Fig. 7.1
The arches of the hand give it a cup shape, favoring the grips
When the hand is pressed against a support, it can flatten and thus increase the surface of support.
The 2nd and 3rd metacarpals are relatively fixed, whereas the 4th and 5th are mobile, which allows an important adaptability of the ulnar side.
The length of each osseous segment is essential for a harmonious winding of the long fingers, describing an equiangular spiral described by Fibonacci, according to his numerical series [0, 1, 1, 2, 3, 5, 8, 13, 21, 34] (Fig. 7.2).
Fig. 7.2
The winding movement of the fingers describes an equiangular spiral because the lengths of the osseous segments follow the numeric series of Fibonacci, defined by the gold number (1,618, the “divine proportion”)
When the distal interphalangeal joints flex from an extension position, we can observe that the fingers converge toward the thumb, mainly because of the obliquity of the metacarpophalangeal and interphalangeal joints (in a downward and outward direction) (Fig. 7.3).
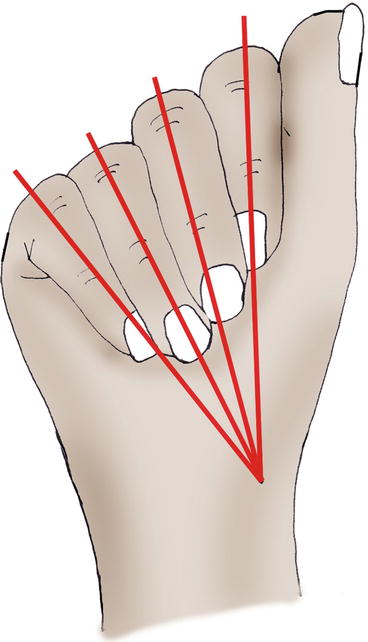
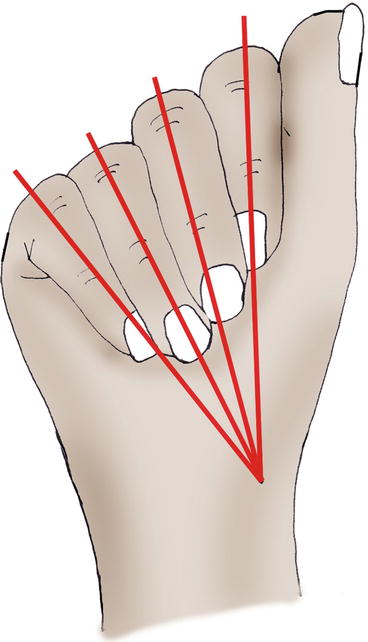
Fig. 7.3
During the winding of the fingers with the distal interphalangeal joint extended, the fingers converge toward the thumb
During the fingers’ opening, the axis of the fingers converges toward the scaphoid tubercle. The axis of the 3rd finger stays still (Fig. 7.4).
Fig. 7.4
When spreading the fingers, the 3rd finger stays still and the axis of the fingers converges toward the scaphoid’s tubercle
7.1.2 Opposition of the Thumb
7.1.2.1 Thumb
The mobility of the thumb depends on the scapho-trapezium, trapeziometacarpal, metacarpophalangeal, and interphalangeal joints.
These four joints, mobilized by the synergic action of the intrinsic and extrinsic muscles of the hand, participate in the opposition of the thumb. This opposition is composed by various actions, a protraction, an abduction, and a pronation, allowing the thumb to oppose its pulp to the long fingers.
This automatic pronation of the thumb is related to osseous (topography of the trapeziometacarpal joint surfaces, radial part of the metacarpophalangeal larger than the ulnar part), ligamentous (radial ligaments longer than the ulnar ones), and muscular (external thenar muscles stronger than the internal thenar muscles during the opposition) factors (Fig. 7.5).
Fig. 7.5
The trapeziometacarpal joint allows automatically associating a pronation during the opposition between the thumb and the fingers, which leads to the pulp of the thumb contacting with the pulp of the finger. The metacarpophalangeal and interphalangeal joints participate too in this automatic rotation, even though they’re less involved
7.1.2.2 Long Fingers
In the long fingers, the opposition between the pulps is allowed by an automatic rotation in supination during the flexion. It’s related to the obliquity of the metacarpophalangeal and interphalangeal joints, the ulnar collateral ligaments longer than the radial collateral ligaments, and the predominant action of the ulnar interosseous muscle (Fig. 7.6).
Fig. 7.6
In the long fingers, the flexion is automatically associated with a supination, to favor the opposition between the pulp of the thumb and the pulp of the fingers
This automatic rotation (and the important anatomical particularities previously described) decreases from the 5th to the 2nd finger, as the segmental movement is more important in the 5th than in the 2nd finger.
7.2 Types of Fractures
7.2.1 Fractures of the Metacarpals [2]
7.2.1.1 Fractures of the Base
Stable and extra-articular fractures don’t present an important risk of secondary displacement, if the treatment is correctly done.
On the contrary, joint fractures are potentially unstable and source of secondary arthrosis.
The fracture of the base of the 5th metacarpal: the radial fragment stays in contact with the base of the 4th metacarpal and the hamate bone, while the extensor carpi ulnaris tends to move the rest of the metacarpal dorsally, proximally, and medially (Fig. 7.7).
Fig. 7.7
In the fractures of the base of the 5th metacarpal, the extensor carpi ulnaris can cause instability of the fracture (left hand on the picture)
The joint fractures in the base of the 2nd and 3rd metacarpals present the same risk of instability, because of the action of the radial muscles.
The joint fractures in the base of the 1st metacarpal can be of two types:
The Bennett fracture, with a medial fragment staying next to the base of the 2nd metacarpal. The rest of the base of the metacarpal moves because of the effect of the abductor pollicis longus. The thenar muscles (mainly the adductor pollicis) tend to move the metacarpal toward adduction (Fig. 7.8).
Figs. 7.8 and 7.8′
Fractures of the base of the thumb, possibly unstable because of the effect of the abductor pollicis brevis and the thenar muscles
The Rolando fracture, which is a fracture with one metaphyseal fracture line and two epiphyseal fracture lines (T-shaped or V-shaped) (Fig. 7.8′).
7.2.1.2 Fractures of the Diaphysis
Long Fingers
These fractures can lead to an anterior tilt of the part distal to the fracture, because of the action of the interossei and flexor muscles (Fig. 7.9).
Fig. 7.9
Anterior tilt of the distal part of the fracture because of the action of the interossei and flexors
Furthermore, the action of the interossei can lead to an axial rotation of the metacarpal, detectable by asking the patient to do a global winding of the fingers. We can then observe a lack of alignment of the metacarpal comparing to the adjacent fingers.
In this type of deformity, the two radial metacarpals are often excessively pronated, whereas the two ulnar metacarpals are more likely to be excessively supinated during the winding (Fig. 7.10).
Fig. 7.10
In fractures of the metacarpal with vicious rotation, the radial metacarpals tend to have an excessive pronation, unlike the ulnar metacarpals
Thumb
We can observe a palmar tilt of the distal part, because of the effect of the expansion made by the flexor pollicis brevis, the abductor pollicis brevis, and the adductor pollicis (Fig. 7.11).
Fig. 7.11
Anterior tilt of the distal fragment in the thumb
7.2.1.3 Boxer’s Fracture
The boxer’s fractures are the most frequently observed, mainly in the 4th and 5th metacarpals. This “bad boxer’s fracture” is due to a punch with an impact on the ulnar side (the “good boxers” usually use the two radial metacarpals that are more fixed), leading to an anterior tilt of the head of the 5th metacarpal.
In that case, like in the fractures of the diaphysis, the dorsal expansion of the interossei (or the thenar muscles – except the opponent – of the thumb) increases the palmar displacement of the metacarpal head.
7.2.1.4 Joint Fractures of the Metacarpal Head
These fractures are a source of stiffness in case of prolonged immobilization and of arthrosis in case of badly reduced displacement, at the level of the thumb or the long fingers.
7.2.2 Fractures of the Phalanges [2–4]
7.2.2.1 Joint Fractures [5, 6]
Joint fractures, like in every other joint, present a risk of stiffness [7] and secondary arthrosis in case of prolonged immobilization and/or bad restoration of the joint surfaces.
We have to be very vigilant because some of these fractures are in fact ligamentous or tendinous injuries, which must be imperatively identified quickly. Here is a list of the most frequent cases (Fig. 7.12).
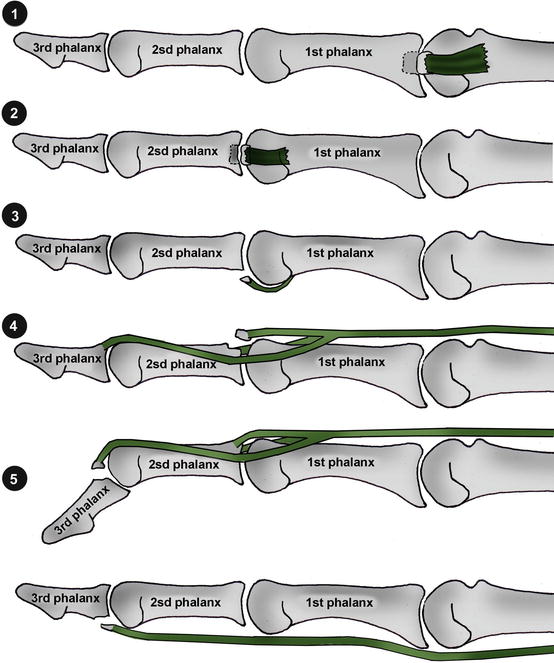
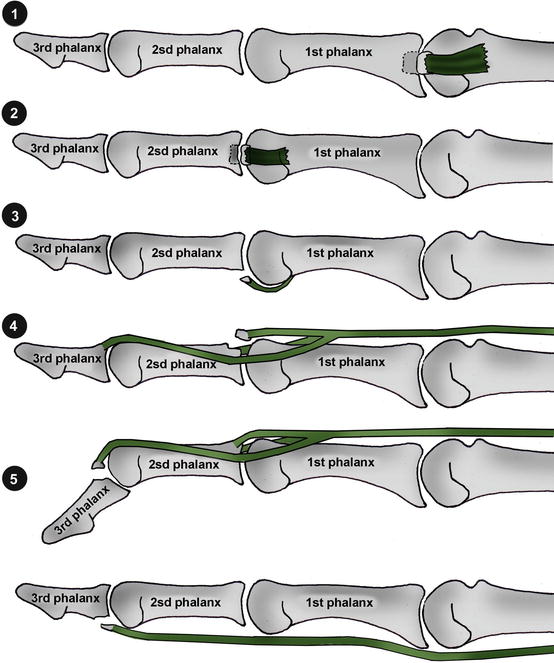
Fig. 7.12
Joint fractures
1. Fracture of the base of the 1st phalanx with lateral fragment; most of the time, it’s a severe sprain of the corresponding collateral ligament
2. Fracture of the base of the 2nd phalanx with lateral fragment; same situation as before
3. Fracture of the base of the 2nd phalanx with palmar fragment; most of the time, it’s a tear of the volar plate of the proximal interphalangeal phalanx (cf. Chap. 8)
4. Fracture of the base of the 2nd phalanx with dorsal fragment; it’s probably a tear of the median strip of the extensor system. It must be treated as such (cf. Chap. 9)
5. Fracture of the base of the 3rd phalanx with dorsal fragment; it is a fracture/tear of the lateral strips (or osseous mallet finger), as seen in the Chap. 9
Fracture of the base of the 3rd finger with palmar fragment; it is a Jersey finger (or rugby finger), where there is a tear of the base of the 3rd phalanx by the flexor digitorum profundus. It’s a surgical emergency (cf. Chap. 10)
7.2.2.2 Fractures of the Diaphysis
First Phalanx
In this kind of fracture, there’s a tendency of palmar displacement of the proximal fragment (because of the dorsal expansion of the interossei) and of dorsal displacement of the distal fragment (because of the extensor system).
Second Phalanx
When the fracture line is proximal to the end of the flexor digitorum superficialis, the proximal fragment is pulled backward by the median strip of the extensor system, and the distal fragment is pulled frontward by the flexor digitorum superficialis.
When the fracture line is distal to the end of the flexor digitorum superficialis, the proximal fragment moves frontward and the distal fragment moves backward.
Third Phalanx
The fractures of the diaphysis of the 3rd phalanx are often the consequence of a crushing trauma, leading to trophic disorders and prolonged pain. They usually don’t cause residual stiffness.
7.3 Therapeutic Process [8]
Our therapeutic process depends on the type of injury. The first priority would be allowing the early mobilization of the damaged finger without disturbing the osseous healing.
7.3.1 Orthopedic Treatment
This treatment is based on the use of thermoformable orthosis, which ideally adapt to the patient’s morphology and leave the unaffected joints free.
7.3.1.1 Allowing Early Mobilization
It’s the treatment that obtains the best results, but it can be used only in stable fractures. The orthosis must allow the osseous healing and at the same time maintain the movements that don’t put excessive constraints on the callus.
The evolution is regularly controlled (by clinical and radiological assessments [9]) to limit the risk of secondary displacements.
7.3.1.2 Immobilization
This is the default choice, when there is a contraindication for surgery and the fracture is displaced or unstable. The orthosis is more constraining and immobilizing in order to improve osseous healing, but it must allow a soft mobilization of the joints that aren’t concerned by the fracture.
7.3.2 Surgical Treatment [10]
Surgical treatment is used in case of displaced fractures with a functional tolerance of 30° of tilt for the fractures of the diaphysis of the 4th or 5th metacarpal and 5° of tilt for the fractures of the diaphysis of the 2nd or 3rd metacarpal.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








