Chapter 12 Fractures of the femur and injuries about the knee

1 Classification: In the AO Classification system the femoral shaft is defined as in effect stretching between the inferior margin of the lesser trochanter (proximal segment) (1) and the upper border (2) of a square containing the distal end of the femur (the distal segment). For descriptive purposes the shaft (or diaphyseal segment) may in turn be divided into proximal (3), middle (4), and distal thirds (5). The proximal third is sometimes referred to as the subtrochanteric zone.
4. Treatment of fractures of the femoral shaft: In the adult, internal fixation by intramedullary nailing is the commonest method of treatment. The prime advantage this has to offer is that it generally permits early mobilisation of the patient, thereby lessening the risks of pulmonary, circulatory, renal, joint and other complications, while promoting muscle activity, joint movements and functional recovery. It may also alleviate problems of bed occupancy (which is the historic reason for its introduction). Note, however, that nailing may have to be delayed in favour of damage control orthopaedics. (See p. 44.)

7 I-M nailing (c): Positioning ctd: Alternatively, using an orthopaedic table, the good leg may be flexed at the hip and externally rotated, to give access for the image intensifier. Traction may be applied on the affected side in the line of the limb through a Steinman pin (1) through the tibial tuberosity (some prefer the femoral condyles), with the perineal post offering counter-traction (2). The affected side is adducted at the hip.

8 I-M nailing (d): The trochanter is exposed through a 6–8 cm lateral incision; the piriform fossa (1) is identified with a finger, and the medullary canal entered using an awl (2). The position is confirmed with the intensifier before enlarging the opening. Alternatively a guide wire (3) held in the chuck of an introducer may be used and the opening may be enlarged with a cannulated cutter (4). (An easier entry point at the tip of the trochanter may be used with angled nails – see p. 313.)

13 Retrograde I-M nailing (a): This can be of value in obese patients, in cases of multiple injury, and where there are additional fractures round the femoral or tibial condyles which have to be dealt with at the same time. The knee is flexed over a pillow to about 45°. The intercondylar notch is exposed either through a patellar tendon splitting incision or through a medial parapatellar incision, with lateral displacement of the patella.

19 Other methods of fixation: External fixators: Fractures of the femur are less easy to control with external fixators than those of the tibia, owing to the magnitude of the stresses at the fracture site from the weight of the limb. Nevertheless the technique is often useful in the management of highly contaminated open fractures, and can be replaced under suitable circumstances by an I-M nail at up to 10 days post trauma. Some cases of open fracture are suitable for treatment by thin wire methods (e.g. Ilizarov p. 79).

20 Other methods of fixation: Plating: This is useful for rapid, rigid fixation in an ischaemic limb requiring vascular repair. Plating has a slightly increased risk of infection and non-union. Compression plating (but see p. 77 for alternatives) is best carried out engaging 8 cortices above and 8 below the fracture, and if possible an interfragmentary screw should be inserted. Compression plating with bone grafting is sometimes used in the treatment of non-union after intramedullary nailing.

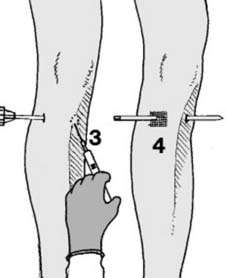
25 Applying skin traction (a): With the exercise of care and gentleness this can usually be done without an anaesthetic. (1) Begin by shaving the skin. (2) It is then traditional to swab or spray the skin with a mildly antiseptic solution of balsam of Peru in alcohol. This may facilitate the adhesion of the strapping.

31 Traction systems: Skin traction in a Thomas splint (a): The most important decision in selecting a Thomas splint is the ring size. To save time (e.g. before anaesthesia) the uninjured leg may be measured, and an allowance of 5 cm made for swelling, present and anticipated. It is nevertheless wise to have readily available a size above and below the estimate in case of inaccuracies.

37 Thomas splint (g): In long oblique fractures and those with apposition no manipulation will be needed and the traction system may be completed by, for example, tying the cords to the end of the splint (1). The convention of passing the medial cord under the corresponding iron helps to control the tendency to lateral rotation (2). A Chinese windlass (of spatulae or a metal rod) may be used to take up slack (3).

42 Thomas splint (l): The pressure of the ring of the Thomas splint tends to produce sores (1) (especially in the perineal, groin and ischial tuberosity regions) and must be relieved (3). This is done by applying traction (c. 3 kg/8 lb) to the anchored cords (2). If ring pressure is unrelieved, increase the traction weights.
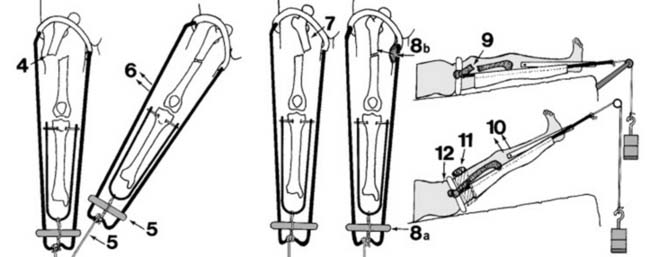
48 Thomas splint (r): Corrections: (ii) Where the proximal fragment is abducted (4) the position may be improved by increasing the traction (5) and abducting the leg (6). The position of the ring traction pulley and the splint supports will require corresponding adjustment. (iii) If the proximal fragment is adducted (7) increase of traction alone (8a) may lead to an improvement in the position. It may be helpful to apply side thrust with a pad (8b) between the leg and the medial side iron. (iv) Flexion and/or abduction of the proximal fragment (9) due to unresisted psoas and gluteal action is frequently a very painful complication. In the young patient, raising the splint (10) and/or abducting the leg and bandaging a local pad in position (11) may bring the fragments into alignment, but this manoeuvre is less certain in the older patient where internal fixation is frequently advisable for femoral fractures at this level and of this type. In any patient in whom this conservative technique is practised, care must be taken to avoid pressure in the region of the anterior superior iliac spine (12).

52 Thomas splint (v): Aftercare (iii): The ring area: Good nursing care is vital to avoid skin breakdown. In addition, for: circumferential tightness, split the ring; perineal pressure, increase the ring traction weight; anterior spine pressure (a), lower the splint (b); pressure below the ring (c), decrease or remove any support weight (d) and place a pillow above the ring (e); pad the edge of the sling if needed (f).
54. Thomas splint (x): Aftercare (v): In those cases where skeletal traction is employed, look for:
During the period a patient spends in bed he should practise quadriceps and general maintenance exercises. Splintage in children should be continued till union (6–12 weeks). In adults, mobilisation of the knee joint and/or the patient may be possible before union is complete.
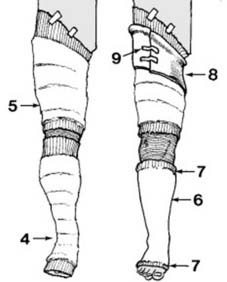
57 Cast bracing (ii): A layer of wool roll is used to protect the bony prominences below the knee (4) and as a single layer of padding in the thigh (5). A below-knee plaster is then applied (6) and completed by turning back and incorporating the circular woven bandage (7). An appropriately sized bucket top of polythene is selected (8), trimmed as required and taped in position (9).

61 Gallows traction: Children up to the age of 3 years (or 4 if very small and light) are ideally treated by this method, which may sometimes be used at home if the circumstances are suitable. Traction tapes are applied to both legs and fixed to an overhead beam (1) so that the child’s buttocks are just clear of the bed (2), making nursing easy. The body weight is responsible for the traction. Gallows traction should not be used in the older child as there is the risk of vascular spasm and peripheral gangrene.

62 Hip spica: Stable femoral shaft fractures may be supported by a plaster hip spica (3); this must include the injured leg to the toes, the other leg to above the knee, and extend to above the nipple line (‘one and a half hip spica’). A hip spica may be used for the fretful child where good nursing care is available at home (with fortnightly out-patient reviews) or for the badly infected open injury in the adult (see Ch. 11 for application details).
(f) Femoral neck fracture with dislocation of the hip: See p. 295.

65 Fractures of the femur after hip replacement (a): The Vancouver Classification of these fractures (Duncan and Masri) is well established. Three Groups, some with subdivisions, are recognised: Type A: These are the trochanteric fractures (incidence 4%), and are subdivided into AG and AL, depending on which trochanter is involved. Type B: These occur round or just distal to the stem of the prosthesis. In B1 the prosthesis is stable (incidence 16%).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree