendinosis). Here the approach is medial and superior.
The patient is requested to spread the shoulders/scapulae apart against operator resistance (see Fig. 17.21).
SRS Correlation
A regional or segmental dysfunction in the lower cervical and/or upper thoracic spine may be associated with a prominent finding of palpable band or prominent extensive “myospasms” in the incriminated muscle.
Comments
Both of the rhomboid muscles often participate in the spondylogenic event. Clinically, patients localize their pain between the shoulder blades.
Strength Testing of the Medial Shoulder Blade Fixator Muscles
(Serratus posterior muscle, rhomboid muscles and trapezius muscle [horizontal portion].)
Examination Procedure
There are two variations, one with the patient standing and the other with the patient prone.
Variation 1: Standing
The patient stands with his back against the wall and abducts his arms to 90°. Keeping the trunk straight, the patient is then instructed to move both of his feet forward, about two foot lengths. Then the physician requests that the patient lift his trunk and shoulders off and away from the wall (about 2 cm) and to maintain this position as long as possible, for up to 30 seconds. A fit person and persons who exercise regularly should have no difficulty in performing this maneuver (Fig. 17.20).
Variation 2: Prone
Here, the arms of the prone patient are abducted at the shoulder. With his arms crossed, the examiner assesses the muscles at their insertion at the medial margin of the scapula. The patient is then requested to contract the muscles responsible for medial shoulder blade fixation, a maneuver performed by lifting the arms off the examination table (Fig. 17.21).
Fig. 17.20 Evaluation of muscle strength: endurance of the medial shoulder blade stabilizers. Patient standing and holding arms slightly abducted with elbows flexed to 90°.
Fig. 17.21 Evaluation of muscle strength of the medial shoulder blade stabilizers. Patient prone. Displace the shoulder blades laterally and then request patient to push them toward the midline.
Positive Findings
Variation 1: Standing
The patient may have difficulty maintaining this position and may actually begin to recruit additional respiratory muscles as it becomes increasingly difficult to breathe slowly (forced respiratory movements). This may alert the examiner that there could be weakness in the medial shoulder blade fixator muscles.
Variation 2: Prone
If the patient in the prone position has difficulty in displacing the shoulder blades medially (difficult to adduct and retract), it is usually due to prominent weakness of the medial shoulder blade fixator muscles.
Erector Spinae Muscle Group
The main mass of the back muscles can be divided into three groups of muscles. Most superiorly and medial is the spinalis group. The medial and middle groups are termed the longissimus. Most inferiorly and laterally is the iliocostalis group. The erector spinae muscles are also known as the sacrospinales muscles.
Origin; General Comments
At the pelvis, the longissimus and iliocostalis muscles cannot be differentiated from each other at their respective origins. Akin to a two-headed muscle, they share a common and rather broad origin. Their origins of the longissimus and iliocostalis muscles stretch from the spinous processes of all five lumbar vertebrae via the median sacral crest and the posterior portion of the sacrum in the S3–S4 region to the lateral sacral crest. They continue further to the medial and superior side of the iliac tuberosity, the short posterior sacroiliac ligaments, and the anterior side of the posterior part of the inner lip of the crest of the ilium (Figs. 17.22, 17.23, and 17.24).
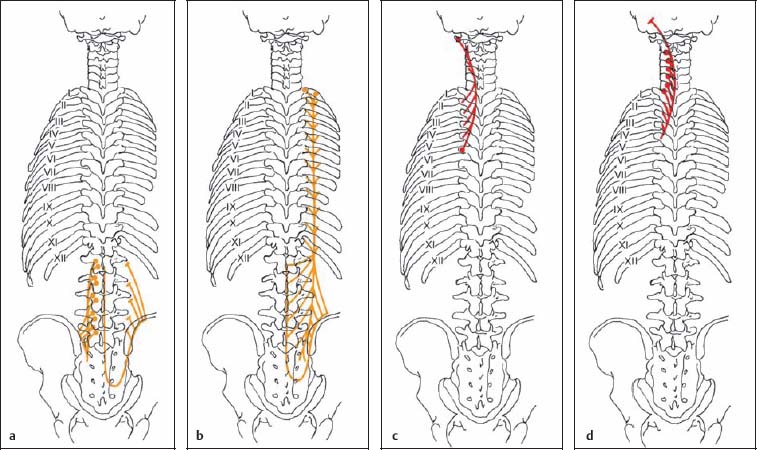
Fig. 17.22a–d Course of longissimus muscle—medial portion.
a Course of longissimus lumborum
b Course of longissimus thoracis
c Course of longissimus cervicis
d Course of longissimus capitis
Fig. 17.22e–g Course of iliocostalis muscle—lateral portion.
e Course of iliocostalis lumborum
f Course of iliocostalis thoracis
g Course of iliocostalis cervicis
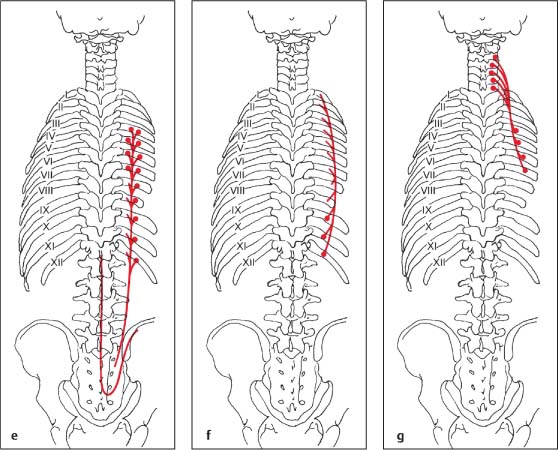
Fig. 17.23 Erector spinae muscles, superficial layer.
Fig. 17.24 Erector spinae muscles, deep layer.
Longissimus Lumborum Muscle
Origin
The longissimus lumborum muscle arises from the broad sacrospinous ligament primarily at the superior and anterior portions of the iliac tuberosity (Fig. 17.25).
Insertion
It inserts to all lumbar vertebrae via two rows, a lateral and medial row.
• A lateral row of broad insertions attaches to the entire inferior edge and spans the entire length of the posterior surface of the lumbar transverse processes. The insertion at L5 usually only reaches the iliolumbar ligament (Fig. 17.25).
• The medial row overlies the lateral row and converges toward the ligamentous fascia above the mamillary and accessory processes. The dorsal ramus of the spinal nerves is located beneath this fascia (Fig. 17.25).
Course and Relations
The longissimus lumborum muscle lies deep in relation to the iliocostalis and the longissimus thoracis muscles (see Fig. 17.24). By way of its origin at the iliac tuberosity, it connects to the interosseous sacroiliac ligaments.
Innervation
Dorsal ramus of the respective spinal nerve.
Fig. 17.25 Course of the longissimus lumborum muscle.
Left: Medial row
Right: Lateral row
Fig. 17.26 Palpation of the longissimus lumborum.
Action
Bilateral contraction results in extension of the vertebral column. Unilateral contraction results in side-bending of the spine to the side of the contracted muscle.
Palpatory Approach
Except in very rare cases, it is almost impossible to distinctly palpate the origin tendinoses of the longissimus lumborum muscle. Thus, the examiner must rely on the patient to report pain.
The lateral portion is stronger than the medial, and is palpated from a lateral and inferior direction (Fig. 17.26). The examiner must attempt palpatory differentiation between this muscle and the lateral lumbar intertransverse muscles, whereby it should be noted that these two muscles can develop myotendinoses (e. g., hard, palpable band) simultaneously (Fig. 17.27).
SRS Correlation
The insertions at the lateral and medial rows have different spondylogenic correlations. The lateral row of insertion is correlated with the first three sacral vertebrae. The medial row is correlated with the last cervical and the first four thoracic vertebrae.
Comments
The longissimus lumborum is a strong muscle. Myotendinosis of this muscle can easily lead to somatic or segmental motion restriction in one or several lumbar vertebrae. In the case of the “functionally unstable pelvis” (according to Sutter’s terminology), an abnormal position or vertebral dysfunction (e. g., somatic dysfunction) of the segments L1–L2 and L2–L3 can be brought about by the lateral insertions that are correlated with S1, S2, and L3. Due to the crossover of the SRS of LI, L2, and L3, a complex clinical picture can arise in the axial skeleton, as well as in the extremities.
Fig. 17.27 Palpation of the longissimus lumborum.
Muscle Length Testing
Examination Procedure
At first, the patient is sitting. The muscle contours are evaluated for symmetry and presence of any prominence. The patient is examined in the lateral recumbent (sidelying) position, both thighs flexed passively in order to introduce flexion to the lower spine. In this way, the range of motion can also be evaluated. Equally important is the evaluation of the end-feel (Fig. 17.28). Clinical evaluation of the longissimus lumborum muscle is difficult, however, and has proved to be of only limited value, especially when the procedure elicits pain.
If it is difficult to examine the patient in the side-lying position, then the patient can be evaluated in the seated position (Fig. 17.29).
Positive Findings
1. Prominent erector spinae muscle contours in the lumbar region with readily apparent increased tension in the standing patient may be an indication that the erector spinae muscle group is shortened.
2. Significant loss of flexion motion in the lumbar spine with a soft end-feel. The likelihood that the lumbar erector spinae muscle group is shortened increases proportionally with the degree of flexion motion loss in the lumbar area, especially when side-bending and extension motion are relatively preserved.
Fig. 17.28 Length testing of the longissimus lumborum.
Fig. 17.29 Length testing of the longissimus lumborum.
Longissimus Thoracis Muscle
Origin
The longissimus thoracis arises from the broad sacrospinous ligament primarily at the superior and anterior portions of the iliac tuberosity. Together with the longissimus lumborum it arises via a rather large sacrospinalis tendon (Figs. 17.30 and 17.31).
Insertion
The insertions are divided into a medial and a lateral row.
• The medial row of insertions is narrow and reaches the tips of the transverse processes of the thoracic vertebrae between T1 and T12 (Figs. 17.30 and 17.32).
• The lateral row of insertions is rather broad and reaches the ribs, in particular their inferior edge between the tubercle and costal angle (Fig. 17.30). Some of its superior portions are reinforced through other muscle segments originating from the mamillary processes of L1–L2.
Course and Relations
Muscle fibers originating at the iliac crest are destined for inferior insertions. Those arriving from the lumbar spinous processes and the median sacral crest are directed toward the middle and upper thoracic spine. The longissimus thoracis muscle lies lateral to the spinalis muscle and medial to the iliocostalis muscle, thus being on the midline over the thoracic transverse processes and lying lateral to the levatores costarum muscles and the ribs, reaching the line of the costal angle (Figs. 17.32 and 17.33).
Fig. 17.30 Course of the longissimus thoracis muscle.
Fig. 17.31 Origin of the longissimus thoracis muscle.
1 Longissimus thoracis
2 Iliocostalis lumborum
3 Internal abdominal oblique
4 Gluteus maximus
5 Gluteus medius
Innervation
Dorsal rami of the spinal nerves.
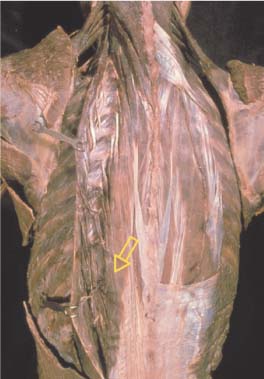
Motor End Plates
The lumbar and thoracic portions of the longissimus dorsi muscles are representative of a nonpennate muscle that has a number of motor end plates (Fig. 17.34).
Action
Bilateral contraction results in extension of the vertebral column. Unilateral contraction results in side-bending of the vertebral column to the side of the contracted muscle.
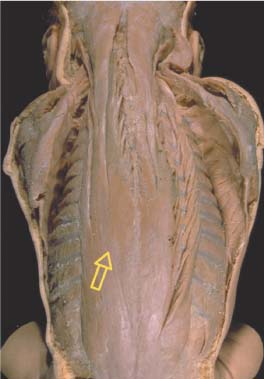
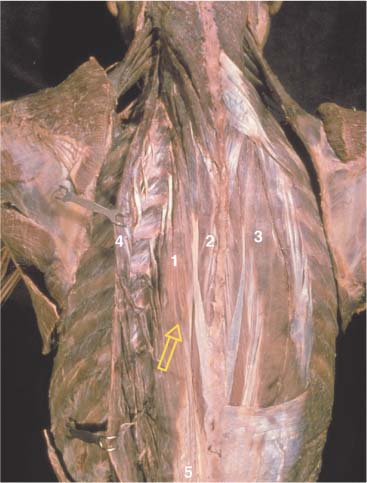
Fig. 17.32 Erector spinae muscles, deep layer.
1 Longissimus thoracis
2 Spinalis
3 Iliocostalis thoracis
4 Iliocostalis thoracis (reflected laterally)
5 Thoracodorsal fascia
Fig. 17.33 Erector spinae (superficial layer).
Fig. 17.34 Motor end plates of the superficial back muscles (with kind permission of Dr. J. Chomiak)
1 Longissimus thoracis et lumborum
2 Latissimus dorsi
3 Trapezius, pars ascendens
Palpatory Approach
Origins
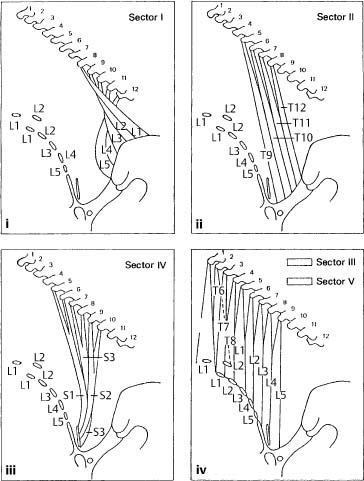
1. Sector I: The origin of sector I arises between the origins of the longissimus lumborum muscle on one side and the iliocostalis muscle on the other. The tendinoses at the iliac tuberosity and the intermediate line of the iliac crest are 4–8 mm broad. They are palpated posterosuperiorly in the direction of the iliac crest (differential diagnosis of the short sacroiliac ligaments).
2. Sector II: The tendinoses at the lateral sacral crest are also palpated posterosuperiorly (differential diagnosis: the long dorsal sacroiliac ligaments).
3. Sector IV: The origin is at the posterior aspect of the sacrum (S3–S4). These tendinoses are also 4–8mm broad and must be distinguished from the sacral zones of irritation (ventralization testing). The palpatory direction is posterosuperior following the muscle fiber direction.
4. Sectors III and V: The origins of these two sectors are located at the spinous processes of L1–L3 (at the median sacral crest). The palpatory direction is in accordance with the muscle fiber direction when performed at the correct palpatory level and with the proper pressure. At L1 and L2, the superior reinforcement (see above) of the mamillary processes must be considered. Palpatory technique is modified accordingly (Fig. 17.35a).
Insertion
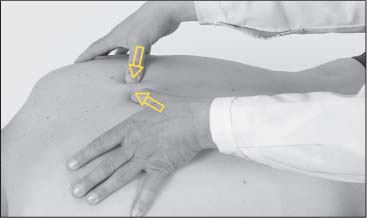
The palpatory approach is the same for all sectors: slightly lateroinferiorly from posterior in the direction of the inferior lateral margin of the transverse process (Fig. 17.35b).
The insertion tendinosis of the longissimus thoracis muscle is almost always accompanied by an irritation zone of the corresponding thoracic vertebra (result of myotendinosis).
At the ribs, the insertions are palpated inferiorly, i. e., between the tubercle and the costal angle at the inferior margin of the rib (comparison with the adjoining ribs is very important).
It is highly unlikely that the SRS correlation of these lateral lines of insertion is identical to that of the medial insertions. Since they have not been definitely categorized, they will not be discussed here. The muscle overlying the hard surface of the ribs and the spinous processes can easily be palpated perpendicular to the fiber direction. This allows for the differential diagnosis of the adjoining muscle layers.
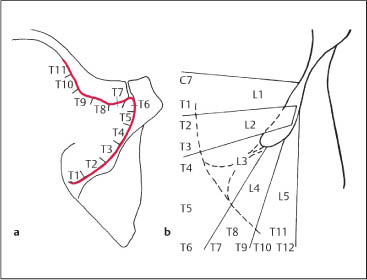
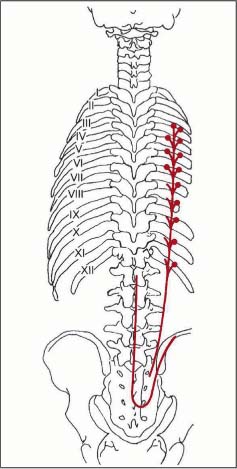
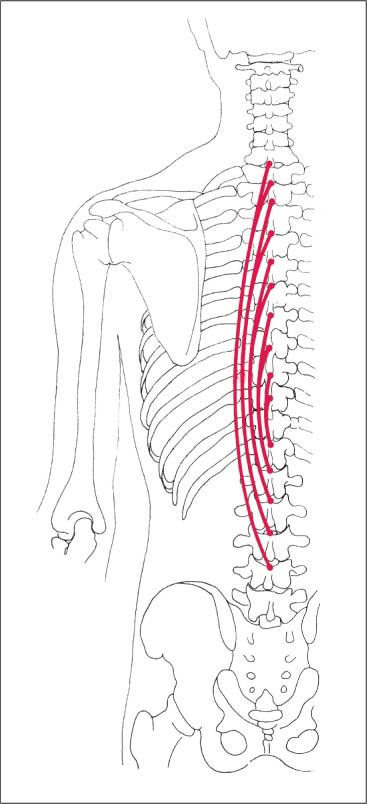
SRS Correlation
See the sector diagrams (Fig. 17.35a). The longissimus thoracis muscle is one of the most important muscles for the SRS. It responds rapidly to a segmental or regional dysfunction and thus can often be clinically found to undergo myotendinotic changes (e. g., hard, palpable band). It should not be difficult for the novice with little palpatory experience to detect the myotendinosis of the longissimus thoracis muscle and to correlate it correctly with the level of dysfunction.
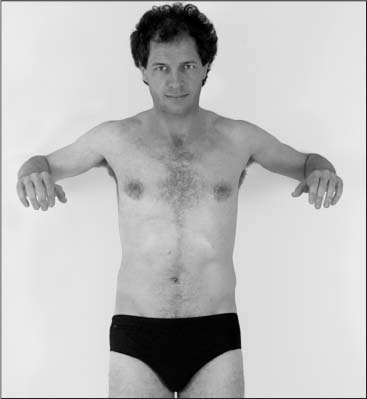
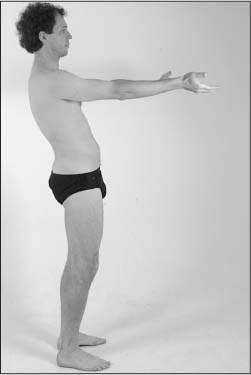
Muscle Endurance Test (Mathiass Test)
Examination Procedure
The standing patient is requested to raise the arms 90° in front and subsequently supinate the forearms so that the palms face horizontally upward. The patient should be as relaxed as possible and breathe slowly without forcing the respiratory movements (Fig. 17.36).
Positive Findings
1. If the patient has difficulty maintaining this position (e. g., the patient is unable to remain in one place), his postural muscles may be weak.
2. If the patient drops the arms without being able to maintain a maximally erect posture, it is most likely the result of postural insufficiency (Fig. 17.37).
3. The patient is either unable to maintain this position at all or only for a few seconds along with obvious asymmetry. This is probably due to significant postural de-compensation (Fig. 17.37).
Fig. 17.35 a Myotendinoses associated with the longissimus thoracis.
Fig. 17.35 b Palpation of the longissimus thoracis.
Fig. 17.36 Test to evaluate muscle endurance and strength in specific position.
Fig. 17.37 Test to evaluate muscle endurance and strength in specific position.
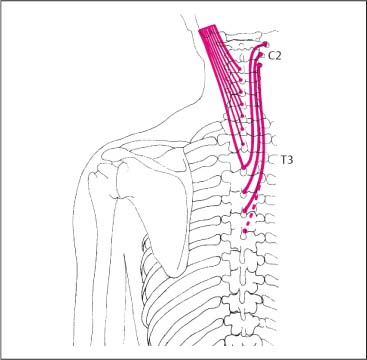
Longissimus Cervicis Muscle
Origin
Arises from upper six thoracic transverse processes, near to the center of the superior surface of the tip. On occasion the muscle may arise as inferiorly as T8 (Fig. 17.38).
Insertion
It inserts to the posterior surface and the root of posterior tubercles of the second to sixth cervical transverse processes, occasionally the atlas. It inserts practically together with the iliocostalis cervicis, splenius cervicis, levator scapulae, posterior scalene, and the longissimus capitis muscles.
Course and Relations
This is a flat and rather weak muscle with its main surface in the sagittal plane. At the T4–T5 level, it is often connected to the belly of the longissimus thoracis muscle via a tendon. In its lower half, it runs medially to the longissimus thoracis muscle. The muscle belly in the lower cervical region runs deeply and laterally to the longissimus capitis muscle, which in turn is lateral to the semispinalis capitis muscle. The muscle fiber direction is nearly perfectly longitudinal. The longissimus group and the semispinalis capitis muscle have their own muscular fasciae and can therefore easily be distinguished from each other by palpation (Fig. 17.39).
Innervation
Dorsal rami of the spinal nerve, the cervical nerves, and the thoracic nerves C3–T2.
Action
Bilateral contraction results in extension of the cervical spine. Unilateral contraction results in side-bending of the cervical spine to the side of the contracted muscle.
Palpatory Approach
The muscle belly is, as already described, easily palpable in the region of the lower cervical spine (perpendicular to the fiber direction).
The origins are palpated at the tip of the thoracic transverse processes from superior to inferior. It is very difficult to differentiate these origins from the semispinalis capitis and cervicis muscles. The insertion at the posterior tubercle of the costal transverse processes is palpated from inferior to superior.
SRS Correlation
Each origin to insertion unit represents one myotenone (i. e., always the most superior insertion together with the most superior origin).
Longissimus Capitis Muscle
Origin
The longissimus capitis muscle arises from the upper six thoracic transverse processes (T1–T6), together with the longissimus cervicis muscle, and from the articular processes of the lower four to five cervical vertebrae (C3 or C4 to C7). In the cervical spine the origins are medial to the insertions of the longissimus cervicis muscle and in the thoracic spine they arise medial to the origins of the longissimus cervicis muscle.
Insertion
The posterior margin of the mastoid process to its tip with a length of 1.5 cm (Fig. 17.41).
Course and Relations
The longissimus capitis muscle is a slender muscle oriented in the sagittal plane. The longitudinal muscle bundles arise most inferiorly at the anterior edge of the muscle belly. In the cervical spine, the deep layer of the muscle can be relatively easily palpated between the semispinalis capitis and the longissimus cervicis muscles. At its insertion, the longissimus cervicis muscle is covered by the splenius capitis muscle and the sternocleidomastoid muscle (Figs. 17.39 and 17.40).
Innervation
Dorsal rami of the corresponding cervical nerves C1–C3, possibly C4.
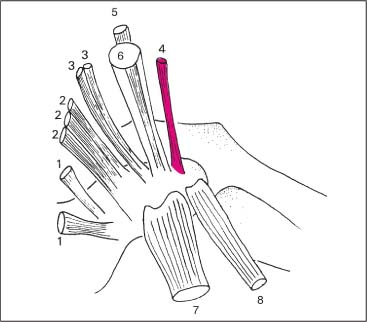
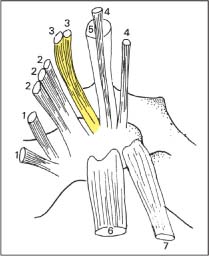
Fig. 17.38 Muscle attachments at the tip of the thoracic transverse process.
1 Rotatores
2 Multifidus
3 Semispinalis cervicis
4 Longissimus cervicis
5 Longissimus capitis
6 Semispinalis capitis
7 Longissimus thoracis
8 Levator costae
Fig. 17.39 Longissimus cervicis.
Fig. 17.40 Longissimus capitis.
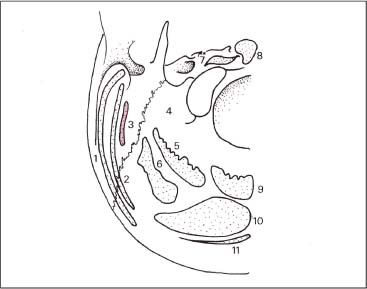
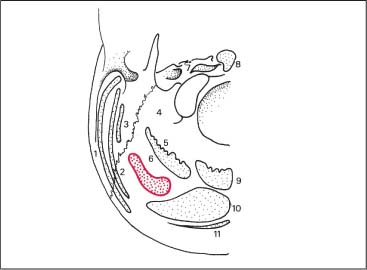
Fig. 17.41 Muscle attachments at the occiput.
1 Sternocleidomastoid
2 Splenius capitis
3 Longissimus capitis
4 Rectus capitis lateralis
5 Rectus capitis posterior major
6 Obliquus capitis superio
7 Rectus capitis anterior
8 Longus capitis
9 Rectus capitis posterior minor
10 Semispinalis capitis 11 Trapezius
Action
Bilateral contraction results in extension of the head. Unilateral contraction results in side-bending and rotation of the head to the side of the contracted muscle.
Palpatory Approach
The muscle belly can easily be palpated perpendicularly to the fiber direction in the deep layers of the lower cervical spine between the semispinalis capitis and the longissimus muscles.
The insertion at the mastoid is palpated beneath the splenius capitis muscle and the sternocleidomastoid muscle from an initial posterior and inferior position following the muscle in a superior direction (Fig. 17.41). The origins are palpated from superior to inferior approaching the roots of the corresponding transverse processes.
SRS Correlation
Similar to the longissimus cervicis muscle, each origin to insertion unit of the longissimus capitis muscle represents one myotenone. The various muscles are differentiated from each other at their origins and the respective irritation zones.
Iliocostalis Muscle
The most lateral upward continuation of the erector spinae group is termed the illiocostalis system. This system has three linear and overlapping portions, the lumborum, thoracis and cervicis.
Iliocostalis Lumborum Muscle
Origin
Arises from the broad sacrospinous ligament and the ante-rolateral surface of the iliac tuberosity (Fig. 17.42).
Insertion
Inserts at the costal angle of the lower ribs, about IV–XII (Fig. 17.43).
Iliocostalis Thoracis Muscle
Origin
Arises medially at the costal angle of the lower ribs, about IV–XII (Figs. 17.42 and 17.44).
Fig. 17.42 Course of erector spinae muscles. 1 Iliocostalis 2 Longissimus dorsi 3 Latissimus
Insertion
Inserts laterally at the costal angle of the upper ribs, VII–I (Fig. 17.44)
Iliocostalis Cervicis Muscle
Origin
Arises directly medial to the costal angle of the upper ribs, III (IV)–VII (Fig. 17.45).
Insertion
Inserts at the posterior tubercles of the transverse processes of C3 and C4 to C6 (refer to the insertion of the longissimus cervicis muscle) (Fig. 17.45)
Course and Relations
The iliocostalis muscle (Fig. 17.42) shows a roof-tile arrangement. The iliocostalis lumborum muscle ascends from inferior, traverses the posterior surfaces of the ribs going superiorly, and runs lateral to the longissimus thoracis muscle. In the neck, the iliocostalis cervicis muscle also lies lateral to the longissimus cervicis and capitis muscles, and medial to the posterior and medial scalene muscles, as well as the levator scapulae muscle. Its main course is in the sagittal plane. The iliocostalis cervicis muscle can be isolated anatomically but should be viewed as the direct continuation of the iliocostalis lumborum muscle (Figs. 17.43–17.45).
Innervation
Dorsal rami of the corresponding spinal nerves.
Action
Bilateral contraction results in extension of the spine. Unilateral contraction results in side-bending of the spine toward the side of the contracted muscle.
Palpatory Approach
At its origin, the iliocostalis lumborum muscle (Fig. 17.46) cannot be distinguished from the tendon of the longissimus dorsi muscle. In its course, the iliocostalis muscle is found lateral to the longissimus dorsi muscle. Inferiorly, it is possible to palpate the insertion tendinoses at the inferior edge and the posterior surface of the costal angle (Fig. 17.47). To avoid contact with the levator costae muscle, the direction must be perfectly inferior.
The iliocostalis cervicis muscle is relatively accessible to palpation. Following the costal angle of the ribs, the origins are approached by starting medially and superiorly and moving laterally and inferiorly. The insertions are palpated from inferior to superior at the posterior tubercles of the cervical transverse processes.
Fig. 17.43 Iliocostalis lumborum.
Fig. 17.44 Iliocostalis thoracis.
Fig. 17.45 Iliocostalis cervicis.
Fig. 17.46 Palpation of the iliocostalis lumborum.
Fig. 17.47 Palpation of the iliocostalis lumborum.
While palpating the iliocostalis muscle, the examiner will need to differentiate between the other muscles inserting at this location, including the longissimus cervicis and the levator scapulae muscles (at C3–C4), as well as the medial and posterior scalenes, and the medial portion of the posterior cervical intertransverse muscles.
SRS Correlation
The spondylogenic correlation of the iliocostalis muscle is still undetermined. There are indications that the iliocostalis cervicis muscle is correlated with the myotenone L5.
Spinalis Muscle
Three muscles make up the spinospinal system:
• Spinalis capitis muscle
• Spinalis cervicis muscle
• Spinalis thoracis muscle.
As the name readily implies, these muscles interconnect the spinous processes. However, they have a great variability in their distribution. When present, the spinalis capitis muscle is fused anatomically with the semispinalis muscle.
The discussion is restricted to the spinalis thoracis muscle, which is the only one of clinical importance in the field of manual medicine. It is a slender muscle in the mid-thoracic region.
Spinalis Thoracis Muscle
Origin
Spinous processes between T11 and L2 or L3 (Fig. 17.48).
Insertion
Tips of the spinous processes between C7, and T1 through T9 (Fig. 17.49).
Course
The longest fascicles run from L3 to C7 and T1. The shortest fascicles run from T11 to T8 or T9. This arrangement results in the largest muscle profile in the lower thoracic region. The fibers can be palpated above the tips of the transverse processes (when myotendinosis [e. g., hard palpable band] is present) (Figs. 17.50 and 17.51).
Innervation
Dorsal rami of the thoracic nerves T6–T8.
Action
Bilateral contraction results in extension of the vertebral column. Unilateral contraction results in side-bending (lateral flexion) of the vertebral column.
Palpatory Approach
The origin tendinosis of the spinalis thoracis muscle is palpated from a superior direction in order to reach the proximal pole of the spinous process. It must be differentiated from the adjoining origin tendinoses, for instance, that of the latissimus dorsi muscle in the lumbar region and the serratus posterior inferior muscle in the upper thoracic and cervical region (Fig. 17.52).
SRS Correlation
The spinalis muscle is spondylogenically and reflexogenically correlated with the lumbar spine.
Comments
As already noted, the spinalis cervicis and capitis muscles are nonuniform and, for all purposes, spondylogenically and reflexogenically insignificant.
Fig. 17.48 Origin of the spinalis muscle.
Fig. 17.49 Attachment of the spinalis muscle.
Fig. 17.50 Course of the spinalis muscle.
Fig. 17.51 Erector spinae (deep layer).
1 Longissimus thoracis
2 Spinalis
3 Iliiocostalis thoracis
4 Iliocostalis thoracis (reflected laterally)
Fig. 17.52 Palpation of the spinalis muscle.
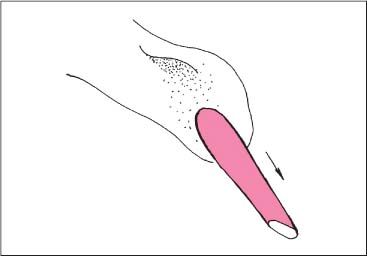
Treatment of Erector Spinae Muscles in the Lumbar Region
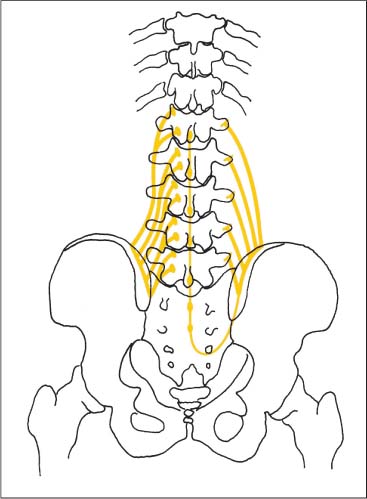
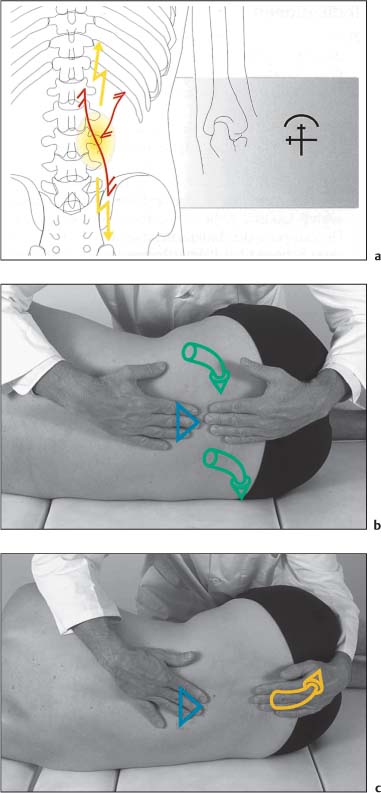
NMT 2 (Figs. I17.3a–c)
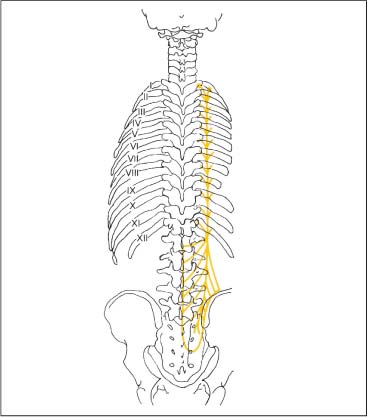
Indications
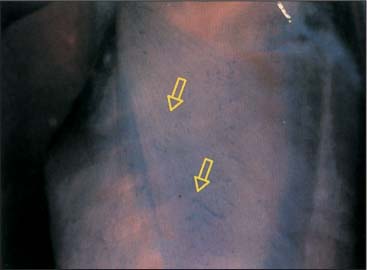
• Pain: Pain that is localized to the patient’s back; this can be chronic or acute and may radiate into the legs (a).
• Motion testing: Lumbar spine flexion and side-bending restriction with soft end-feel.
• Muscle testing: The erector spinae muscle is shortened and its contours become rather prominent. The psoas major and quadratus lumborum muscles are often shortened and the abdominal muscles are weak. Furthermore, there may coexist a segmental dysfunction in the lumbar spine or the pelvis, and there may be concurrent hip joint disease (a).
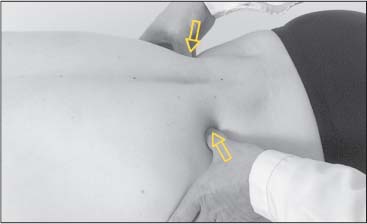
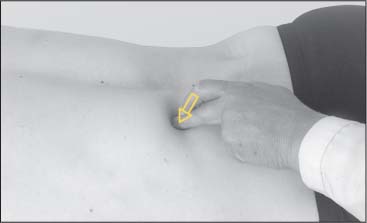
Patient Positioning and Set-up
• The patient is in the side-lying position.
• The muscle is maximally stretched by flexing the lumbar spine, hip, and knee joints.
• The physician places one hand flat over the sacrum and the other over the spinous processes in the mid-lumbar spine (b).
Treatment Procedure
• During inhalation the patient is instructed to isometrically contract the erector spinae as much as possible (b).
• During the postisometric relaxation phase, passive stretch is introduced by the physician by further flexing of the lumbar spine and simultaneous traction applied to the sacrum.
• Since the hip joints are increasingly flexed with this maneuver, pelvic flexion is therefore introduced as well, which further assists in indirectly increasing the stretch (c).
Comments
Since the isometric contraction of the erector spinae muscles requires a high degree of proprioceptive control, the specific movements should initially be performed by the patient under supervision and if necessary through palpatory/factile guidance by the physician.
Splenius Muscles
This is a flat muscle that typically divides at its origin into the splenius capitis and splenius cervicis muscles. These muscles lie in the cervical region, deep to the trapezius and rhomboid muscles.
Splenius Capitis Muscle
Origin
Arises from the lower half of the nuchal ligament, and from the spinous processes of C7 and T1–T3 (Fig. 17.54).
Insertion
Inserts at the lateral surface of the mastoid process, including its tip, and the occipital bone of the skull. This insertion forms a posterior arch that reaches the lateral half of the superior nuchal line (Figs. 17.53, 17.54).
Splenius Cervicis Muscle
Origin
Arises from the spinous processes and the supraspinous ligaments of T3–T10. The length of the tendons increases inferiorly. The parallel muscle bundles form a long, slender belly that is more vertical than that of the splenius capitis muscle and swings around the neck superolaterally (Fig. 17.54).
Insertion
Inserts via three tendons of disproportionate size at the first three cervical vertebrae. The largest fascicle inserts at the posteroinferior portion of the tip of the transverse process of the atlas. The second largest inserts at the tip of the transverse process of the axis, and the third inserts at the posterior surface of the transverse process of C3 (Fig. 17.54).
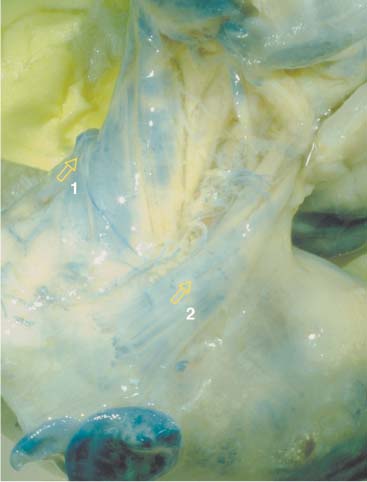
Course and Relations
The trapezius, the rhomboid, and the serratus posterior superior muscles cover a broad section of the inferior and medial portions of the splenius muscle. The sternocleidomastoid and the levator scapulae muscles cover the splenius muscle superiorly and laterally. The splenius muscle overlies the semispinalis capitis muscle. Many parts of the inserting tendons of the splenius cervicis muscles are fused with the tendons of the levator scapulae and the longissimus cervicis muscle. The free medial border of the splenius capitis muscle forms together with the nuchal ligament and the medial end of the superior nuchal line, a triangular space through which the occipital vessels and the greater occipital nerve emerge (Fig. 17.55).
Innervation
Dorsal rami of the cervical nerves C1–C5.
Action
Bilateral contraction results in extension of the head and the cervical spine. Unilateral contraction results in side-bending and rotation of the head toward the side of the contracted muscle.
Palpatory Approach
Due to its rather flat shape, the splenius muscle is not easily accessible to direct palpation. Palpation starts by identifying the spinous process of C3 superolaterally. While staying relatively superficial, the examiner follows inferiorly along C4–C5 to T5–T6. In the more inferior segments, the palpatory direction is primarily vertical. The inserting portion of the splenius capitis muscle is palpated inferiorly at the lateral surface of the mastoid process and is then followed along a curve that reaches the superior nuchal line. The largest tendon insertion of the splenius cervicis muscle is palpated posteroinferiorly, by approaching the tip of the transverse process of the atlas. The tendon insertions leading to C2 and C3 are substantially weaker and are palpated from a posteroinferior direction as well.
SRS Correlation
Both the splenius capitis and the splenius cervicis muscles are correlated with C7 as a single myotenone.
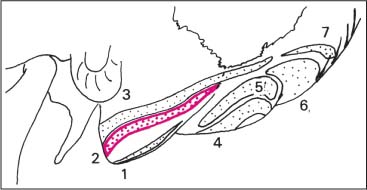
Motor End Plates
The splenius capitis muscle is a nonpennate muscle with a number of motor end plate zones, that correlate with their respective segmental innervation (Fig. 17.56).
Fig. 17.53 Muscle attachments at the mastoid process and occiput.
1 Longissimus capitis
2 Splenius capitis
3 Sternocleidomastoid
4 Rectus capitis posterior major
5 Obliquus capitis superior
6 Semispinalis capitis
7 Trapezius
Fig. 17.54 Left: Splenius capitis. Right: Splenius cervicis.
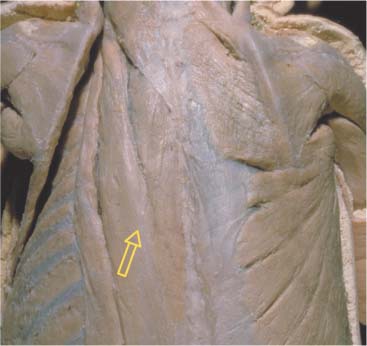
Fig. 17.55 Splenius muscles—course and relations.
1 Splenius capitis
2 Splenius cervicis
3 Serratus posterior superior
4 Levator scapulae
Fig. 17.56 Motor end plates (with kind permission of Dr. J. Chomiak).
1 Splenius capitis
2 Trapezius
3 Rhomboid major
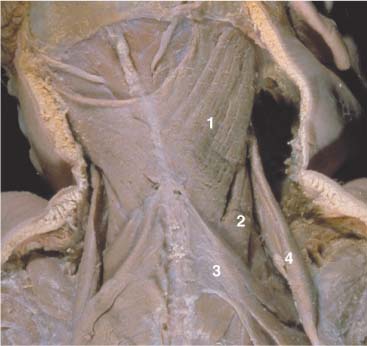
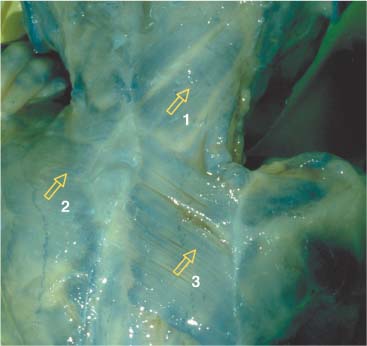
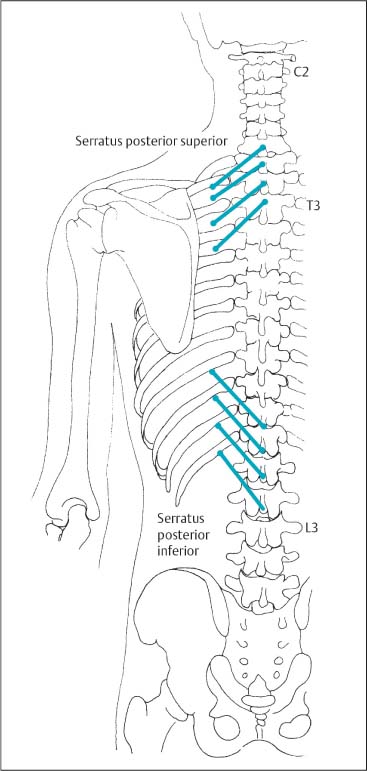
Posterior Serratus Muscles
The serratus posterior muscles lie in the upper and lower thoracic regions, between the muscles of the upper extremity and the other muscle groups of the back (erector spinae, transversospinalis, segmental).
Serratus Posterior Superior Muscle
Origin
The muscle arises from the nuchal ligament close to the spinous process of C6 and from the tips of the spinous processes of C7, T1, and T2 (Figs. 17.57, 17.58).
Insertion
The muscle inserts via four fascicles at ribs II–V, lateral to the costal angles.
Course and Relations
This is a deep muscle that extends from the spinous processes to the ribs at an angle of about 30° and is primarily covered by the rhomboid and the trapezius muscles (Figs. 17.57, 17.58).
Innervation
Intercostal nerves of T1–T4.
Action
Rib elevation.
Palpatory Approach
Using an anterior and inferior approach, this deep muscle can only be palpated at the spinous processes, which requires that one localizes any insertion tendinoses. The latter must be differentiated from the spondylogenic correlation with the rhomboid muscle.
Fig. 17.57 Posterior serratus muscles—course and relations.
1 Serratus posterior superior
2 Serratus posterior inferior
Serratus Posterior Inferior Muscle
Origin
Arises from the spinous processes and the supraspinous ligament at T11–L2, occasionally L3. The tendon of the origin of the serratus posterior inferior muscle is virtually identical with the superficial layer of the thoracolumbar fascia and the lumbar aponeurosis of the latissimus dorsi muscle (origin) (Fig. 17.57, 17.58).
Insertion
The serratus posterior inferior muscle inserts by four fascicles at the inferior margin of ribs IX–XII between the origins of the latissimus dorsi and the iliocostalis muscles. The most lateral fibers travel to the ninth rib almost horizontally.
Course and Relations
This muscle, which shows a near-perfect horizontal course, is only covered by the latissimus dorsi muscle. The tendon and muscle junction is located at the lateral edge of the iliocostalis muscle, where a painful myotendinosis can often be found.
Innervation
Intercostal nerves T9–T12.
Action
When contracted, the muscle keeps the lowermost four ribs in place while resisting diaphragm contraction. Thus, it is considered an accessory respiratory muscle facilitating inhalation.
Palpatory Approach
Even though the serratus posterior inferior muscle is completely covered by the latissimus dorsi muscle, the presence of a myotendinosis may be palpated without much difficulty.
The palpatory direction is perpendicular to the fiber direction, from inferior to superior. The insertion tendinoses are located at the ribs about four finger-widths lateral to the spinous processes.
SRS Correlation
The serratus posterior and inferior muscles each represent a single individual myotenone. Segmental dysfunction of the first thoracic vertebra may cause muscle changes that can be palpated as a tight muscle band in the serratus posterior superior muscle. Similarly, segmental dysfunction of the first lumbar vertebra can lead to changes in muscles that are palpable as a tight band in the serratus posterior inferior muscle.
Fig. 17.58 Course of the serratus muscles.
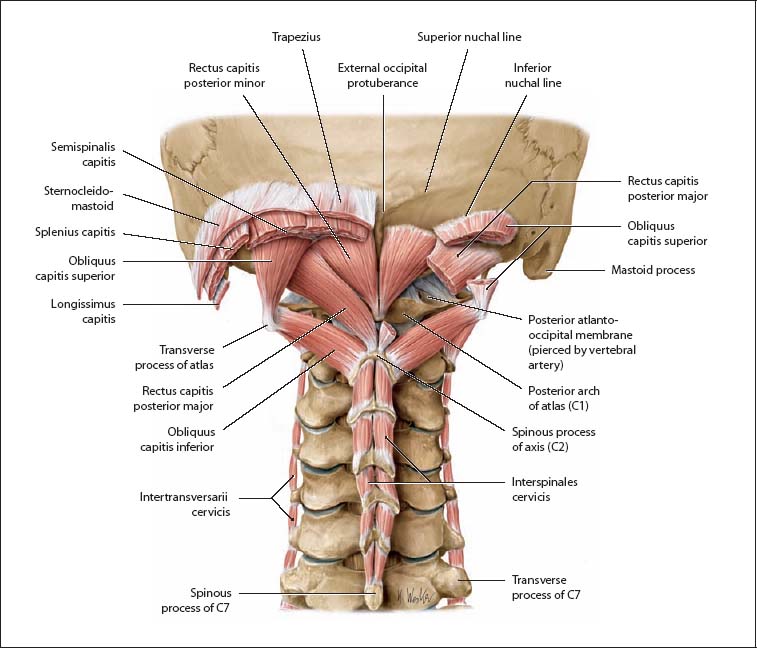
Suboccipital Muscles (Overview)
Fig. 17.59 Location of the short nuchal muscles (suboccipital muscles). Nuchal region, posterior aspect. (From Schuenke, Thieme Atlas of Anatomy Vol. I, 2007.)
Fig. 17.60 Course of the short nuchal muscles.
Suboccipital region, posterior view. The rectus capitis posterior major and obliquus capitis superior muscles on the right side have been partially removed. (From Schuenke, Thieme Atlas of Anatomy Vol. I, 2007.)
The suboccipital muscles in the strict sense are the short or deep nuchal muscles that belong to the intrinsic back muscles (recti capitis posteriores major and minor and obliquii capitis superior and inferior). They meet the criterion of being innervated by a dorsal ramus−in this case the C1 dorsal ramus, the suboccipital nerve. Thus the recti capitis anterior and lateralis are not classified as intrinsic back muscles, despite their suboccipital location, because they are innervated by ventral rami. The short or deep nuchal muscles lie within the thoracolumbar fascia deep at the back of the neck and course between the occiput and the first two cervical vertebrae. They act mainly on the craniovertebral joints and support differentiated head movements (e. g., for fine adjustments of head position). The following muscles have been partially removed to demonstrate their location in the right nuchal region: trapezius, sternocleidomastoid, splenius capitis, and semi-spinalis capitis. An important landmark in the deep nuchal region is the spinous process of the axis.
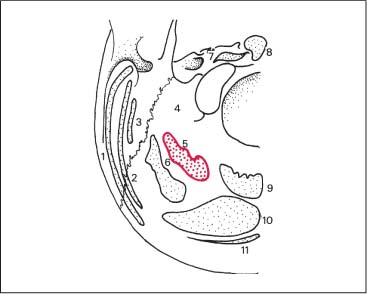
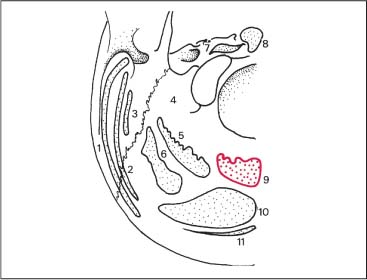
Rectus Capitis Posterior Major Muscle
Origin
The rectus capitis posterior major arises from the spinous process of the axis (its lateral and superior half), and has a pointed tendinous origin. The thick muscle belly takes on a triangular shape, with its muscle bundles spreading toward the skull. In this arrangement, the muscle fibers are twisted so that those bundles originating most anteriorly have their insertion medially (Fig. 17.88).
Insertion
On the occiput, the lateral half of the inferior nuchal line (Fig. 17.61).
Course and Relationships
The rectus capitis posterior major muscle courses from its origin obliquely and superolaterally to the occiput and is primarily superimposed by the trapezius muscle (descending portion) and the semispinalis capitis muscle (Fig. 17.63).
Innervation
Dorsal rami of the spinal nerves C1 and C2.
Fig. 17.61 Rectus capitis posterior major (muscle attachments at the occiput).
1 Sternocleidomastoid
2 Splenius capitis
3 Longissimus capitis
4 Rectus capitis lateralis
5 Rectus capitis posterior major
6 Obliquus capitis superior
7 Rectus capitis anterior
8 Longus capitis
9 Rectus capitis posterior minor
10 Semispinalis capitis
11 Trapezius
Action
Bilateral contraction results in extension of the head. Unilateral contraction results in side-bending (lateral flexion) with rotation of the head toward the side of the contracted muscle.
Palpatory Approach
This muscle is easily palpated. Starting from the mastoid process, the finger presses deeply under the semispinalis capitis muscle. The fleshy insertion presents itself in a region of 1 × 0.5 cm below the lateral third of inferior nuchal line. The obliquus capitis superior muscle covers the lateral portion of the insertion, and the medial portion is covered by the lateral part of the semispinalis capitis muscle. Palpation of the origin is according to the anatomical position. The palpatory direction is from superomedial to inferolateral.
SRS Correlation
The whole rectus capitis posterior major muscle represents a single myotenone and is correlated with the sacroiliac joint.
Comments
Myotendinosis of the rectus capitis posterior major muscle may influence the mechanics of the occipital-atlanto-axial joints via its origin at the spinous process of C2.
Rectus Capitis Posterior Minor Muscle
Origin
Arises from the posterior tubercle of the atlas (Fig. 17.64).
Insertion
Inserts on the occipital bone, between the medial third of the lower nuchal line and the external margin of the occiput (Fig. 17.62).
Course and Relations
Covered mainly by the trapezius and splenius muscles (descending portion) as well as the semispinalis capitis muscle (medial portions) (Fig. 17.63).
Innervation
Dorsal rami of the spinal nerves C1 and C2.
Action
The main action of this short-lever muscle is that of posture and stabilization of the atlanto-occipital joint. Bilateral contraction results in extension of the head, and unilateral contraction results in lateral bending to the side of the contracted muscle.
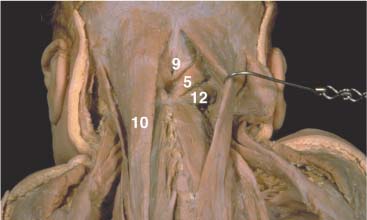
Palpatory Approach
About 2 cm below the external occipital protuberance the palpating finger presses deeply, but very carefully, between the two semispinalis capitis muscles. The palpatory direction is such that one starts inferiorly, then goes from medial to lateral. Palpation of the origin at the posterior tubercle of the atlas is done at its usual anatomic location (Fig. 17.64).
SRS Correlation
This occipital muscle also represents a single myotenone.
Comments
Myotendinotic changes (i. e., palpable bands) in the rectus capitis posterior minor muscle can influence the normal physiologic motion in the atlanto-occipital joints.
Clinical Pearl
From this position one can use NMT2, where the patient’s head is resting in the examiner’s hand. The patient is asked to push downward into the hand against equal resistance and, during the relaxation phase, the head is carried more anteriorly in a stepwise fashion with each repetition of this step. It is surmised that with this procedure one is also able to potentially “induce” stretching of the nuchal ligament.
Fig. 17.62 Rectus capitis posterior minor (muscle attachments at the occiput.
1 Sternocleidomastoid
2 Splenius capitis
3 Longissimus capitis
4 Rectus capitis lateralis
5 Rectus capitis posterior major
6 Obliquus capitis superior
7 Rectus capitis anterior
8 Longus capitis
9 Rectus capitis posterior minor
10 Semispinalis capitis
11 Trapezius
Fig. 17.63 Suboccipital neck muscles.
5 Rectus capitis posterior major
9 Rectus capitis posterior minor
10 Semispinalis capitis
12 Obliquus capitis inferior
Fig. 17.64 Suboccipital muscles
1 Obliquus capitis inferior
2 Obliquus capitis superior
3 Rectus capitis posterior major
4 Rectus capitis posterior minor
Obliquus Capitis Superior Muscle
Origin
This muscle originates from the transverse process of the atlas, in thick tendinous fibers from the posterior corner and the lateral segment of the C1 transverse process (Figs. 17.67).
Insertion
Inserts into the occipital bone at the superior to the lateral third of the inferior nuchal line (Fig. 17.65).
Innervation
Dorsal rami of C1.
Action
Bilateral contraction results in extension of the head. Unilateral contraction results in side-bending of the head toward the side of the contracted muscle.
Palpatory Approach
The origin is palpated inferiorly, below the most lateral insertion of the semispinalis capitis muscle (about 3 cm lateral to the external occipital protuberance). The origin is palpated superoposteriorly in the direction of the tip of the transverse process of the atlas (Fig. 17.66).
SRS Correlation
The posterior cervical intertransverse muscles and the obliquus capitis superior muscle play an important role in the spondylogenic event.
Even though the obliquus capitis superior muscle belongs anatomically to the posterior cervical intertransverse muscle group, it has been reported that it is spondylogenically and reflexogenically correlated with the sacroiliac joint.
Obliquus Capitis Inferior Muscle
Origin
The spinous process of the axis.
Insertion
The transverse process of the atlas, along the inferior and posterior surface.
Course and Relations
Refer to Figures 17.63 and 17.67.
Fig. 17.65 Muscle attachments at the occiput (see Fig. 17.62 for specific muscles).
Fig. 17.66 Palpation of the obliquus capitis superior.
Innervation
Dorsal rami of the spinal nerves C1 and C2.
Action
Rotation of the head to the side of the contracted muscle.
Palpatory Technique
The origin is palpated laterally at the spinous process of C2 according to the direction of the muscle fibers. The insertion, at the transverse process of the atlas, is palpated medioinferiorly. To evaluate the muscle origin and insertion, it is important to be at the correct palpatory depth. It is very difficult to distinguish tendinosis of the insertion from the zone of irritation. Myotendinotic changes in the muscle belly (i. e., hard, palpable band) appear in the sub-occipital soft tissues as a perpendicular, laterosuperiorly directed spindle.
SRS Correlation
The entire muscle is correlated with the sacroiliac joint as a single myotenone.
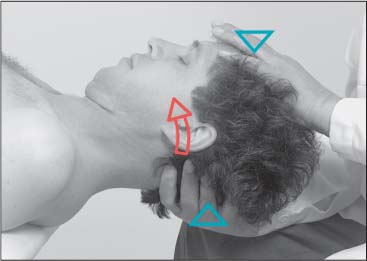
Length Testing of the Suboccipital Muscles
Examination Procedure
The patient is in the supine position. The examiner cradles the patient’s head by placing one palm over the patient’s occiput while the other embraces the forehead. The examiner then carefully introduces flexion to the upper cervical spine, specifically inclination to the upper cervical spinal segments, while at the same time applying traction. The axis of rotation is hypothetically placed through both mastoid processes (Fig. 17.68).
Positive Findings
1. Loss of inclination motion with soft end-feel indicates shortening of the suboccipital muscles.
2. Loss of inclination motion with hard end-feel indicates degenerative joint changes.
Fig. 17.67 Suboccipital muscles.
1 Obliquus capitis inferior
2 Obliquus capitis superior
3 Rectus capitis posterior major
4 Rectus capitis posterior minor
Fig. 17.68 Length testing of the suboccipital muscles.
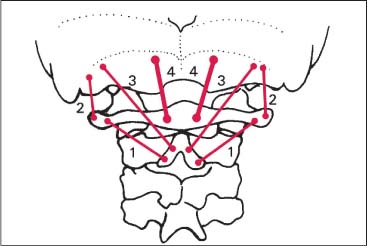
Transversospinalis Muscle Group (Semispinalis, Multifidus, Rotatores)
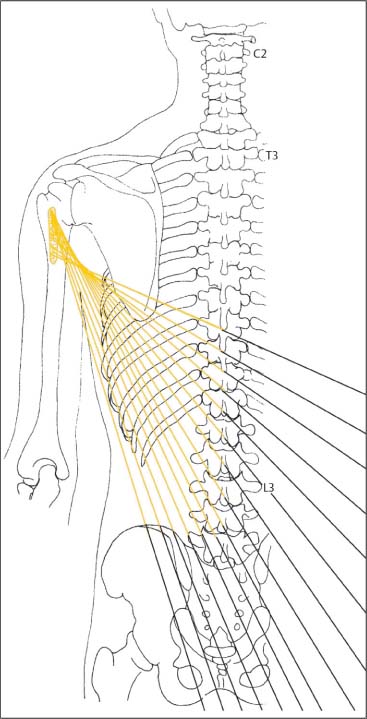
Semispinalis Muscle – Overview
Spanning from the sacrum to the upper cervical spine, the semispinalis muscle is a long and rather flat muscle that is made up of many divergent fascicles. From superior to inferior, the muscular units overlap each other in a roof-tile manner. Starting at the axis and going inferior, the characteristic feature of the transversospinal muscle system is determined by the muscle’s shape and varying length: the muscle fibers originate from an individual transverse process but then the various muscle slips fan out to attach at several spinous processes. which explains the different lengths. The superficial portions are the longer muscle sections with the fibers running nearly vertically. The deeper muscle portions are the shorter components of the muscle with the fibers extending in a transverse direction (Figs. 17.69, 17.70).
Semispinalis Lumborum Muscle
Origin
The muscle arises by a strong fascia from the mamillary processes of S1, L5, and L2.
At L1 and T12, the muscles originate directly from the vertebra’s mamillary processes.
Fig. 17.69 Semispinalis muscle.
Insertion
It inserts as long tendons at the inferior portions of the two spinous processes that are positioned six and seven segments superior to the vertebra from which the myotenone originates. The anatomic muscle unit of the semispinalis muscle described here is identical to the spondylogenic unit, the myotenone.
Semispinalis Thoracis and Cervicis Muscles
Origin
From the superior edge of the transverse processes.
• Thoracic portion: superior margin of the transverse processes of T6 through T10.
• Cervical portion: the superior margin of the transverse processes of upper thoracic vertebrae, T2 through T5 (Fig. 17.71).
Fig. 17.70 Semispinalis muscle—course and relations.
1 Semispinalis capitis
2 Semispinalis cervicis
3 Semispinalis thoracis
4 Spinalis
5 Longissimus, thoracic region
Insertion
The structure of the myotenone remains the same as described previously. The insertions are found at the spinous processes, which are six to seven segmental levels higher than the vertebra from which the myotenone originates. The insertion tendinosis is most prominent at the medial and posterior margin of the muscle (Figs. 17.69, 17.71).
Course and Relations
All three semispinalis muscles are positioned at the same level. The superior surface is covered by the longissimus muscle and the spinalis muscle, and partially by the semi-spinalis capitis muscle (Fig. 17.70). A thin connective-tissue layer demarcates this muscle from the multifidus muscle below, which is important for palpation. Differentiation from the multifidus muscle is facilitated by recalling that the longest portions of the multifidus muscle skip two fewer vertebrae than the semispinalis muscle.
Innervation
Dorsal rami of the spinal nerves.
Action
Bilateral contraction results in extension of the vertebral column. Unilateral contraction results in contralateral rotation of the vertebral column.
Palpatory Approach
Due to its frequent spondylogenic participation, exact palpation of the transversospinal system is extremely important. As a result of the close anatomical arrangement at the mamillary or transverse processes, it is difficult to distinguish between a tendinosis at the origin of the semispinalis muscle, and other muscles including the multifidus muscle and the rotator muscles. Only when the attachment tendinoses are present at both poles of the muscle is differentiation possible.
The rotator muscles pass from one vertebra to the first or second above (be aware of the difference between the anatomical and spondylogenic units). The multifidus muscle passes from one vertebra to the third above and inserts via three fascicles. The semispinalis muscle extends from one vertebra to the sixth above and inserts via two fascicles. When a painful superior margin of the mamillary bodies is located, all seven spinous processes must be palpated from their lateral aspect to the root in order to eliminate the rotatores muscles and the multifidus muscle as the source of the dysfunction and pain.
The origin tendinosis is determined to belong to the semispinalis muscle when the insertion is on opposite poles and lies six to seven segmental levels above the roots of the spinous process. The myotendinosis of the individual muscle fibers can normally be palpated as a thin matchlike band.
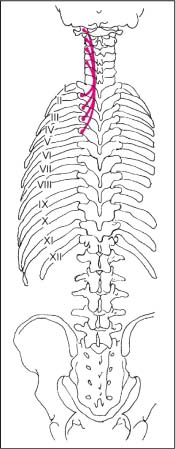
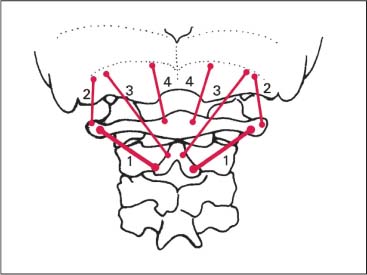
SRS Correlation
The spondylogenic unit, the myotenone, is represented in Fig. 17.72. The 17 myotenones of the semispinalis muscle are correlated with the spinal segments C0 through T9.
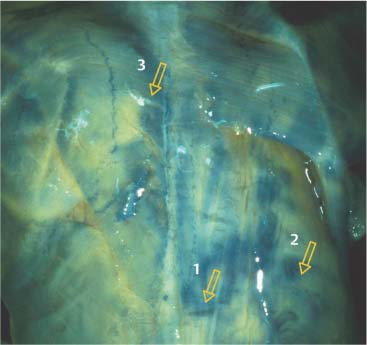
Fig. 17.71 Muscle attachments at the transverse process of the thoracic vertebra.
1 Short rotator
2 Long rotator
3 Multifidus
4 Semispinalis thoracis
5 Longissimus capitis and cervicis
6 Semispinalis capitis
7 Longissimus thoracicis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree