I. FRACTURES OF THE PROXIMAL HUMERUS
A. Mechanism. Proximal humerus fractures are seen in all age groups, but are more common in the elderly. In young adults, they are a result of high-energy trauma. In older patients, they often result from low-energy falls.1
B. Physical examination. Bruising and swelling about the shoulder and pain and crepitus with passive motion of the glenohumeral joint suggest a proximal humerus fracture. A careful neurologic examination is essential, as proximal humerus fractures and fracture–dislocations can be accompanied by axillary nerve and brachial plexus injuries.
C. Radiographs. Evaluation should include anteroposterior, true anteroposterior, and axillary lateral shoulder radiographs, as well as anteroposterior and lateral films of the humerus. Pain may limit motion, making obtaining an axillary lateral difficult. Assisting the patient by slowly and gently elevating the arm while they lie in a supine position can achieve sufficient elevation for axillary radiographs. Alternatively, a Velpeau view, obtained with the patient’s arm resting at their side and their forearm across their chest can also demonstrate fracture alignment.
D. Treatment. Neer divides proximal humeral fractures into six groups, as shown in Fig. 18-1, on the basis of the number of fracture fragments and the degree of displacement.In order to be considered a displaced fragment, the fragment must be displaced more than 1 cm or angulated more than 45° (thus a nondisplaced fracture is a Neer one-part fracture, no matter the number of fracture lines). Although studies have shown a lack of inter-rater reliability in interpreting radiographs to accurately classify proximal humerus fractures,4 the Neer classification remains the most often utilized.
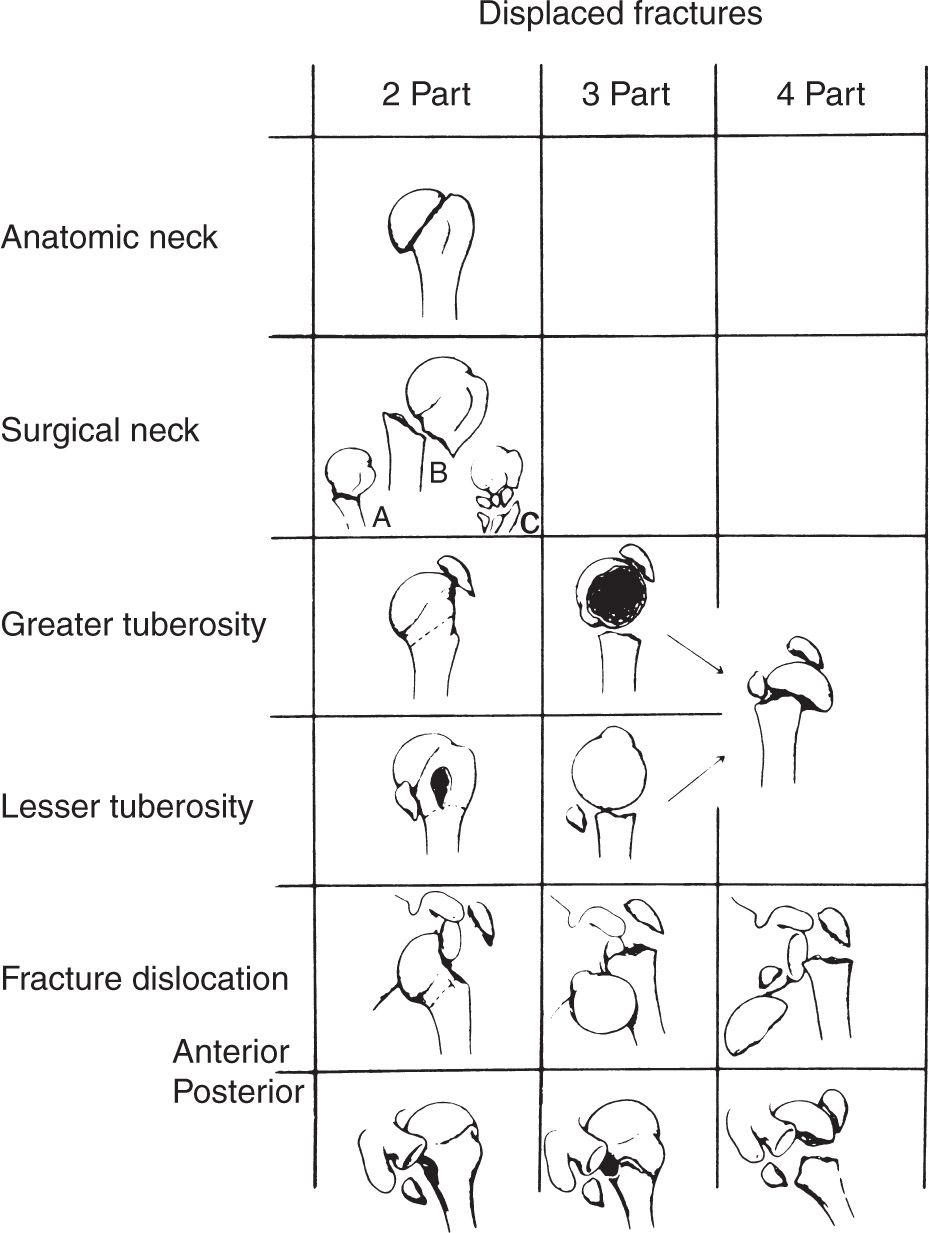
Figure 18-1. Neer’s anatomic concept for standardizing the terminology of fractures of the proximal humerus. (From Neer CS II. Displaced proximal humeral fractures. Part I. Classification and evaluation. J Bone Joint Surg Am. 1970;52:1077–1089, with permission.)
- Fractures with minimal displacement and displaced anatomic neck fractures (Neer one-part fractures). Approximately 85% of all fractures of the proximal humerus fall into this category. These fractures are typically managed nonoperatively with a sling and early motion. Stability is usually afforded by some impaction at the fracture site and the preservation of soft-tissue attachments. Elbow, wrist, and hand range of motion exercises should begin immediately. Shoulder circumduction exercises (aka pendulum exercises) are initiated as soon as they can be tolerated, generally within 5 to 7 days. The patient is instructed to bend to 90° at the waist, allowing the arm to either hang or swing in a gentle circle and avoid active contraction of the shoulder muscles.2 Assisted forward elevation and assisted external rotation exercises in the supine position can generally be started approximately 10 to 14 days after injury. Some form of protection may be needed for 6 to 8 weeks; then more vigorous physical therapy may be prescribed, including wall climbing, overhead rope-and-pulley, passive range of motion, and rotator cuff strengthening exercises.3
- Displaced surgical neck fractures. The fracture generally occurs with the arm in abduction. The rotator cuff is usually intact. Undisplaced linear fractures that extend into the humeral head can occur. The fracture site is often angulated more than 45° or malrotated. Neurovascular injury can occur in this type of fracture because the shaft may be displaced into the axilla. This is more common in elderly patients with atherosclerotic (less compliant) arteries.
a. Treatment is by closed reduction under general or supraclavicular regional anesthesia. Align the distal fragment to the proximal one, usually by abducting and flexing the distal fragment. Reduction of the fracture depends on an intact posteromedial periosteal sleeve in younger patients. The fracture may be stable enough to permit immobilization of the arm at the side in a sling-and-swathe, but may require a spica cast or abduction pillow splint to hold the arm in the reduced position. As soon as the immobilization is concluded, generally in 2 to 3 weeks, a program to regain shoulder motion is started as for fractures with minimal displacement and anatomic neck fractures.
Unstable reductions may necessitate percutaneous pin or screw fixation. In unreliable patients, the fixation may need to be protected with a shoulder spica cast for 3 weeks. With reliable patients, gentle circumduction exercises can be started immediately after pinning, and the exercise program can be advanced as described at 4 to 6 weeks after surgery for pin removal.
b. If closed reduction is impossible, consideration is given to open reduction and plate fixation or tension band wiring. A low-profile plate such as the AO/ASIF (Association for the Study of Internal Fixation) cloverleaf small fragment plate or proximal humeral locking plate is preferred. The locking plates are particularly useful in patients with osteopenia.
3. Displaced greater or lesser tuberosity fracture, or both. Rarely, a three-part fracture is encountered involving the lesser or greater tuberosity as well as the surgical neck. If the fracture is displaced, the rotator cuff function is compromised and open reduction of the fracture is indicated. The fracture should be anatomically reduced and held firmly with tension band wiring or screw fixation. It is also possible to fix these fractures percutaneously, but this will not address a rotator cuff tear. The rotator cuff tear can be addressed later if pain and weakness remain after the rehabilitation program is implemented.
3. A fracture–dislocation of the shoulder, whether anterior or posterior, may be reduced by a closed method under general anesthesia. If closed reduction fails, open reduction with internal fixation or prosthetic replacement (in older patients) is indicated.
4. Neer (see Selected Historical Readings) states that open reduction is indicated for any displaced three-part fracture and that prosthetic replacement is preferable treatment for any displaced four-part fracture. This is due to the high rate of posttraumatic humeral head osteonecrosis in four-part fractures. We believe that, at best, these are difficult fractures to treat and that operative treatment should be undertaken only by surgeons with special expertise in managing shoulder trauma.
E. Complications.
- The most common complication is loss of some glenohumeral motion, especially internal rotation and abduction. This often occurs as a result of malposition of the greater tuberosity. The best way to rehabilitate the glenohumeral joint is to start motion early and to achieve primary fracture union. Careful attention to starting an early physical therapy program can markedly improve the end result. Home programs where exercises are performed by a motivated patient two to three times per day with weekly physical therapy monitoring seem to produce the best results. Open treatment may be indicated to achieve adequate stability of displaced fractures to allow early motion.
- Delayed union or nonunion is not uncommon with displaced fractures, especially surgical neck fractures. When it occurs, some loss of joint motion generally results, regardless of subsequent treatment. If the patient experiences pain and loss of motion in association with the nonunion, the treatment is either replacement arthroplasty or internal fixation with bone grafting.
- Associated nerve and vascular damage is not rare with displaced fractures and should be identified early so that prompt, effective treatment can be instituted. Involvement of the axillary, median, radial, and ulnar nerves is reported with nearly equal frequency.
- Osteonecrosis. Avascular necrosis of the humeral head is more likely to occur after three- or four-part fractures or fracture–dislocations, but can follow even innocuous appearing fractures. If symptomatic, osteonecrosis is often managed with shoulder arthroplasty in older patients.
II. PROXIMAL HUMERAL EPIPHYSEAL SEPARATION
A. Anatomy. The proximal humeral remains open until 14 to 18 years of age, and accounts for about 80% of the length of the humerus. In younger children, significant angulation at the fracture site is well tolerated because of the remodeling potential of the growing proximal humerus.
B. Radiographs. Anteroposterior and axillary lateral radiographs typically illustrate the fracture. The most common pattern is a Salter–Harris type 2 injury, but numerous variations have been reported (see Chapter 2 for description of the Salter–Harris classification). Salter–Harris type 1 injuries are seen in neonates and in very young children.
C. Treatment. This fracture can often be reduced by closed methods with appropriate anesthesia. Reduction requires aligning the distal fragment to the proximal one, usually by abduction and external rotation of the distal fragment. As long as the rotation of the two fragments relative to one another is correct, up to 70° of angulation can remodel to produce normal shoulder function up to 7 years of age. Up to 11 years in a girl and 12 years in a boy, 50% apposition is acceptable, but varus malalignment should not exceed 45° and rotary deformity must be minimal.5,6 Treatment is then carried out in a sling with circumduction exercises. Open reduction is rarely indicated, but closed manipulation and percutaneous pin fixation should be considered if closed reduction fails to achieve an acceptable degree of correction and stability. The mature adolescent should be treated as an adult.
III. DIAPHYSEAL HUMERUS FRACTURES
A. Mechanism. Diaphyseal humerus fractures can be the result of high-energy trauma in young patients, or much lower energy mechanisms in the elderly. The incidence of this fracture is bimodal occurring at the highest rates in young adults and individuals of age 60 and older.7,8 Although the fracture may occur in any part of the diaphyseal bone, the middle third is the most commonly involved.
B. Physical examination should be thorough to rule out any nerve or vascular damage. The time of onset of any nerve involvement must be accurately documented. The radial nerve travels through the spiral groove directly on the humeral shaft and is injured in approximately 11% of diaphyseal humerus fractures.8 If the radial nerve is intact, the patient will be able to extend the wrist against gravity and extend the fingers as well as the thumb. If the radial nerve is not functioning, the patient will still be able to use the hand intrinsics to extend the fingers with the wrist in flexion. Do not be fooled.
There are three separate mechanisms by which the radial nerve may be injured.
- Damage at the time of injury usually produces a neurapraxia, less commonly an axonotmesis or traction injury, and rarely a neurotmesis. Neurotmesis is most commonly associated with open fractures.9
- During the process of manipulation and immobilization, neurapraxia can occur, and if the pressure is not relieved, it can become an axonotmesis. This is usually a result of the nerve being trapped between the fracture fragments.
3. During the process of internal fixation, neurapraxia or axonotmesis can develop from manipulation of the nerve.
C. Treatment. Initial fracture treatment includes immobilizing the arm against the chest with plaster coaptation splints, as shown in Fig. 18-2
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








