Fig. 8.1
Free flap from the flexor aspect of the wrist. SBPRA superficial palmar branch of the radial artery, PCBMN palmar cutaneous branch of the median nerve, SCV subcutaneous vein
Arterialized Venous Flaps
Venous flaps are those in which the primary blood supply enters and exits the flap through the venous system. The exact vascular circuit or mechanism of physiologic nutrition, however, remains unclear [23].
There are several clinical applications for them in the reconstruction of hands and fingers when conventional flaps are limited or unavailable [24]. They can be used as pedicled venous flaps, free venous perfusion flaps, free arterial perfusion (arterialized) venous flap, and innervated AVF for different goals such as resurfacing soft tissue defects, skin and vascular defects, reconstruction of circumferential injuries, and, of course, for fingertip reconstruction .
Several classifications of the venous flaps have been described in literature based on: vessels that enter and leave the flap as well as the direction of flow within these vessels [25], presence of an intravenous valve, the venous network of the donor site, the location, and the number of veins at the recipient site [26]. Probably the most commonly used venous flaps in plastic and microsurgery surgery are the three classification types of Thatte et al. [25] which are type I, unipedicled venous; type II, bipedicled; and type III, AVFs, which are perfused by a proximal artery anastomosed with a cephalad end vein and drained by a distal vein. The most reliable of these is the type III [27] and that is why clinical use has mostly focused on it.
Success in reconstructing skin defects of the digits with AVFs seems to be influenced by the donor site and size of the flap [27]. The influence of donor site on the survival of AVFs has been attributed to the configuration of the venous network of different donor sites. The most frequent donor sites for venous flaps are: the distal volar forearm, the dorsum of the foot and medial aspect of lower leg, and the thenar and hypothenar eminences [28]. The configuration of the dorsal skin of digits and hypothenar or thenar eminence is more favorable than that of the volar forearm, while the donor site of the lower leg, in which there is a poor venous network, is considered the last choice for venous flaps. Kakinoki et al. [29] showed that the size of the flap was the factor that correlated statistically with a successful result. AVFs with a surface area less than 767 mm2 were less likely to develop necrosis of the skin (Fig. 8.2).
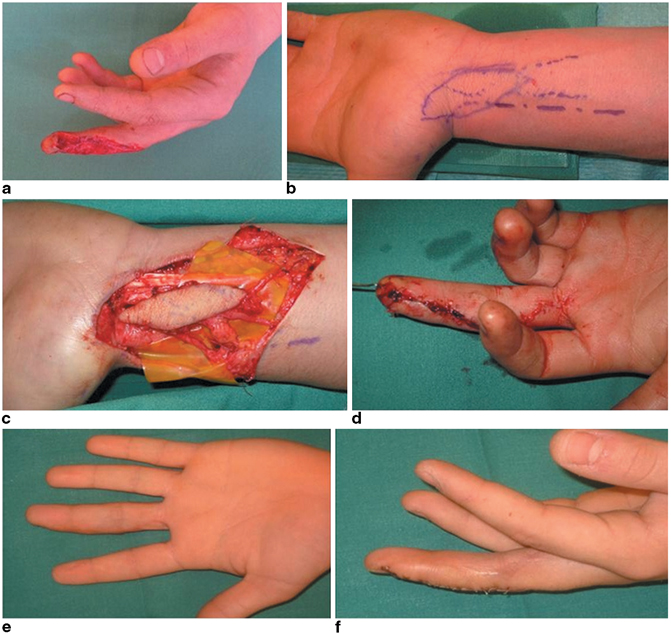
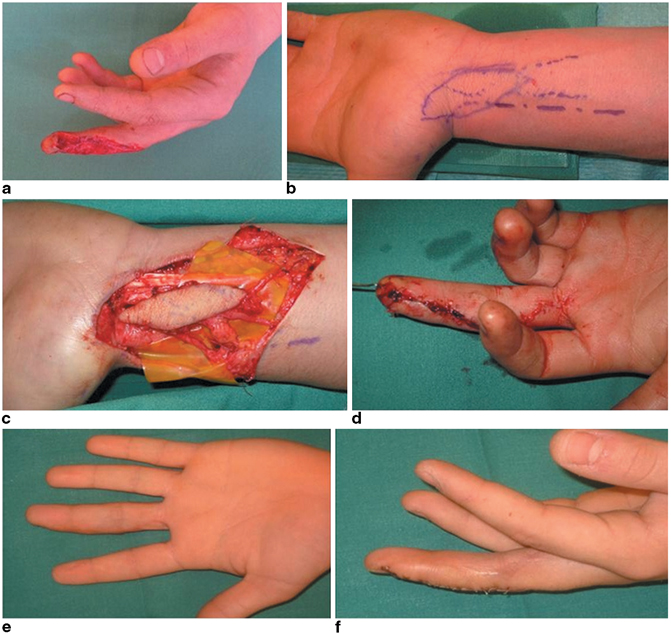
Fig. 8.2
Arterialized venous flap from the distal volar forearm. The terminal branch of the lateral cutaneous nerve of the forearm is included in order to provide a sensate flap. (Courtesy: Dr. Thomas Giesen)
For fingertip reconstruction, the most indicated AVFs are the thenar and hypothenar flaps, first described by Iwasawa et al. [28], since the volar forearm and dorsum of the foot skin are not glabrous skin, have poor skin texture for volar surface reconstruction, and result in instability with pinching.
The operative technique of the AVF from thenar and hypothenar eminences was described this way in the original paper:
The donor site is the lateral side of the metacarpophalangeal joint for the thenar venous flap and the lateral side of the hypothenar region for the hypothenar flap. A branch of the dorsal cutaneous vein is located in either the thenar or the hypothenar region. When elevating the flap, a segment of the branch of the dorsal cutaneous vein, the subcutaneous tissue and deep fascia of the thenar or hypothenar muscles are included. At the recipient site, a proper digital artery and dorsal vein are prepared at the interphalangeal joint level and microvascular anastomoses are performed between these vessels [28].
The skin of the thenar and hypothenar regions is not completely glabrous. However, it has a thick keratosis layer and deep fascia of the thenar and hypothenar muscles that provide durability for mechanical stress and good stability. None of these is a sensory flap. Nevertheless, good sensory recovery has been reported with thenar and hypothenar flaps by Iwasawa et al. The authors explained this recovery is due to the fact that palmar tissue has many sensory receptors [28].
Innervated AVFs have been described from the dorsum of the foot preserving sensation by anastomosing branches of superficial peroneal nerves with the digital nerves [30] but they are nonglabrous flaps. The authors explain that, “ideally, the volar side of the finger should be reconstructed with glabrous skin such as palm or instep. Although small arterialized venous flaps that use medial plantar skin are useful for finger pulp reconstruction it is difficult to harvest a thin and pliable arterialized venous flap from medial plantar skin. It is also not easy to include enough long cutaneous veins and cutaneous branches of medial plantar nerve in the instep venous flap.”[31]
Compared with conventional arterial flaps, the advantages of venous flaps are that they provide non-bulky and good-quality tissue, ease of design, and harvest without the need to perform deep and tedious dissection, no sacrifice of a major artery at the donor site, no limitation of the donor sites, and less donor-site morbidity with optimal postoperative contour. They could be a good option for reconstruction of small defects of the fingers, but it should be noted they are either insensate or nonglabrous skin flaps or both. Also, they have an unstable postoperative course and are difficult to monitor. They are not very reliable due to their inconsistent survival and possible partial loss, but these problems may be solved by techniques such as surgical delay procedure, pre-arterialization technique, surgical expansion, and application of growth factors after meticulous preoperative planning. [23].
Posterior Auricular Artery Sensate Flap
This flap provides wound coverage while retaining sensation and negligible donor-site morbidity. It is used for fingertip radial-side pulp reconstruction and is based on the posterior auricular artery . The first clinical success for the free retroauricular skin flap was reported by Wada and coworkers in 1979 [32], and it has been popular for intraoral and facial reconstruction for years. It was in 2009 when Hsieh et al. [33] first described this flap for fingertip reconstruction .
The posterior auricular sensate free flap is not simple but some authors consider it cost-effective because the sensation recovery is good and primary closure of the donor site is possible. The donor-site scar is located in the posterior auricular area, and it provides good aesthetic appearance of finger reconstruction area with no joint stiffness.
Surgical Technique
The posterior auricular vessels over the posterior auricular sulcus must be detected preoperatively using a Doppler probe. The posterior auricular vessel is identified after incision over the posterior auricular sulcus and meticulous dissection. A skin island in the posterior auricular area is designed over the entry area of the posterior auricular vessel. The flap is elevated from the layer beneath the posterior auricular vessel. The great auricular nerve is also identified in the posterior auricular area. The pedicle of the posterior auricular flap is anastomosed to the radial digital artery and dorsal vein, and the great auricular nerve is anastomosed to the radial side digital nerve . Primary closure of the posterior auricular donor site can be accomplished with no morbidity [33] (Fig. 8.3).
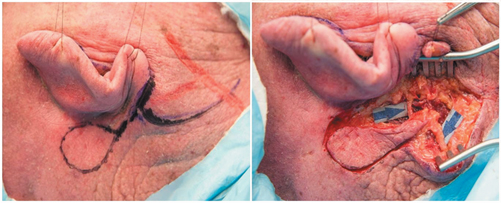
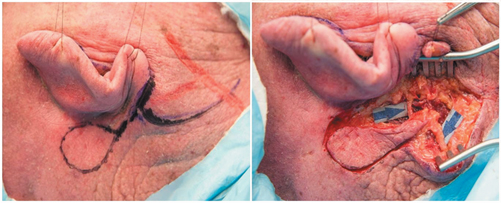
Fig. 8.3
Posterior auricular artery sensate flap. Cadaver dissection. Arrows show the vascular pedicle and the great auricular nerve. (Courtesy: Dr. Shih-heng Chen)
Widespread utilization of the posterior auricular free flap has yet to become popular due to a considerable amount of technical challenges, although previous success has been reported and can be promising. Technical challenges include a short vascular pedicle, a superficial venous system that is not always present, extremely small vena comitantes, anatomic variation [34] (for instance, sometimes posterior auricular vessels are too small to transfer in a free flap), tendency of the flap based on the superficial temporal vessels to become congested, and limited flap size (although this is not usually a problem when treating pulp injuries).
Since there are few reports of this flap as far as pulp coverage is concerned in the literature, it is difficult to draw reliable conclusions about its indications and true functional and aesthetic results. Hsieh et al. [33] report 7 mm of static 2PD and good aesthetic recovery and consider this flap an alternative to foot tissue transfers.
Inversely, there are other flaps such as the posterior interosseous artery flap [35] or the temporoparietal free fascial flap with a split-thickness skin graft [36] that are mentioned in the literature as useful for fingertip coverage. The former gives excellent cover but it is a nonglabrous skin flap, and the latter, even though it provides a pseudo-glabrous surface, is relatively insensate. These reasons are more than enough not to consider them ideal options for the replacement of pulp injuries.
Glabrous Skin Flaps
Defects on the volar surface of the fingers require replacement with specialized sensory cells that can only be found in the hand itself, on the toes, or on the sole area of the foot, what is generally known as glabrous tissue [37]. The best way to accomplish this replacement is by microneurovascular transplantation of glabrous skin from the foot [38].
The most widespread free flaps that can provide glabrous skin on a consistent vascular pedicle are the free medialis pedis flap, free MPAP flap, and great toe and second toe pulp neurovascular island (NVI) flaps.Free medialis pedis flap and free MPAP flap are interconnected and share anatomy and some properties. The complex vascular anatomy of the medial plantar system was reported in 1990 by Masquelet and Romana [39]. The medial plantar artery is divided into the superficial and deep branches of the medial plantar artery . The deep branch of the medial plantar artery in turn subdivides into lateral and medial branches. The medial branch runs dorsally between the tibialis posterior tendon and the abductor hallucis muscle, after which it courses distally along the medial margin of the foot, proximal to the tubercle of the navicular bone. The artery is usually accompanied by one or two venae comitantes.
The medialis pedis flap receives its blood supply from the medial branch of deep division of the medial plantar artery. In contrast with this, the MPAP flap is nourished by superficial division of the medial plantar artery [40] (Fig. 8.4).
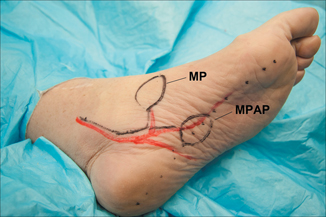
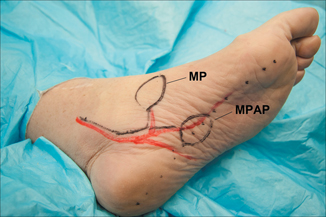
Fig. 8.4
Free medialis pedis (MP) flap and free medial plantar artery perforator (MPAP) flap schematic design. The red line indicates the posterior tibial artery trajectory with the medial plantar artery branch for MP flap and superficial division of the medial plantar artery branch for MPAP flap. Cadaver dissection
The free medials pedis flap for resurfacing skin defects of the hand and digits was first reported by Ishikura et al. [22] based on Masquelet and Romana’s studies [39] for soft tissue defects of the foot in which a thin and supple skin cover was needed. The advantages of this flap are: It is very thin in comparison with other standard free flaps; it can be used for small repairs; it possesses two draining venous pathways, the vena comitantes and the subcutaneous veins; the diameters of its vessels are similar to those of the fingers; it provides a good color and texture match for the repair; and according to Ishikura, a good recovery of protective sensation is achievable.
This latter point is questionable since one of its main disadvantages is that it is an insensate flap. Other drawbacks are that skin grafting is usually necessary for donor-site closure and that in cases where the posterior tibial artery represents the dominant or singular inflow source to the foot, the harvesting of this flap could potentially compromise the circulation to the foot. Although it can be an appropriate flap for volar hand and digit injuries given that it provides glabrous skin coverage, its use is discouraged for fingertip lesions since it is not a sensory flap (Fig. 8.5).
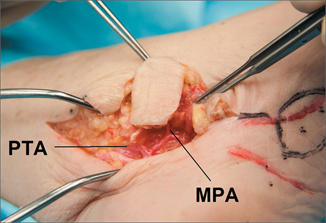
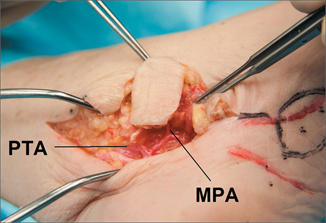
Fig. 8.5
Free medialis pedis flap. Cadaver dissection. PTA posterior tibial artery, MPA medialis pedis artery
The free medial plantar artery perforator flap, despite its anatomical proximity to the medialis pedis flap, has several positive differences: It is thicker, providing adequate cushioning surface; donor site can close primarily if flap width is less than 2 cm, and it can be sensate including the cutaneous branch of medial plantar nerve or saphenous nerve for anastomosing to the digital nerve [41].
Before 1986, when Hidalgo described favorable results using it for palm coverage [42], its utilization was limited for resurfacing feet and heel defects since Mir and Mir presented it in 1954 [43]. However, the first report of this flap as a neurovascular flap for pulp reconstruction was published by Inoue 2 years later [44] (Fig. 8.6).
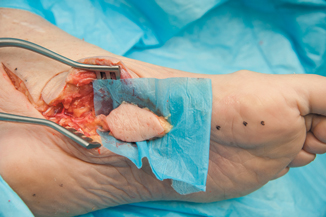
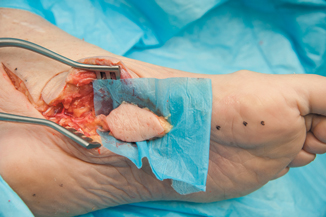
Fig. 8.6
Free medial plantar artery perforator flap. Cadaver dissection
Operative Technique
The posterior tibial artery can be located by palpation posterior to the medial malleolus and followed downward to the instep groove between the abductor hallucis muscle and the flexor digitorum brevis muscle. The perforator can be easily identified by marking the septum between the abductor hallucis and the flexor digitorum brevis with a straight line. From this line, a perpendicular line is drawn to the navicular tubercle and the perforator will be located in a 2-cm-radius area from this line [40] and adjacent to the first cuneiform bone. This can be confirmed by Doppler.
The medial plantar flap is designed on the axis of the plantar surface of the first metatarsal with the perforator in the central area [38]. The plantar incision is made and the suprafascial plane is dissected until the perforators are identified. To expose the medial plantar vessels, a dissection between the abductor hallucis muscle and the flexor digitorum muscle is performed. Then, the lateral incision is made and the vein draining into the saphenous system is preserved, in case the comitantes veins of medial plantar artery are too small for anastomosis. The saphenous vein branch is also isolated with the saphenous nerve to innervate the flap. After releasing the tourniquet, flap circulation is evaluated and if there is no problem, the flap is harvested and inset on the finger . Inflow is provided by a digital artery and outflow is established via dorsal vein. The digital nerves are repaired to the saphenous nerve branch.
The advantages of this flap were well detailed by Huang et al. [40]: (a) It can be up to 7 cm long and 2 cm wide, providing a large surface area; (b) medial plantar vessels remain intact, therefore there is no compromise of the foot’s blood supply; (c) provide cushioning and glabrous skin, (d) flap elevation can be performed quickly in experienced hands because a short pedicle does not require a tedious dissection; and (e) size and length of pedicle are compatible with the digital vessel.
It also presents disadvantages: Preserving small perforators without causing further injury is difficult and delicate surgical skills and sometimes microscope-assisted procedures are needed. When the donor area is more than 2 cm wide, it is necessary to use split-thickness skin graft to close. And mainly, there is some lack of good 2PD recovery although it is a sensate flap [45]
Great Toe Pulp Neurovascular Island Flap
Of all the free flaps utilized for digital pulp reconstruction, the free neurovascular toe flap provides a particularly efficient solution for loss of cutaneous substance [46, 47]. It not only restores the finger with a solid and well-cushioned cover but also with a dense population of specific sensory end organs attached to the flap [45]. That is the main advantage of these flaps in comparison with any other flaps, as they comply with one of the major surgical principles described by Sir Harold Gillies, the father of modern plastic surgery: “replace like to like” [48].
With the free neurovascular toe flap we not only provide tissue with the same unique mechanical and aesthetic characteristics of the finger and thumb pulp but also provide their same specific sensory functional pattern. From the mechanical and aesthetic point of view, the palmar aspect of the hand is gifted with anatomical characteristics of skin, subcutaneous tissue and appendages, suitable for carrying out its principal functions of pinching and grasping [49]. It is devoid of hair and the epithelium is of thick cornified stratified squamous epithelium, rich in ridges and grooves that become thicker with usage [50]. Also, the epidermis is thick compared with that on other body areas and has abundant sweat glands but not sebaceous glands [49]. The connective tissue forms a dense array of tissue with numerous fibrous septa interconnecting the volar digital skin, periosteum, and synovial sheaths, and the connective tissue of dermis is more compact and less elastic. The subcutaneous tissue exists in many compartments in between these fibrous septa, adding a cushion effect and durability to an area constantly exposed to friction forces [41]. The pulp of the toes is the unique area of the body that has the same characteristics, so there can be no better option for replacement in case of this tissue loss.
As far as the sensory function is concerned, it is known that sensory endings can be divided into three general patterns: free sensory endings, sensory endings with expanded tips, and encapsulated sensory endings. Free nerve endings are encapsulated and are responsible for pain and temperature sensation. Sensory endings with expanded tips are the so-called Merkel’s cell and the Ruffini complexes. Merkel’s cell neurite complexes are only present in glabrous skin and are responsible for transmitting sensation of constant touch, pressure, and static tactile gnosis whereas Ruffini complexes are only present in hairy skin. The encapsulated sensory endings are found exclusively in glabrous skin. They are the Pacinian corpuscles and Meissner’s corpuscles, highly sensitive converters of mechanical stimuli. Also, Meissner’s corpuscles seem to provide the ultimate degree of sensitivity for tactile gnosis and discrimination. Both corpuscles are fast-adapting fiber mechanoreceptors that mediate sensory relays concerning moving touch, fluttering, vibration, and moving tactile gnosis [37, 38].
It is logical to assume that replacing specifically these specialized sensory endings by the same kind of sensory endings, we will be able to get the best critical sensory recovery. It has been observed that there is a correlation between the return of functional sensibility and the total number of Meissner’s corpuscles in the transplanted tissue [51], which would demonstrate the necessity of using selectively glabrous skin tissue to replace glabrous skin loss if we want to achieve the best sensory result. Despite these apparent logical advantages, the application of this flap has been typecast only for selective cases and patients.
Classically, it has been differentiated between manual laborers in whom fast functional recovery is the main purpose; thus, easy, quick recovery and reliable procedures are recommended (simple revision amputation, skin grafting, island flap, etc.) and sensitivity-demanding professions such as musicians, in whom sensitivity recovery is the priority and who need specific solutions to reach that goal.
The toe pulp NVI flap is typecast in literature as the ideal and almost exclusive indication for those latter patients. However, in our opinion its indications should be expanded for any patient when preserving functional and aesthetic appearance of the injured digit is the priority and the size of the defect contraindicates the use of local flaps.
History
Reconstruction of pulp defects with toe pulp NVI flap was described for the first time in 1978 by Buncke and Rose [46]. In their paper, they propose a new technique that offered durable skin cover which becomes innervated by the sensory nerve of the recipient finger itself, and does not result in deformity or anesthesia of an adjacent finger nor require cortical reorientation of stimuli, unlike Littler’s technique [52].
Although only four out of six flaps they presented survived, they showed an innovative idea that has been applied by surgeons for pulp reconstruction all over the world. Precisely, this low flap survival rate at the beginning questioned this technique’s reliability, and literary tradition has retained this idea for the last century without taking into account more recent results that show flap survival rates up to 99.7 % in the largest series [53]. In fact, the current average survival rate has been shown to be 98 % [54]. Undoubtedly, the development of microsurgery and technique refinement since the first reports have contributed to making this flap very reliable.
Another argument of the authors who criticize the reliability of toe to pulp NVI flap is its anatomy variability, which can complicate the dissection of the flap and the fact of sacrificing a major artery, which may adversely affect foot circulation during old age [33].
It is true that neurovascular anatomy of the foot is quite complicated and a significant amount of variations have been described. The first dorsal metatarsal artery (FDMA) originates from the dorsalis pedis artery when the latter dives plantarward at the base of the first intermetatarsal space. As described by Poirier and Charpy [55], the artery courses over the dorsum of the first dorsal interosseus muscle and divides into two branches—medial and lateral—at the level of the metatarsophalangeal joint of the big toe. The medial branch provides two dorsolateral collaterals to the big toe. The lateral branch terminates as the dorsomedial branch of the second toe. Distally, in the web space, the FDMA plunges plantarward and bifurcates into its terminal branches, both medial and lateral. The medial plantar branch forms the plantar hallucal arteries, both fibular and tibial, whereas the lateral branch terminates as the medial plantar artery of the second toe. The lateral branch of the first plantar metatarsal artery (FPMA) joins the FDMA at the level of its plantar bifurcation. The plantar tibial hallucal artery crosses transversely between the mid-segment of the proximal phalanx and the flexor hallucis longus tendon to reach the medial plantar aspect of the big toe, where it is joined by the medial bifurcation branch of the FPMA. Poirier and Charpy clearly state that it is the FDMA and not the FPMA that provides the three inner plantar collaterals of the first and second toes. The FPMA is considered a branch of the dorsalis pedis or a terminal branch of the lateral plantar artery. It arises at the level of the inferior border of the second metatarsal from the dorsalis pedis arterial area during its vertical course in the first intermetatarsal space. It is directed medially and anteriorly, separated from the FDMA by the first dorsal interosseous muscle. It is located deep to the level of the oblique head of the adductor hallucis and the flexor hallucis brevis. Initially applied against the lateral surface of the first metatarsal, the artery passes between the bone and the flexor hallucis brevis muscle. At the level of the distal bifurcation triangle of this muscle, the FPMA divides into two branches: lateral and medial. The lateral branch courses between the two heads of the flexor hallucis brevis and then passes plantar to the lateral head of the short flexor. It turns around the lateral sesamoid, pierces the deep lateral sagittal septum of the plantar aponeurosis for the big toe, courses on the plantar aspect of the deep transverse metatarsal ligament, and joins the FDMA at the point of bifurcation in the first web space. The medial branch of the FPMA also emerges between the two heads of the short flexors of the big toe, passes around the medial sesamoid or between the two sesamoids, and terminates in the tibial plantar hallucal artery. This medial branch is joined by a thin branch from the medial plantar artery [56].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








