INTRODUCTION
The study of functional anatomy—human anatomy as it relates to function—is an undertaking vital to physiatrists and any medical professionals who care for patients with disabilities or injuries of the musculoskeletal system. This chapter provides an overview of functional anatomy organized by common clinical problems framed from the perspective of anatomic study. There are many excellent resources for further study, which is essential for mastery of this topic. Some of these are listed within this chapter.
THE UPPER LIMB
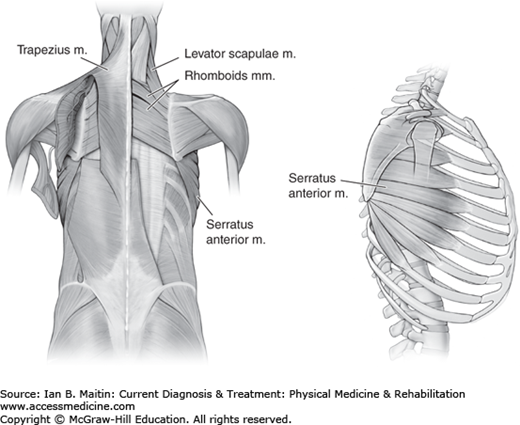
The trapezius muscle (Figure 2–1) performs the following functions:(Figure 2–1)
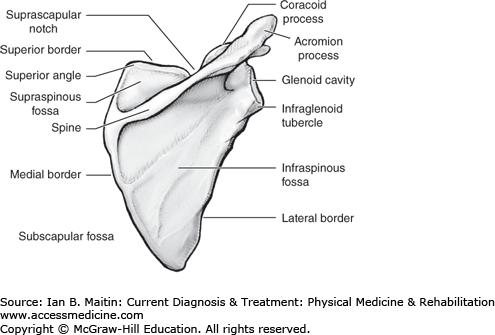
It stabilizes the scapula (Figure 2–2) proximally in the coronal plane via retraction toward the rib cage and spinous processes.
It rotates the scapula upward in the coronal plane to maximize upward and outward reach of the arm.
It rotates the scapula to optimize the length–tension relationship for the other shoulder abductor muscles, including the deltoids and the rotator cuff, allowing for the most efficient and forceful contraction.
The serratus anterior muscle (Figure 2–1) stabilizes the scapula in the sagittal plane, rotates the scapula upward in the sagittal plane, and protracts the scapula. This produces a combination of lateral excursion in the coronal plane, internal rotation, and anterior translation in the sagittal plane. Weakness of the serratus produces scapular dyskinesis in the sagittal plane, most notably during flexion of the arm.
The arm can be abducted 180 degrees in the coronal plane. Of this motion, 120 degrees occurs at the glenohumeral joint and 60 degrees occurs at the scapulothoracic joint. Weakness of the trapezius causes impairment in arm abduction and produces a form of scapular dyskinesis. Scapular dyskinesis, or alteration in the normal scapulohumeral rhythm, results in a counter-rotation of the scapula downward, due to the direction of deltoid pull and the unopposed force of gravity on the upper limb. Humeral abduction in the coronal plane can be limited to as little as 60 degrees of abduction due to the limitation of scapulothoracic joint motion. Shoulder abduction in the upright position causes the scapula to wing laterally in a patient with trapezius weakness.
A patient with serratus weakness may not have noticeable winging when standing upright with the arms at the sides. However, when posterior force is exerted through the humerus onto the scapula, medial winging of the entire vertebral border of the scapula is noted. (This is a more effective way to assess for winging than having the patient place the arms on a wall or having him or her perform a pushup. Patients with serratus weakness may have difficulty performing these maneuvers correctly because of concomitant weakness of other necessary musculature.)
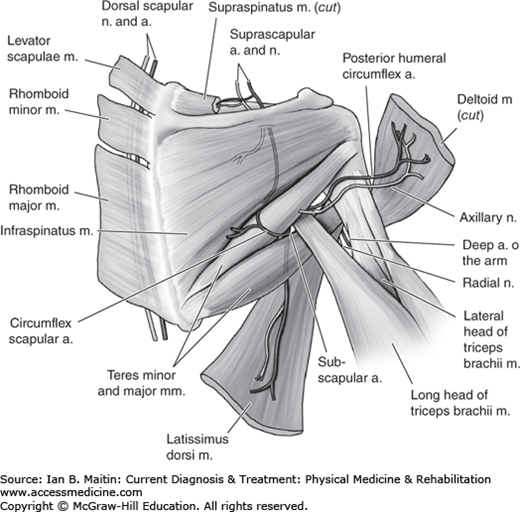
The rotator cuff is composed of the supraspinatus, infraspinatus, teres minor, and subscapularis muscles (Figure 2–3). The first three muscles originate from the posterior scapula (Figure 2–2) and insert on the greater tuberosity of the humerus, functioning to externally rotate the humerus. The subscapularis originates on the anterior fossa of the scapula and inserts on the lesser tuberosity of the humerus.
Collectively, the rotator cuff muscles confer dynamic stability to the glenohumeral joint by holding the humeral head centered within the glenoid fossa. The rotator cuff musculature resists humeral translation and subluxation during the midranges of humeral motion in the coronal or transverse planes. The subscapularis is the only internal rotator of the humerus that also functions to hold the humeral head in the glenoid dynamically during internal rotation. Thus weakness of the subscapularis may have a more profound impact on strength of internal rotation than weakness in the anterior deltoid or pectoralis muscles. Weakness of the whole rotator cuff produces limited overhead motion as the middle deltoid contraction vector causes anterior–superior subluxation of the humeral head and clearly impairs further glenohumeral joint motion. The rotator cuff muscles function as dynamic stabilizers of the glenohumeral joint by pulling the humeral head into the glenoid fossa throughout flexion, extension, abduction, and adduction of the arm.
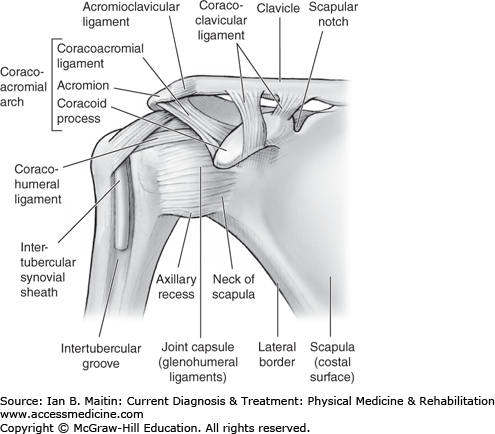
One of the major joints of the shoulder, the acromioclavicular joint (Figure 2–4) is supported by the acromioclavicular ligament and the coracoacromial ligament. The superior aspect of the acromioclavicular ligament runs horizontally over the joint and provides stability in this direction. The coracoacromial ligament extends to the acromion from a wide base on the coracoid process. The coracoclavicular ligament, while not technically a part of the acromioclavicular joint, is composed of two parts, the trapezoid and conoid ligaments, and attaches the scapula to the clavicle.
Injury to the shoulder, such as forcibly landing on the shoulder, can produce damage to the acromioclavicular joint and is termed a shoulder separation. Such an injury impairs scapular motion and thus flexion and abduction of the arm. The degree of damage to the acromioclavicular and coracoclavicular ligaments and degree of resulting displacement of the clavicle relative to the acromion are the criteria for the classification of acromioclavicular separations. Type I injuries involve sprained but intact coracoclavicular and acromioclavicular ligaments. Type II injuries are characterized by a complete disruption of the acromioclavicular ligament with a sprained but intact coracoclavicular ligament. In a type III injury, both the coracoclavicular and acromioclavicular ligaments are completely disrupted. Type IV injuries are characterized by posterior displacement of the clavicle relative to the acromion with buttonholing through the trapezius muscle. In type V injuries, the clavicle is widely displaced superiorly relative to the acromion as a result of disruption of muscle attachments. Type VI injuries are rare and are characterized by displacement of the distal clavicle below the acromion or coracoid process.
Static stabilizers of the glenohumeral joint include the following structures (Figure 2–4):
Glenohumeral joint capsule
Superior glenohumeral ligament
Middle glenohumeral ligament
Inferior glenohumeral ligament
Coracohumeral ligament
Coracoacromial ligament
With removal of the glenohumeral joint capsule the force required to dislocate the glenohumeral joint is decreased by 20%, indicating that this structure has an important role as a static stabilizer. The superior glenohumeral ligament provides posterior and inferior stability when the humerus is in adduction and external rotation. The middle glenohumeral ligament restrains anterior glenohumeral joint instability when the humerus is in 45 degrees of abduction. The inferior glenohumeral ligament protects from anterior and posterior glenohumeral joint instability. Severing the posterior band of this ligament results in posterior subluxation; however, dislocation will not occur until the rotator interval is disrupted.
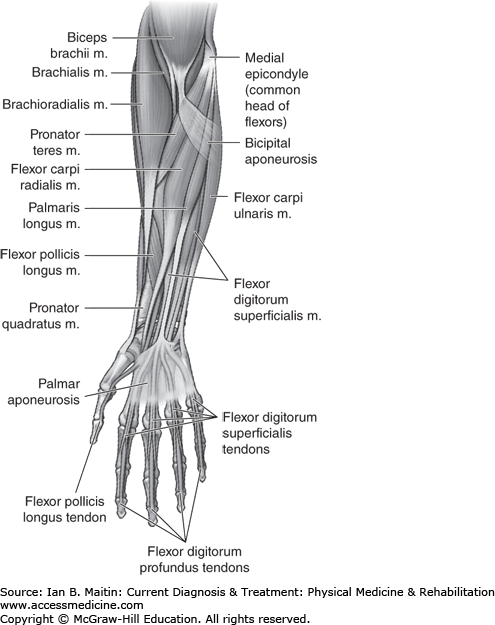
The flexor digitorum superficialis and the flexor digitorum profundus are anterior forearm muscles (Figure 2–5) that flex the fingers at the proximal interphalangeal joint and the distal interphalangeal joint, respectively. The deep anterior forearm muscle, the pronator quadratus, runs from the distal ulna to the radius with fibers running perpendicular to these bones. The flexor pollicis longus, also of the deep compartment of the anterior forearm, inserts onto the distal phalanx of the thumb and is the only muscle that flexes the interphalangeal joint. All of the aforementioned forearm muscles are innervated by the anterior interosseous branch of the median nerve with the exception of the flexor digitorum superficialis, which is innervated by the median nerve proper, and the medial half of the flexor digitorum profundus, innervated by the ulnar nerve.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree