Forearm Fractures: Open Reduction Internal Fixation
Steven J. Morgan
Indications
The radius and the ulna form a complex articulation that permits elbow, forearm, and wrist motion. Loss of normal angular alignment results in loss of forearm supination and pronation (1,2). Angular deformity in single bone fractures of the forearm with associated soft-tissue injury result in dislocation. Isolated ulna fractures are often referred to as Monteggia fractures and are recognized as having an associated injury or dislocation of the proximal radioulnar joint. Isolated fractures of the radius are accompanied by a distal radioulnar joint (DRUJ) dislocation and are often called a Galeazzi fracture. Open reduction and internal fixation (ORIF) of displaced forearm fractures in the skeletally mature patient remains the standard treatment for displaced forearm fractures. Internal fixation allows for maintenance of fracture alignment during healing while the patient performs functional range of motion with the arm. Outcomes following internal fixation provide better results than nonoperative treatment (3,4,5,6,7,8).
Isolated ulna fractures resulting from a direct blow remain the exception to this general rule. The “night stick” fracture, as it is commonly called, does not have the degree of soft-tissue injury recognized in other fractures of the forearm, and the likelihood of acute instability of the distal or proximal radioulnar articulations is absent. Fractures involving the distal third of the ulna should be evaluated closely and observed carefully over time as angular deformity can result in significant functional impairment at the DRUJ. Operative fixation of isolated ulna fractures, regardless of injury mechanism, is recommended in open fractures, fractures angulated greater then 10 degrees in any plane, and in fractures with greater than 50% comminution (9).
Initial Evaluation, Management, and Surgical Planning
Initial evaluation of the patient and the radiographs is necessary for developing a treatment plan. A detailed history related to mechanism of injury, hand dominance, occupation,
previous injury, and associated medical problems is required. The entire extremity needs to be carefully examined for associated injuries. Circumferential inspection of the extremity should be performed to identify the presence of an open fracture as well as to assess the extent and severity of the soft-tissue injury. Any violation of the skin in reasonable proximity to the fracture should be enough to consider the injury an open fracture. Ecchymosis, fracture blisters, and edema suggest that the soft tissue absorbed significant energy and the index of suspicion for compartment syndrome should be high. Palpation for tenderness and instability should be performed from the shoulder to the hand. The elbow, wrist, and carpal bones should receive special attention.
previous injury, and associated medical problems is required. The entire extremity needs to be carefully examined for associated injuries. Circumferential inspection of the extremity should be performed to identify the presence of an open fracture as well as to assess the extent and severity of the soft-tissue injury. Any violation of the skin in reasonable proximity to the fracture should be enough to consider the injury an open fracture. Ecchymosis, fracture blisters, and edema suggest that the soft tissue absorbed significant energy and the index of suspicion for compartment syndrome should be high. Palpation for tenderness and instability should be performed from the shoulder to the hand. The elbow, wrist, and carpal bones should receive special attention.
Injuries to the DRUJ or proximal radioulnar joint, scaphoid fractures, and carpal instability are common. Neurological examination should be focused and include the motor and sensory status of the radial (posterior interosseous, superficial radial), ulnar, and median nerves. Vascular examination should focus on the perfusion of the extremity and should include palpation of the brachial radial and ulnar pulses.
Initial radiographic evaluation, prior to the application of splinting material, should consist of orthogonal radiographs (AP and lateral) that include both the wrist and the elbow. In situations when the physical examination indicates additional injury or radiographs are inadequate or inspire suspicion that associated injuries exist, joint specific views of the wrist and elbow should be obtained. Radiographic evaluation should never inhibit the overall care of the patient. In the patient with multiple injuries as well as in the patient with soft-tissue injury or neurological or vascular compromise, a provisional reduction and splint should be applied prior to obtaining radiographs. Traction radiographs often facilitate evaluation of comminuted fractures. Difficult to obtain without proper sedation, these radiographs are best obtained following induction of anesthesia prior to surgery. Stress radiographs of the joints for associated instability can also be obtained at this time, and fluoroscopy is often helpful in this regard.
Initial management of the forearm fracture following the physical examination consists of basic open-fracture wound management (if present) and gross realignment and splint immobilization of the forearm to limit pain and further soft-tissue injury while definitive fracture fixation is pending. In cases of marked angulation or vascular compromise, realignment should be performed immediately. In a Monteggia fracture with a dislocated radial head, gentle traction and supination with conscious sedation or regional anesthesia (Bier block) is necessary to reduce the dislocation. In most other situations, adequate analgesia will permit gross realignment and splint application of the forearm. A long-arm posterior splint is preferred. A sugar tong splint, while adequate in many patients, can result in unnecessary skin breakdown in the supracondylar area. Following any manipulation, the neurological and vascular status of the extremity should be reevaluated and documented.
The timing of surgery is largely dependent on the condition of the soft tissues and the general condition of the patient. Internal fixation is warranted on an emergent basis for open fractures, impending or frank compartment syndrome, and irreducible dislocation with impending skin breakdown or neurological deficit. In other situations, the surgery can be performed in a more elective setting. The reduction, however, becomes more difficult with time, and additional soft-tissue dissection may be required to achieve reduction when fracture fixation is delayed beyond 72 hours. Several studies on open fractures have shown no increased morbidity with immediate plate fixation (6,10). Repeat irrigation and debridement are dictated by the severity of the soft-tissue injury and viability following initial plate fixation. In the patient with multisystem trauma and an open forearm fracture, external fixation following irrigation and debridement may be used as a temporizing measure until the patient’s general condition is allowed to improve.
The implant of choice for forearm fracture fixation is a 3.5-mm plate that allows for dynamic compression and application of lag screws through the plate. These implants are available in full contact and limited contact designs. They are available in either titanium or stainless steel from a variety of manufacturers. In theory, low-contact plates limit devitalization of the underlying bone, and titanium decreases the likelihood of stress shielding. Excellent results can be achieved with any of these implant choices. Recently, locked compression plates have been introduced as a fixation option. Their role in diaphyseal fractures of the forearm remains
undefined and to a large extent appears to be unnecessary except in cases of significant osteoporosis (11). In adults, reconstruction and one-third tubular plates are contraindicated.
undefined and to a large extent appears to be unnecessary except in cases of significant osteoporosis (11). In adults, reconstruction and one-third tubular plates are contraindicated.
Implant selection and size, with reasonable variations, should be determined following full evaluation of radiographs and characterization of the fracture pattern. Implant templates are available to aid in this process and should be used liberally. Traditional technique has called for the use of plates that can obtain a minimum of 6 cortices of fixation on either side of the fracture. The use of long plates with spaced screws is also an option. More important, a well thought-out surgical plan should be developed to achieve reduction and fixation. This is paramount when utilizing indirect reduction aids to restore length and alignment.
General Surgical Technique
While regional anesthesia can be utilized in these cases, general anesthesia is preferred so that accurate postoperative assessment of neurological function and evaluation for compartment syndrome can be ensured. The patient is positioned supine and the arm is placed on a radiolucent arm board. Following the induction of anesthesia, a nonsterile tourniquet is applied, and in the case of comminuted fractures, traction radiographs are obtained by applying longitudinal traction to the hand while an assistant or the surgeon applies counter traction in the upper arm.
The extremity is prepped and draped in a standard fashion. In the case of open fractures, the tourniquet is not utilized so that further anoxic injury to the traumatized soft tissue can be avoided. In closed fractures, the limb is exsanguinated and the tourniquet is inflated to 250 psi. Surgical incisions are then drawn on the extremity, and the fracture site is localized with the C-arm and marked. In general, the least comminuted fracture is approached first to aid in the indirect reduction of the other fracture(s). In noncomminuted fractures, the radius is generally approached first. Loop magnification may be utilized for volar forearm dissections to better recognize and control bleeding vessels. Bipolar cautery is utilized when the surgeon is working in close proximity to the nerves, and small ligature clips are utilized liberally during the dissection.
Surgical Approaches
Flexor Carpi Radialis Approach
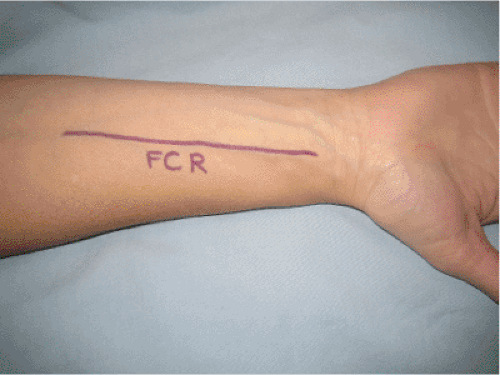
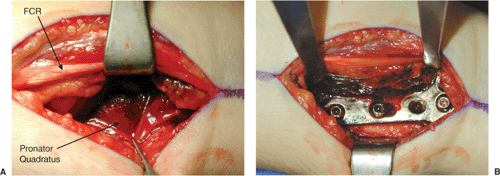
For fractures involving the distal third of the radius, a volar approach based on the flexor carpi radialis (FCR) is utilized. The surgical incision is located just radial to the FCR tendon (Fig. 10.1). Following the skin incision, the FCR tendon sheath is split longitudinally and the FCR tendon is retracted ulnarly. The floor of the tendon sheath is then incised. The flexor pollicis longus (FPL) is then encountered and
retracted ulnarly; this action adds further protection to the median nerve. The pronator quadratus is then incised, elevated from the periosteum, and retracted ulnarly to expose the distal third of the radius (Fig. 10.2). This exposure offers the benefit of avoiding direct dissection of the radial artery, which the FCR sheath protects.
retracted ulnarly; this action adds further protection to the median nerve. The pronator quadratus is then incised, elevated from the periosteum, and retracted ulnarly to expose the distal third of the radius (Fig. 10.2). This exposure offers the benefit of avoiding direct dissection of the radial artery, which the FCR sheath protects.
Volar Approach of Henry
The extensile volar approach of Henry is utilized for most fractures of the proximal radius (12




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree