TALUS FRACTURES
- Background: Talus fractures are relatively rare and make up 1% of all foot and ankle fractures. These are generally high-energy injuries.1
- Mechanism. Talar neck fractures occur with hyperdorsiflexion of the ankle. The talar neck impinges against the anterior lip of the tibia and fractures. Historically, this was called “aviator’s astragalus” and was due to upward force of the foot plate when biplanes crashed.
- Examination
- In a displaced neck or body fracture, there is frequently significant swelling, deformity, and tenting of the skin. Depending on the displacement, pressure may be put on the superficial and deep peroneal nerves, or the tibial nerve.
- Imaging
- Anteroposterior (AP), lateral, and mortise views of the ankle are generally adequate to identify talar body, neck, and process fractures. A talar neck fracture is further evaluated with a Canale view. Talar head fractures are better evaluated with AP, lateral, and oblique views of the foot. Computed tomographic (CT) scans are helpful to look at fracture pattern, displacement, and to evaluate articular involvement.
- Classification
- Talar head fractures
- Talar body fractures including talar dome, posterior process, and lateral process
- Process fractures can be easily missed on initial X-rays unless there is a high index of suspicion.
- Talar neck fractures are described by the Hawkins classification2 (Fig. 28-1)
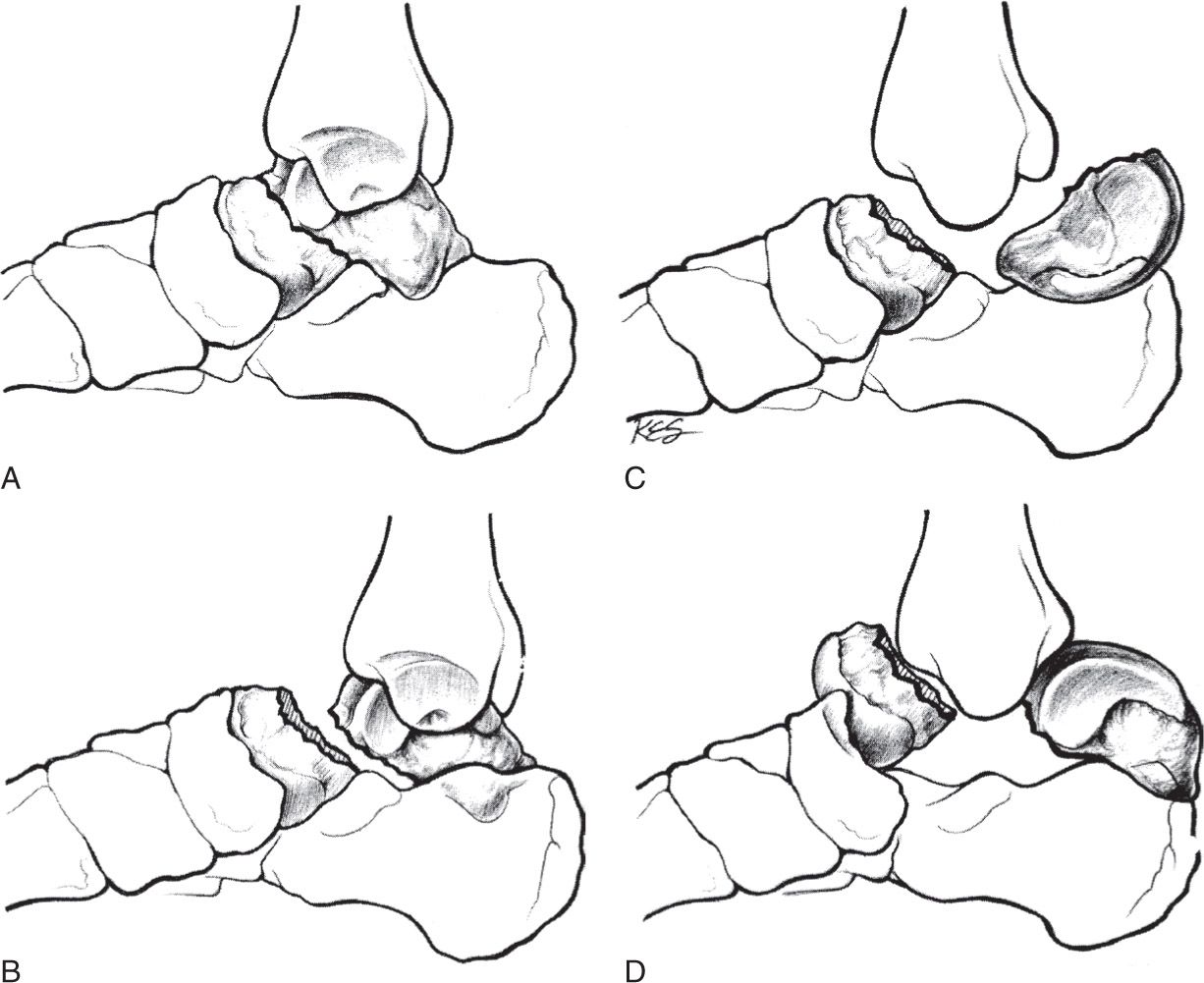
Figure 28-1. Diagrammatic representation of Hawkins classification of talar neck fractures. A: Nondisplaced; B: Displaced with associated subtalar joint subluxation; C: Talar body dislocated from the ankle mortise; D: Talonavicular joint subluxated also. (From Hansen ST, Swiontkowski MF. Orthopaedic Trauma Protocols. New York, NY: Raven; 1993:340, with permission.) (iDams asset name: 75755-27-03)
- Type I: Nondisplaced
- Type II: Displaced fracture with subtalar subluxation/dislocation
- Type III: Displaced fracture with subtalar and ankle subluxations/dislocations
- Type IV: Displaced with subtalar, ankle, and talonavicular joint subluxations/dislocations
- Treatment
- Talar neck fractures with any displacement require open reduction and internal fixation. This can be done through one or two incisions, and with either screws or minifragment plate. Plates are generally used where there is fracture comminution that renders the fracture pattern unstable for compression with lag screws. Displaced fractures with skin tenting require emergent reduction to prevent skin necrosis. Although no studies demonstrate a direct correlation between time to reduction and development of AVN, most surgeons support an “urgent” reduction of talar neck fractures.1
- Talar head, body, and process fractures, if nondisplaced can be treated in a nonweightbearing cast for 6 to 12 weeks, or until healing is demonstrated. Displaced fractures (>2 mm) are generally treated with open reduction with internal fixation (ORIF). Severely comminuted fractures, particularly of the lateral process, may also be treated with primary excision.3
- Complications
- Avascular necrosis (AVN) of the talus is the most devastating complication of talar fractures. The risk of AVN is highest in comminuted body fractures, followed by neck fractures (Type IV with the highest, Type I with the lowest risk).
- Arthritis of the surrounding joints can develop.
SUBTALAR DISLOCATION
- Background: Subtalar dislocation is defined as combined dislocation through the talocalcaneal and talonavicular joints. These are uncommon injuries and make up less than 2% of all large joint dislocations.
- Mechanism: Generally a strong inversion or eversion force results in medial or lateral dislocation, respectively.
- Examination: There is classic positioning of the foot medially or laterally on the ankle with marked tenting of the skin on the side opposite the foot.
- Imaging: AP, lateral, and mortise of the ankle; AP, lateral, and oblique of the foot. CT scan should be obtained postreduction to assess for associated fractures that are common.
- Classification: Described by the location of the foot in relation to the talus: medial, lateral, anterior, or posterior. Medial dislocation is most common (80%) followed by lateral (17%), with very rare dislocations occurring anteriorly or posteriorly.
- Treatment: Emergent reduction. This requires adequate anesthesia. The knee should be flexed to take tension off the gastrocnemius and the foot is then pulled in line with the deformity prior to reversal of the deformity. After reduction, if the joint is stable and no associated displaced fractures are noted, patient can be treated in a nonweightbearing cast or fracture boot for 4 to 6 weeks. Any associated displaced fractures should be treated with ORIF if the fragments are large enough to accept implants. In medial dislocations, reduction may be prevented by interposition of the extensor retinaculum or the extensor digitorum. In lateral dislocations, the posterior tibialis may become entrapped and block reduction.4–6
- Complications: Stiffness, subtalar arthritis
CALCANEUS FRACTURES
- Background: Calcaneal fractures are the most common tarsal bone fracture and account for 1% to 2% of all fractures. These injuries are economically significant in that 90% of them occur in working people, age 20 to 40.
- Mechanism: Intraarticular fractures are generally high energy and result from a fall from height or a motor vehicle accident. The mechanism is generally axial load. Associated injuries include compression fractures of the lumbar spine and occasionally fractures about the knee or pelvis. Avulsion fractures are typically due to a sudden, forceful contraction of the Achilles.
- Examination: Generally the foot is diffusely swollen with lateral and plantar ecchymosis, and widening of the heel. There is pain with palpation of the heel and with attempted hindfoot motion. There may also be pain with ankle or foot motion as well. In open fractures, the wound is most often medial near the sustentaculum tali. Foot compartment syndrome can occur in 2% to 5% of patients and must be treated with urgent decompression. Because of the risk of associated injuries, the spine and pelvis must be thoroughly evaluated.
- Imaging: Initial radiographic evaluation for a suspected calcaneus fracture should include the standard three views of the foot as well as an axial (harris) heel view. Fractures are identified on radiographs by a line of increased (impaction) or decreased bone density or general distortion of the normal shape of the calcaneus. CT scan is then utilized to further clarify the fracture pattern and assess the subtalar joint. Ankle films may be necessary to rule out concomitant injury, and given the association with pelvic and lumbar spine injuries, pelvic and lumbar spine imaging should be a consideration where there is any indication of injury on physical examination.
- Radiographic lines and angles (Fig. 28-2)
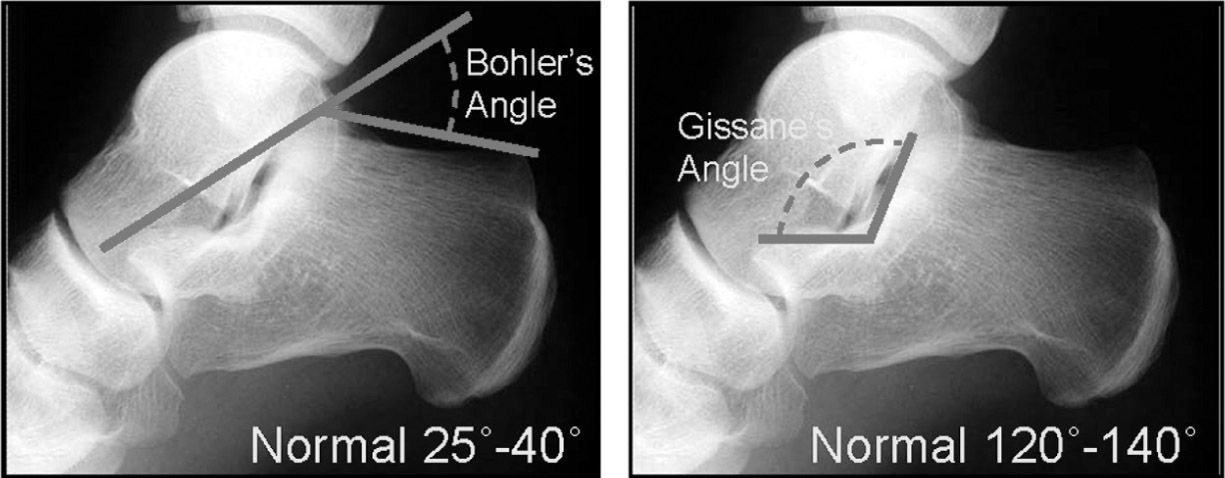
Figure 28-2. Bohler’s angle and Gissane’s angle as seen on the lateral calcaneal view.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








