I. GENERAL INFORMATION
A. Anatomy, epidemiology, and mechanism. The clavicle is the main stabilizer between the axial (via the sternoclavicular joint) and the appendicular (via the acromioclavicular joint) skeleton. It has a unique S-shaped curve as seen in an axial X-ray projection, but is flat in the anteroposterior plane. Any force absorbed by the upper extremity transmits to the thorax through the clavicle. This fact, in addition to its superficial location, explains why it is vulnerable to injury. It has been estimated to be one of the most commonly fractured bones, at 3.8% of all fractures.1
Classic articles2,3 on clavicle fractures indicated that nonunion after fracture occurred approximately 0.1% to 0.8% of the time; however, nonunion rates in contemporary series are higher. A systematic review of 2,144 clavicle fractures by Zlowodzki et al.4 detailed a 15.1% nonunion rate in displaced clavicle fractures. Risk factors for nonunion include advancing age, female gender, completely displaced clavicle fractures with bony no contact, distal clavicle fractures, and comminuted fractures.5 These variables do not provide absolute indications for surgery, but should be taken into consideration for Treatment decision making.
Most often, clavicle fractures result from a blow to the shoulder region, such as during a fall to the turf, although they may also result from a direct hit to the collarbone. These fractures are most commonly seen in children and young adults, but are diagnosed with increasing frequency in later decades, when lifestyles are more active, and in the context of the osteoporosis epidemic.
B. Classification. Allman6 classified these fractures according to whether they were proximal, middle, or distal one-third injuries and noted that the middle one-third fracture was by far the most common. Approximately 15% of clavicle fractures are in the distal one-third, 5% in the proximal one-third. The distal one-third clavicle fracture should be distinguished further as to whether it is intraarticular or extraarticular and whether or not it is displaced, which would imply disruption of the coracoclavicular ligaments.2,7
II. DIAGNOSIS
A. History and physical examination. Pain and deformity localized to the clavicle provide the most typical presentation. Frequently, ecchymosis and tenting of the skin are recognized. The typical deformity in the common middle third fracture is caused by the proximal (medial) fragment being pulled by the sternocleidomastoid muscle. The deformity is accentuated by the weight of gravity on the upper extremity pulling downward on the distal (lateral) fragment.
Physical examination will frequently detect bony crepitus and should include inspection of the skin for punctures or lacerations consistent with an open fracture. As the clavicle is directly anterior to the brachial plexus and the subclavian artery, examination should also include neurovascular assessment, particularly in injuries associated with high-energy mechanisms.
B. Radiographs. A standard anteroposterior view of the clavicle usually confirms the diagnosis of a fracture. Adding 15° of tube tilt (caudad for PA; cephalad for AP) aids fracture visualization by limiting surrounding structures in the X-ray field.
Radiographic protocols need to be defined to better describe displacement. At our institution, we use a bilateral panoramic view of both shoulders to measure clavicular shortening (Fig. 14-1). Additionally, supine and upright AP views of the shoulder are obtained to better assess instability (Fig. 14-2). Many times greater displacement and angulation manifest in the upright films; thus, this X-ray is the more relevant position for measurement. Fracture location, degree of comminution, and displacement (both vertical translation and medialization) should be assessed. These factors are used to determine how the patient will be managed. Often, in the setting of polytrauma, a chest X-ray provides the initial radiographic diagnosis. Surrounding structures such as the scapula and ribs should be inspected for injury as well.
Repeat X-rays of the shoulder are warranted on a weekly basis for the first 3 weeks if nonoperative treatment is chosen, because clavicle fractures have a propensity to displace and shorten in the early peri-injury period.8
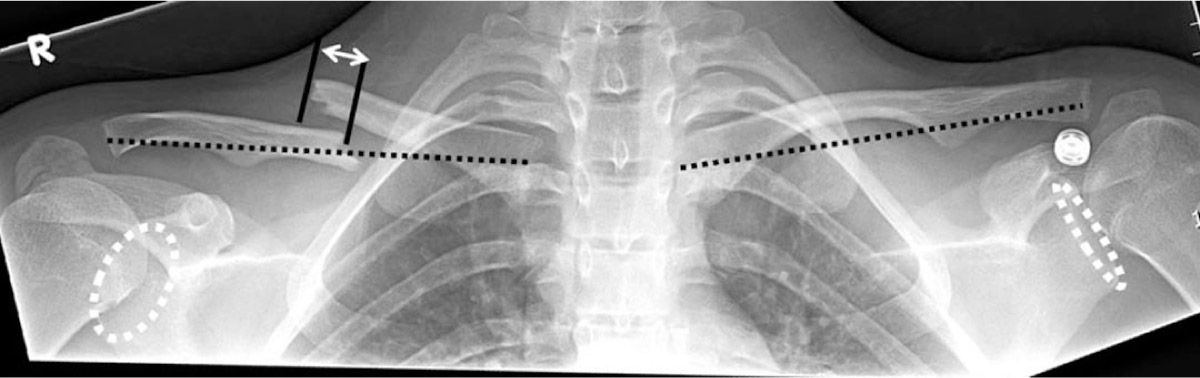
Figure 14-1. Panoramic clavicle view of a midshaft clavicle fracture. Two methods of measuring shortening are illustrated. Measuring the difference in clavicle length has been shown to have a high interreader reliability; however, it is imperative that the X-ray technician ensures proper patient position when taking the X-ray. In this particular view, the lengths of the injured and uninjured clavicle are almost equivalent, while there is clearly enough fragment medialization to consider operative management. Comparing pedicle and glenoid fossa symmetry are helpful in assessing the presence of rotation in the patient or shoulder.
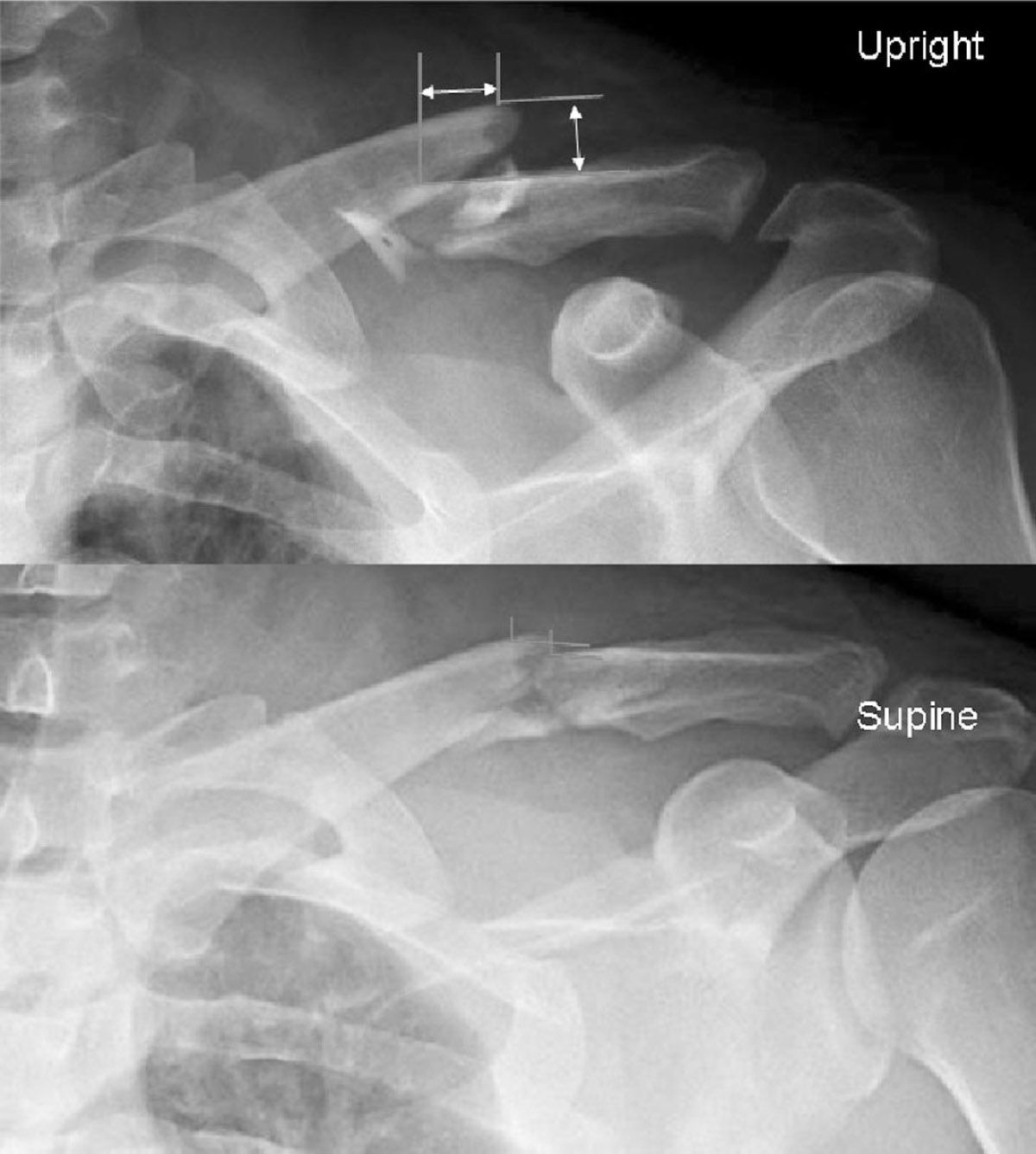
Figure 14-2. A: AP clavicle view with patient upright at the time of X-ray. There is marked medialization and vertical displacement of the clavicle fracture. B:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








